Uterine Contraction Monitoring
In discussions on the benefits of fetal monitoring, uterine contraction monitoring is most often ignored. The initial development of fetal heart rate (FHR) monitoring was concerned with the assessment of fetal status. Contraction patterns were included so that the various decelerative patterns could be timed in relation to contractions. With the use of monitors in labor, however, it became apparent that one principal benefit of such routine monitoring was the data it provided relative to uterine activity.
Uterine activity may be assumed to be adequate if progress in labor, as defined by progressive cervical dilatation and descent, is occurring. Failure to progress in labor may be due to inadequate uterine contractions. On the other hand, excessive uterine activity, as in abruptio placentae, may cause inadequate placental perfusion, and thus give rise to fetal hypoxia and acidosis. When it is necessary to induce or augment labor, the clinician must be aware of uterine activity, as overstimulation could lead to fetal compromise or even uterine rupture.
Manual palpation has been the traditional method of monitoring uterine contractions in labor. This method can be used to identify contraction frequency and duration, but it can measure intensity only relatively. It is time-consuming, requires constant evaluation, and provides no permanent record. The effort can be tedious at best, and what occurs in most cases is intermittent manual palpation for short intervals. The contraction monitor provides a tool that significantly improves the accurate monitoring of uterine contractions.
PHYSIOLOGY OF UTERINE CONTRACTIONS
Uterine contractions have as a primary function the expulsion of the intrauterine contents. Uterine activity before the onset of active labor may prepare the uterus and cervix for labor. The uterus is a smooth muscle organ that, during pregnancy, is progressively stretched. Contractions may be a physiologic response to this stretch, perhaps dampened by mechanisms that normally inhibit the premature onset of labor. Two types of preparatory contractions have been described by Caldeyro-Barcia and Poseiro (1). The first are small, weak contractions of short duration, localized to isolated areas of the uterus occurring about once a minute. These highfrequency, low-intensity contractions begin in early pregnancy and seem to disappear near term. They may be related to or may be the same as the localized periodic thickening of the uterine wall frequently seen on routine ultrasound during early gestation (2,3). The second are the better-known Braxton Hicks contractions. These have a higher magnitude of strength (10 to 20 mm Hg), are more generalized, and have a frequency that increases from one contraction per hour at 30 weeks to as often as every 5 to 10 minutes at term. This background frequency is greater with multiple gestations and the vast majority of the time is not perceived by the patient (4). The transition into the regular rhythmical contractions of labor may be insidious or abrupt, and the exact control of this transition remains unknown.
Contractions can be described by frequency, duration, strength (amplitude), uniformity, and shape. During normal labor, the amplitude of contractions increases from an average of 30 mm Hg in early labor to 50 mm Hg in later first stage and 50 to 80 mm Hg during the second stage. The uterus is not a flaccid sac but has baseline tone. At and near term, this baseline tone is generally 8 to 12 mm Hg, with values in excess of 25 mm Hg defined as hypertonus (or, redundantly, baseline hypertonus). The smaller nonpregnant uterus will generate very strong uterine contractions because, according to the law of Laplace, at a given amount of uterine wall tension, the amount of intracavitary pressure is inversely proportional to the radius of the cavity. This is true for the uterus only to a point, however. With excessively large volumes, as in polyhydramnios, uterine tone may begin to rise because of excessive stretching of the muscle fibers (5).
Once actual labor begins, contractions generally become more frequent, coordinated, and stronger. The propagation of uterine contractions is the result of pacemaker-like activity originating usually from the area of the uterotubal junction. For the contraction to fulfill its purpose most efficiently (i.e., expulsion of the fetus via cervical dilation and fetal descent), the contraction must start in the fundus and progressively propagate toward the cervix. Reynolds et al. (6) described this as “fundal dominance,” which, simply stated, means that, because of the lesser curvature at the fundus and the greater muscle mass, the strength of contractions is greatest at the fundus and least at the cervix. Caldeyro-Barcia and Poseiro (1) further refined this description. They described a triple descending gradient of wave propagation, intensity, and duration, such that the origin of the contraction is in the fundus and the direction of the contractile wave is toward the cervix. Not only is the contraction more intense in the fundus, but the duration of the contraction is progressively shorter from the fundus to midcorpus to cervix.
MONITORING OF UTERINE ACTIVITY
External Monitoring
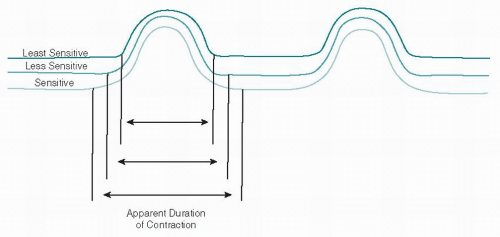
Contractions are most conveniently monitored externally with a tocodynamometer. Mechanical devices for monitoring contractions externally were introduced as early as 1861. Murphy (7) described a ring tocodynamometer and, subsequently, Reynolds et al. (8) used three such instruments on various portions of the uterus to describe normal contraction physiology. The tocodynamometer or “toco” is essentially a weight with a centrally placed pressure-sensitive surface secured to the abdominal wall with a strap (Fig. 5.1). The toco is positioned near the fundus and adjusted to a position that results in the best contraction recording. A sensitivity calibration device, present either on the toco or, more commonly, on the monitor itself, is adjusted to place the resting pressure at 15 to 20 mm Hg to obtain the best tracing. It must always be remembered that the contraction strength is only relatively accurate and varies greatly with maternal position, body habitus, and the tightness of the belt. These factors also affect the sensitivity of the recording. The duration of the contraction will appear to vary: The more sensitive the toco, the longer the apparent duration (Fig. 5.2). With external contraction monitoring, frequency is most accurately, duration less accurately, and intensity least accurately recorded.
The external technique has the advantage of being noninvasive, thus being applicable for patients with intact membranes, that is, the antepartum patient, the patient in premature labor, or the patient during the intrapartum period. There are, however, disadvantages. Patient mobility is limited. Often, the best tracings are obtained with the patient supine. Generally, external monitors are more
uncomfortable for the patient. Some patients generate poor to nonexistent tracings of uterine activity. The limitations with regard to intensity and duration have been discussed. At times, when FHR patterns of concern occur and maternal position is changed, loss of a previously good contraction tracing results, thus making FHR decelerations difficult to time or even record due to loss of signal.
uncomfortable for the patient. Some patients generate poor to nonexistent tracings of uterine activity. The limitations with regard to intensity and duration have been discussed. At times, when FHR patterns of concern occur and maternal position is changed, loss of a previously good contraction tracing results, thus making FHR decelerations difficult to time or even record due to loss of signal.
Internal Monitoring
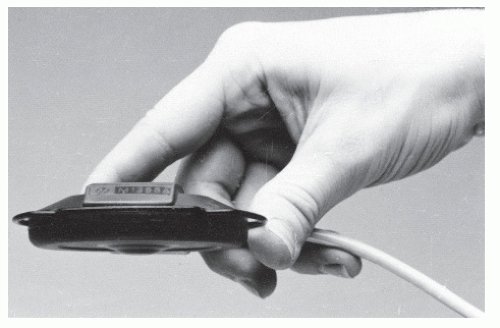
According to the law of Pascal, pressure within a fluid-filled closed spheroid is equal at all points. This describes the uterus quite well; therefore, the pregnant uterus is ideal for contraction pressure monitoring. As reported by Williams and Stallworthy (9), as early as 1872 Schatz had used a hydrostatic bag in the lower uterine segment for pressure recording after the membranes had ruptured. In 1927, Bourne and Burn (10) used the hydrostatic bag extraovularly (between the membranes and the lower uterine segment). Alvarez and Caldeyro-Barcia (11) described a transabdominal technique for inserting open fluid-filled catheters in the amniotic cavity to record contractions. Other techniques, including electrohysterography and intramyometrial pressure recording, have been reported. In 1952, Williams and Stallworthy (9) suggested the use of a Drew-Smythe metal cannula (originally designed for high amniotomy) as a guide to introduce a polyethylene tubing transcervically into the amniotic cavity. This was the forerunner for the technique now commonly used for internal contraction monitoring. Currently, sterile disposable kits are available with flexible plastic catheters containing a pressure-sensing device located in the catheter tip (Figs. 5.3 and 5.4). The details of insertion, instrumentation,
and calibration are described in Chapter 4. This method can be used to define and record accurately the frequency, duration, strength, and tonus of the uterus and its contraction. It is less confining and more comfortable for the patient and is generally unaffected by maternal position.
and calibration are described in Chapter 4. This method can be used to define and record accurately the frequency, duration, strength, and tonus of the uterus and its contraction. It is less confining and more comfortable for the patient and is generally unaffected by maternal position.
 Figure 5.3. Internal pressure catheter with pressure-sensing device in tip. There is no need to fill the catheter with fluid when using this technology (Tyco Healthcare-Kendall LTP, Chicopee, MA).
Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|