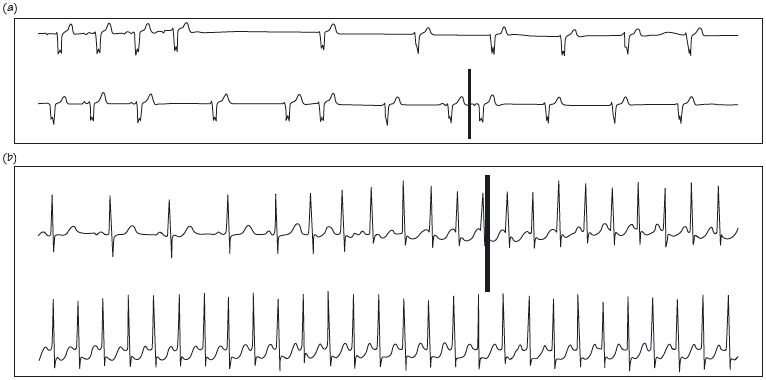
Fig. 63.2 (a) Print out from the time a patient was ‘dizzy’. Sinus rhythm gives way to a narrow complex bradycardia without preceding P waves. This is sinus arrest due to sick sinus syndrome, with junctional escape beats. (b) Supraventricular tachycardia (SVT). Sinus rhythm gives way to a narrow complex tachycardia, with increasing ST depression over time. In both traces the bold upright bar is the patient activated marker, indicating symptoms.
Twenty-four hour ECGs (Holter monitors, after Norman J. Holter) are an indispensable part of modern cardiology practice. Subjects are connected (using 3–5 ECG electrodes attached in a non-standard position called CM5, Fig. 63.1c) for 24 h to a device that records all cardiac electrical activity, the Holter monitor. During this time subjects undertake their usual day-to-day activities. One to three ECG channels are stored in the solid-state memory and analysed after the recording. Patients push a button to mark when symptoms occur. The Holter monitor is useful for determining:
- Heart rhythm, especially to determine whether an arrhythmia underlies symptoms (e.g. palpitations, breathlessness, chest pain, dizzy spells or syncope). This is the main clinical use of the Holter.
- Arrhythmia status, a clue to the presence of disease and/or its prognosis:
(a) Frequent/complex ventricular premature contractions (VPCs) may indicate left ventricular (LV) (rarely right ventricular [RV]) dysfunction, though these can occur in normal hearts (see Chapter 47). Ventricular ectopics are classified according to their frequency and complexity using the Lown grading system (Table 63.1).
(b) Non-sustained ventricular tachycardia (NSVT) has prognostic significance in post-myocardial infarction (MI) -impaired LV function.
(c) In extensive conducting tissue disease (e.g. bi- or tri-fascicular block etc.) episodic second/third degree heart block may indicate the need for a permanent pacemaker.
- Heart rate: particularly in atrial fibrillation (AF) to ensure optimal heart rate control, but also in diagnosing ‘unfitness’ (high resting heart rates/brisk increases with effort), or sick sinus syndrome.
- Heart rate variability (HRV), a surprisingly little used function of the Holter monitor.
- Post-MI risk stratification: by determining average heart rate (the lower the better), occult arrhythmias (especially NSVT) and HRV (the higher the better).
- Ischaemic burden; the amount/duration of ST depression (even if not associated with angina) in ishaemic heart disease (IHD) is a prognostically important and relevant target for intervention.
- QT intervals: the Holter monitor is helpful in this specialized field, giving data on:
(a) Absolute QT interval data, i.e. is the QT interval prolonged?
(b) QT interval variability, i.e. how the QT interval changes with heart rate, and how it is affected by the circadian rhythm (normal subjects have longer QT intervals at night than daytime at any given heart rate).
How to read a Holter monitor report
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


