VASCULAR DISEASES OF THE EXTREMITIES
ARTERIAL DISORDERS
PERIPHERAL ARTERY DISEASE
Peripheral artery disease (PAD) is defined as a clinical disorder in which there is a stenosis or occlusion in the aorta or the arteries of the limbs. Atherosclerosis is the leading cause of PAD in patients >40 years old. Other causes include thrombosis, embolism, vasculitis, fibromuscular dysplasia, entrapment, cystic adventitial disease, and trauma. The highest prevalence of atherosclerotic PAD occurs in the sixth and seventh decades of life. As in patients with atherosclerosis of the coronary and cerebral vasculature, there is an increased risk of developing PAD in cigarette smokers and in persons with diabetes mellitus, hypercholesterolemia, hypertension, or hyperhomocysteinemia.
Pathology
(See also Chap. 30) Segmental lesions that cause stenosis or occlusion are usually localized to large and medium-size vessels. The pathology of the lesions includes atherosclerotic plaques with calcium deposition, thinning of the media, patchy destruction of muscle and elastic fibers, fragmentation of the internal elastic lamina, and thrombi composed of platelets and fibrin. The primary sites of involvement are the abdominal aorta and iliac arteries (30% of symptomatic patients), the femoral and popliteal arteries (80–90% of patients), and the more distal vessels, including the tibial and peroneal arteries (40–50% of patients). Atherosclerotic lesions occur preferentially at arterial branch points, which are sites of increased turbulence, altered shear stress, and intimal injury. Involvement of the distal vasculature is most common in elderly individuals and patients with diabetes mellitus.
Clinical evaluation
Fewer than 50% of patients with PAD are symptomatic, although many have a slow or impaired gait. The most common symptom is intermittent claudication, which is defined as a pain, ache, cramp, numbness, or a sense of fatigue in the muscles; it occurs during exercise and is relieved by rest. The site of claudication is distal to the location of the occlusive lesion. For example, buttock, hip, and thigh discomfort occurs in patients with aortoiliac disease, whereas calf claudication develops in patients with femoral-popliteal disease. Symptoms are far more common in the lower than in the upper extremities because of the higher incidence of obstructive lesions in the former region. In patients with severe arterial occlusive disease in whom resting blood flow cannot accommodate basal nutritional needs of the tissues, critical limb ischemia may develop. Patients complain of rest pain or a feeling of cold or numbness in the foot and toes. Frequently, these symptoms occur at night when the legs are horizontal and improve when the legs are in a dependent position. With severe ischemia, rest pain may be persistent.
Important physical findings of PAD include decreased or absent pulses distal to the obstruction, the presence of bruits over the narrowed artery, and muscle atrophy. With more severe disease, hair loss, thickened nails, smooth and shiny skin, reduced skin temperature, and pallor or cyanosis are common physical signs. In patients with critical limb ischemia, ulcers or gangrene may occur. Elevation of the legs and repeated flexing of the calf muscles produce pallor of the soles of the feet, whereas rubor, secondary to reactive hyperemia, may develop when the legs are dependent. The time required for rubor to develop or for the veins in the foot to fill when the patient’s legs are transferred from an elevated to a dependent position is related to the severity of the ischemia and the presence of collateral vessels. Patients with severe ischemia may develop peripheral edema because they keep their legs in a dependent position much of the time. Ischemic neuropathy can result in numbness and hyporeflexia.
Noninvasive testing
The history and physical examination are often sufficient to establish the diagnosis of PAD. An objective assessment of the presence and severity of disease is obtained by noninvasive techniques. Arterial pressure can be recorded noninvasively in the legs by placement of sphygmomanometric cuffs at the ankles and the use of a Doppler device to auscultate or record blood flow from the dorsalis pedis and posterior tibial arteries. Normally, systolic blood pressure in the legs and arms is similar. Indeed, ankle pressure may be slightly higher than arm pressure due to pulse-wave amplification. In the presence of hemodynamically significant stenoses, the systolic blood pressure in the leg is decreased. Thus, the ratio of the ankle and brachial artery pressures (termed the ankle:brachial index, or ABI) is ≥1.0 in normal individuals and <1.0 in patients with PAD; a ratio of <0.5 is consistent with severe ischemia.
Other noninvasive tests include segmental pressure measurements, segmental pulse volume recordings, duplex ultrasonography (which combines B-mode imaging and Doppler flow velocity waveform analysis examination), transcutaneous oximetry, and stress testing (usually using a treadmill). Placement of pneumatic cuffs enables assessment of systolic pressure along the legs. The presence of pressure gradients between sequential cuffs provides evidence of the presence and location of hemodynamically significant stenoses. In addition, the amplitude of the pulse volume contour becomes blunted in the presence of significant PAD. Duplex ultrasonography is used to image and detect stenotic lesions in native arteries and bypass grafts.
Treadmill testing allows the physician to assess functional limitations objectively. Decline of the ABI immediately after exercise provides further support for the diagnosis of PAD in patients with equivocal symptoms and findings on examination.
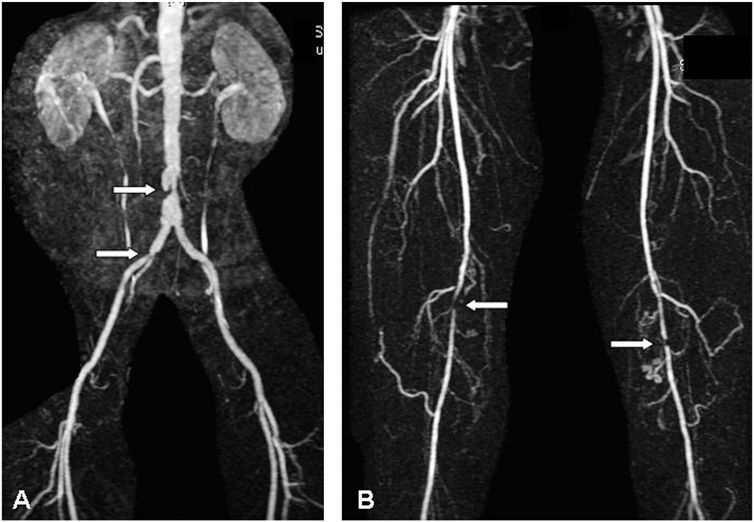
Magnetic resonance angiography (MRA), computed tomographic angiography (CTA), and conventional contrast angiography should not be used for routine diagnostic testing but are performed before potential revascularization (Fig. 39-1). Each test is useful in defining the anatomy to assist planning for catheter-based and surgical revascularization procedures.
FIGURE 39-1
Magnetic resonance angiography of a patient with intermittent claudication, showing stenoses of the distal abdominal aorta and right iliac common iliac artery (A) and stenoses of the right and left superficial femoral arteries (B). (Courtesy of Dr. Edwin Gravereaux; with permission.)
Prognosis
The natural history of patients with PAD is influenced primarily by the extent of coexisting coronary artery and cerebrovascular disease. Approximately one-third to one-half of patients with symptomatic PAD have evidence of coronary artery disease (CAD) based on clinical presentation and electrocardiogram, and over one-half have significant CAD by coronary angiography. Patients with PAD have a 15–30% 5-year mortality rate and a two- to sixfold increased risk of death from coronary heart disease. Mortality rates are highest in those with the most severe PAD. Measurement of ABI is useful for detecting PAD and identifying persons at risk for future atherothrombotic events. The likelihood of symptomatic progression of PAD is lower than the chance of succumbing to CAD. Approximately 75–80% of nondiabetic patients who present with mild to moderate claudication remain symptomatically stable. Deterioration is likely to occur in the remainder, with approximately 1–2% of the group ultimately developing critical limb ischemia each year. Approximately 25–30% of patients with critical limb ischemia undergo amputation within 1 year. The prognosis is worse in patients who continue to smoke cigarettes or have diabetes mellitus.
TREATMENT Peripheral Artery Disease
Patients with PAD should receive therapies to reduce the risk of associated cardiovascular events, such as myocardial infarction and death, and to improve limb symptoms, prevent progression to critical limb ischemia, and preserve limb viability. Risk factor modification and antiplatelet therapy should be initiated to improve cardiovascular outcomes. The importance of discontinuing cigarette smoking cannot be overemphasized. The physician must assume a major role in this lifestyle modification. Counseling and adjunctive drug therapy with the nicotine patch, bupropion, or varenicline increase smoking cessation rates and reduce recidivism. It is important to control blood pressure in hypertensive patients. Angiotensin converting-enzyme inhibitors may reduce the risk of cardiovascular events in patients with symptomatic PAD. β-adrenergic blockers do not worsen claudication and may be used to treat hypertension, especially in patients with coexistent CAD. Treatment of hypercholesterolemia with statins is advocated to reduce the risk of myocardial infarction, stroke, and death. The National Cholesterol Education Program Adult Treatment Panel considers PAD a coronary heart disease equivalent and recommends treatment to reduce low-density lipoprotein (LDL) cholesterol to <100 mg/dL. Platelet inhibitors, including aspirin and clopidogrel, reduce the risk of adverse cardiovascular events in patients with atherosclerosis and are recommended for patients with PAD. Dual antiplatelet therapy with both aspirin and clopidogrel is not more effective than aspirin alone in reducing cardiovascular morbidity and mortality rates in patients with PAD. The anticoagulant warfarin is as effective as antiplatelet therapy in preventing adverse cardiovascular events but causes more major bleeding; therefore, it is not indicated to improve outcomes in patients with chronic PAD.
Therapies for intermittent claudication and critical limb ischemia include supportive measures, medications, nonoperative interventions, and surgery. Supportive measures include meticulous care of the feet, which should be kept clean and protected against excessive drying with moisturizing creams. Well-fitting and protective shoes are advised to reduce trauma. Elastic support hose should be avoided, as it reduces blood flow to the skin. In patients with critical limb ischemia, shock blocks under the head of the bed together with a canopy over the feet may improve perfusion pressure and ameliorate some of the rest pain.
Patients with claudication should be encouraged to exercise regularly and at progressively more strenuous levels. Supervised exercise training programs for 30- to 45-min sessions, three to five times per week for at least 12 weeks, prolong walking distance. Patients also should be advised to walk until nearly maximum claudication discomfort occurs and then rest until the symptoms resolve before resuming ambulation. Pharmacologic treatment of PAD has not been as successful as the medical treatment of CAD (Chap. 33). In particular, vasodilators as a class have not proved to be beneficial. During exercise, peripheral vasodilation occurs distal to sites of significant arterial stenoses. As a result, perfusion pressure falls, often to levels lower than that generated in the interstitial tissue by the exercising muscle. Drugs such as α-adrenergic blocking agents, calcium channel antagonists, papaverine, and other vasodilators have not been shown to be effective in patients with PAD.
Cilostazol, a phosphodiesterase inhibitor with vasodilator and antiplatelet properties, increases claudication distance by 40–60% and improves measures of quality of life. The mechanism of action accounting for its beneficial effects is not known. Pentoxifylline, a substituted xanthine derivative, increases blood flow to the microcirculation and enhances tissue oxygenation. Although several placebo-controlled studies have found that pentoxifylline increases the duration of exercise in patients with claudication, its efficacy has not been confirmed in all clinical trials. Statins appeared promising for treatment of intermittent claudication in initial clinical trials, but more studies are needed to confirm their efficacy. There is no definitive medical therapy for critical limb ischemia, although several studies have suggested that long-term parenteral administration of vasodilator prostaglandins decreases pain and facilitates healing of ulcers. Clinical trials of angiogenic growth factors are proceeding. Intramuscular gene transfer of DNA encoding vascular endothelial growth factor, fibroblast growth factor, hepatocyte growth factor, or hypoxia-inducible factor 1α, as well as administration of endothelial progenitor cells, may promote collateral blood vessel growth in patients with critical limb ischemia. Some trial results have been negative, and others encouraging. The outcome of ongoing studies will further elucidate the potential role of therapeutic angiogenesis for PAD.
REVASCULARIZATION Revascularization procedures, including catheter-based and surgical interventions, are usually indicated for patients with disabling, progressive, or severe symptoms of intermittent claudication despite medical therapy and for those with critical limb ischemia. MRA, CTA, or conventional contrast angiography should be performed to assess vascular anatomy in patients who are being considered for revascularization. Nonoperative interventions include percutaneous transluminal angiography (PTA), stent placement, and atherectomy (Chap. 36). PTA and stenting of the iliac artery are associated with higher success rates than are PTA and stenting of the femoral and popliteal arteries. Approximately 90–95% of iliac PTAs are initially successful, and the 3-year patency rate is >75%. Patency rates may be higher if a stent is placed in the iliac artery. The initial success rates for femoral-popliteal PTA and stenting are approximately 80%, with 60% 3-year patency rates. Patency rates are influenced by the severity of pretreatment stenoses; the prognosis of occlusive lesions is worse than that of nonocclusive stenotic lesions. The role of drug-eluting stents in PAD is under investigation.
Several operative procedures are available for treating patients with aortoiliac and femoral-popliteal artery disease. The preferred operative procedure depends on the location and extent of the obstruction(s) and the general medical condition of the patient. Operative procedures for aortoiliac disease include aortobifemoral bypass, axillofemoral bypass, femoro-femoral bypass, and aortoiliac endarterectomy. The most frequently used procedure is the aortobifemoral bypass using knitted Dacron grafts. Immediate graft patency approaches 99%, and 5- and 10-year graft patency in survivors is >90% and 80%, respectively. Operative complications include myocardial infarction and stroke, infection of the graft, peripheral embolization, and sexual dysfunction from interruption of autonomic nerves in the pelvis. The operative mortality rate ranges from 1–3%, mostly due to ischemic heart disease.
Operative therapy for femoral-popliteal artery disease includes in situ and reverse autogenous saphenous vein bypass grafts, placement of polytetrafluoroethylene (PTFE) or other synthetic grafts, and thromboendarterectomy. The operative mortality rate ranges from 1–3%. The long-term patency rate depends on the type of graft used, the location of the distal anastomosis, and the patency of runoff vessels beyond the anastomosis. Patency rates of femoral-popliteal saphenous vein bypass grafts approach 90% at 1 year and 70–80% at 5 years. Five-year patency rates of infrapopliteal saphenous vein bypass grafts are 60–70%. In contrast, 5-year patency rates of infrapopliteal PTFE grafts are <30%. Lumbar sympathectomy alone or as an adjunct to aortofemoral reconstruction has fallen into disfavor.
Preoperative cardiac risk assessment may identify individuals who are especially likely to experience an adverse cardiac event during the perioperative period. Patients with angina, prior myocardial infarction, ventricular ectopy, heart failure, or diabetes are among those at increased risk. Stress testing with treadmill exercise (if feasible), radionuclide myocardial perfusion imaging, or echocardiography permits further stratification of patient risk (Chap. 36). Patients with abnormal test results require close supervision and adjunctive management with anti-ischemic medications. β-adrenergic blockers and statins reduce the risk of postoperative cardiovascular complications. Coronary angiography and coronary artery revascularization compared with optimal medical therapy do not improve outcomes in most patients undergoing peripheral vascular surgery, but cardiac catheterization should be considered in patients with unstable angina and angina refractory to medical therapy as well as those suspected of having left main or three-vessel CAD.
FIBROMUSCULAR DYSPLASIA
Fibromuscular dysplasia is a hyperplastic disorder that affects medium-size and small arteries. It occurs predominantly in females and usually involves the renal and carotid arteries but can affect extremity vessels such as the iliac and subclavian arteries. The histologic classification includes intimal fibroplasia, medial dysplasia, and adventitial hyperplasia. Medial dysplasia is subdivided into medial fibroplasia, perimedial fibroplasia, and medial hyperplasia. Medial fibroplasia is the most common type and is characterized by alternating areas of thinned media and fibromuscular ridges. The internal elastic lamina usually is preserved. The iliac arteries are the limb arteries most likely to be affected by fibromuscular dysplasia. It is identified angiographically by a “string of beads” appearance caused by thickened fibromuscular ridges contiguous with thin, less-involved portions of the arterial wall. When limb vessels are involved, clinical manifestations are similar to those for atherosclerosis, including claudication and rest pain. PTA and surgical reconstruction have been beneficial in patients with debilitating symptoms or threatened limbs.
THROMBOANGIITIS OBLITERANS
Thromboangiitis obliterans (Buerger’s disease) is an inflammatory occlusive vascular disorder involving small and medium-size arteries and veins in the distal upper and lower extremities. Cerebral, visceral, and coronary vessels may be affected rarely. This disorder develops most frequently in men <40 years of age. The prevalence is higher in Asians and individuals of Eastern European descent. Although the cause of thromboangiitis obliterans is not known, there is a definite relationship to cigarette smoking in patients with this disorder.
In the initial stages of thromboangiitis obliterans, polymorphonuclear leukocytes infiltrate the walls of the small and medium-size arteries and veins. The internal elastic lamina is preserved, and a cellular, inflammatory thrombus develops in the vascular lumen. As the disease progresses, mononuclear cells, fibroblasts, and giant cells replace the neutrophils. Later stages are characterized by perivascular fibrosis, organized thrombus, and recanalization.
The clinical features of thromboangiitis obliterans often include a triad of claudication of the affected extremity, Raynaud’s phenomenon, and migratory superficial vein thrombophlebitis. Claudication usually is confined to the calves and feet or the forearms and hands because this disorder primarily affects distal vessels. In the presence of severe digital ischemia, trophic nail changes, painful ulcerations, and gangrene may develop at the tips of the fingers or toes. The physical examination shows normal brachial and popliteal pulses but reduced or absent radial, ulnar, and/or tibial pulses. Arteriography is helpful in making the diagnosis. Smooth, tapering segmental lesions in the distal vessels are characteristic, as are collateral vessels at sites of vascular occlusion. Proximal atherosclerotic disease is usually absent. The diagnosis can be confirmed by excisional biopsy and pathologic examination of an involved vessel.
There is no specific treatment except abstention from tobacco. The prognosis is worse in individuals who continue to smoke, but results are discouraging even in those who stop smoking. Arterial bypass of the larger vessels may be used in selected instances, as well as local debridement, depending on the symptoms and severity of ischemia. Antibiotics may be useful; anticoagulants and glucocorticoids are not helpful. If these measures fail, amputation may be required.
VASCULITIS
Other vasculitides may affect the arteries that supply the upper and lower extremities.
ACUTE ARTERIAL OCCLUSION
Acute arterial occlusion results in the sudden cessation of blood flow to an extremity. The severity of ischemia and the viability of the extremity depend on the location and extent of the occlusion and the presence and subsequent development of collateral blood vessels. There are two principal causes of acute arterial occlusion: embolism and thrombus in situ.
The most common sources of arterial emboli are the heart, aorta, and large arteries. Cardiac disorders that cause thromboembolism include atrial fibrillation, both chronic and paroxysmal; acute myocardial infarction; ventricular aneurysm; cardiomyopathy; infectious and marantic endocarditis; thrombi associated with prosthetic heart valves; and atrial myxoma. Emboli to the distal vessels may also originate from proximal sites of atherosclerosis and aneurysms of the aorta and large vessels. Less frequently, an arterial occlusion results paradoxically from a venous thrombus that has entered the systemic circulation via a patent foramen ovale or another septal defect. Arterial emboli tend to lodge at vessel bifurcations because the vessel caliber decreases at those sites; in the lower extremities, emboli lodge most frequently in the femoral artery, followed by the iliac artery, aorta, and popliteal and tibioperoneal arteries.
Acute arterial thrombosis in situ occurs most frequently in atherosclerotic vessels at the site of an atherosclerotic plaque or aneurysm and in arterial bypass grafts. Trauma to an artery may also result in the formation of an acute arterial thrombus. Arterial occlusion may complicate arterial punctures and placement of catheters; it also may result from arterial dissection if the intimal flap obstructs the artery. Less common causes include thoracic outlet compression syndrome, which causes subclavian artery occlusion, and entrapment of the popliteal artery by abnormal placement of the medial head of the gastrocnemius muscle. Polycythemia and hypercoagulable disorders are also associated with acute arterial thrombosis.
Clinical features
The symptoms of an acute arterial occlusion depend on the location, duration, and severity of the obstruction. Often, severe pain, paresthesia, numbness, and coldness develop in the involved extremity within 1 h. Paralysis may occur with severe and persistent ischemia. Physical findings include loss of pulses distal to the occlusion, cyanosis or pallor, mottling, decreased skin temperature, muscle stiffening, loss of sensation, weakness, and/or absent deep tendon reflexes. If acute arterial occlusion occurs in the presence of an adequate collateral circulation, as is often the case in acute graft occlusion, the symptoms and findings may be less impressive. In this situation, the patient complains about an abrupt decrease in the distance walked before claudication occurs or of modest pain and paresthesia. Pallor and coolness are evident, but sensory and motor functions generally are preserved. The diagnosis of acute arterial occlusion is usually apparent from the clinical presentation. In most circumstances, MRA, CTA, or catheter-based arteriography is used to confirm the diagnosis and demonstrate the location and extent of occlusion.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree