Fig. 51.2 (a) Sinus bradycardia degenerating into ventricular fibrillation (VF). To the left of the trace a slow sinus heart rate is seen (small P wave before each QRS complex), with a long PR interval (up to 440 ms). After a short period of bradycardia, a very fast tachycardia commences, which initially looks rather like torsade-de-pointes, but very rapidly degenerates into a completely chaotic arrhythmia. This is VF. (b) Successful cardioversion from VF (left of trace) to supraventricular rhythm (right of trace). It is not easy to see whether the supraventricular rhythm is sinus, or slow atrial fibrillation.
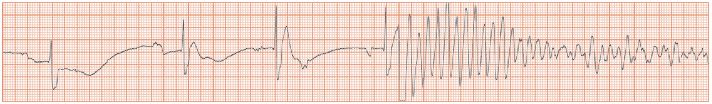
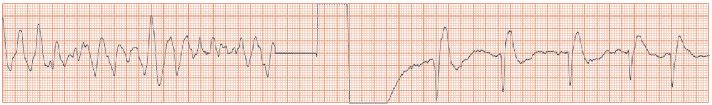
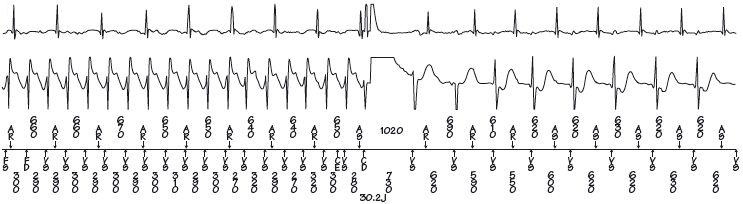
Fig. 51.3 Data from an implantable cardioverter defibrillator (ICD). Here ventricular fibrillation (VF) is terminated by DC shock into sinus rhythm. The top trace shows the intracardiac electrogram from the atrial electrode, the second trace the ventricular one, the final trace shows how beats are labelled and the RR intervals. To the left, the ventricular rate is seen to far exceed the atrial one – so the rhythm is ventricular tachycardia (VT) or VF. The defibrillator is programmed to call all ventricular arrhythmias higher than a certain rate VF and then apply an interval shock (30.2 J in this case). In the trace to the right sinus rhythm is seen, with each P wave being followed after a short interval by an R wave.
Much of cardiology is directed towards preventing death from ventricular fibrillation (VF). To do this one firstly needs to identify which patients are at risk of VF and then intervene to reduce this risk, and secondly to recognize and be able to treat the rhythm disturbance itself.
High-risk patients
Patients with pro-arrhythmic conditions in pro-arrhythmic situations comprise a high-risk population, and include those:
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


