Troubleshooting and Problem Solving
Learning Objectives
On completion of this chapter, the reader will be able to do the following:
3 Determine the cause of a problem using a graphic from a patient-ventilator system.
4 Assess a description of a patient situation and recommend a solution.
5 Describe the signs and symptoms associated with patient-ventilator asynchrony.
9 Identify the causes and potential problems related to electrolyte imbalances and their causes.
10 Recognize the signs and symptoms of a respiratory infection.
12 Recognize the presence of auto-PEEP using ventilator graphics.
15 Use a ventilator flow-volume loop to assess a patient’s response to bronchodilator therapy.
Key Terms
• Ascites
• Asynchrony (Dyssynchrony)
• Problem
• Pulmonary angiogram
• Thrombolytic therapy
Troubleshooting, in the context of mechanical ventilation, involves the identification and resolution of technical malfunctions in the patient-ventilator system. Troubleshooting can be thought of as purposeful resolution of inappropriate and potentially dangerous situations.
Previous chapters have reviewed key concepts used in the management of patients receiving mechanical ventilation. This chapter discusses common technical problems encountered during mechanical ventilation and presents basic problem-solving strategies to ensure patient safety.
Definition of the Term Problem
A problem can be defined as a situation in which a person finds discord or is uncomfortable with a matter that cannot be immediately resolved. Interestingly, a situation that might be uncomfortable for one person may not appear to be a problem for another person. For example, a respiratory therapist in the intensive (ICU) may note that audible and visual alarms have activated for the intravenous pump. Unless it is part of this person’s job function, the respiratory therapist might not perceive this as a problem that must be resolved and may simply contact the nurse. In contrast, if a ventilator alarm is activated, the same respiratory therapist would accept the responsibility of going to the patient’s bedside to assess the situation and finding a solution to the problem. Individuals therefore must perceive an event as a problem and want to find a meaningful solution; that is, a situation must create discomfort which forces someone perceiving it to take action toward a resolution.
The ability to define a problem is particularly important to health care practitioners. The lives of patients receiving ventilatory support may ultimately depend on the mechanical ventilator. Indeed, a matter of minutes can mean life or death. Because potential mishaps can occur with the patient-ventilator system, it is essential that clinicians develop the ability to identify and correct associated problems.
Solving Ventilation Problems
The first step in solving any problem is to assess the situation at hand carefully. The next step is to gather and analyze pertinent data, which should point to a number of viable solutions.
When a solution is attempted, the clinician’s observations of the patient’s response are critical. If the response is positive and leads to the correct remedy, the problem is resolved. If not, the clinician must undo what was attempted and try to determine the reason the particular solution failed before attempting another approach. If the problem cannot be resolved, the clinician should seek help.
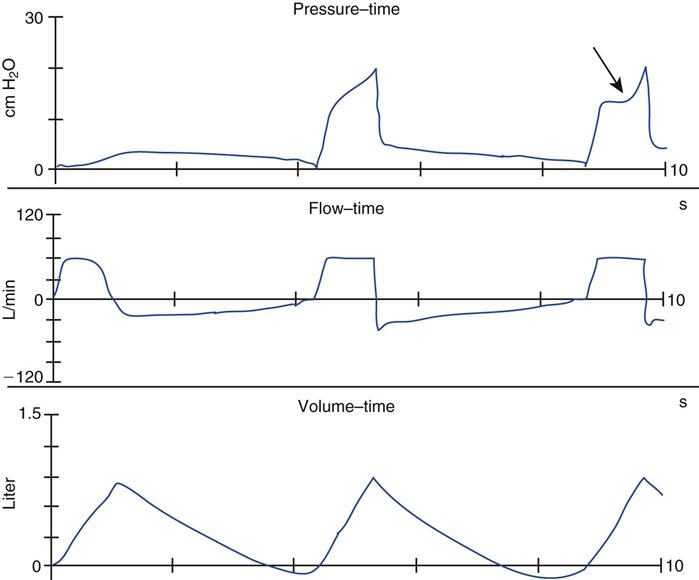
Determining the cause of the problem can help prevent its recurrence. Note the steps taken in Box 18-1 to solve the problem shown in Fig. 18-1. Which individual or individuals first perceived it as a problem? What steps were taken to determine the cause? What was the final resolution?
The volume delivered by the ventilator (the inspiratory portion of the volume curve) is smaller than the volume exhaled, possibly because the patient is actively exhaling. A patient evaluation reveals that this is not the case.
The respiratory therapist, unable to explain the cause immediately, uses a respirometer to measure the volume coming from the volume delivery port, the patient, and the exhalation valve. The three volumes are equal. Still unable to determine the cause, the respiratory therapist contacts the individual who performs the maintenance checks on the ventilator. The respiratory therapist learns that the expiratory transducer was calibrated for a heated humidifier; however, a heat and moisture exchanger (HME) is being used with this patient. Although recalibrating the transducer would resolve the issue, it is not a life-threatening situation, and therefore no immediate action is required.
Protecting The Patient
It is important to understand that ensuring patient safety is the foremost obligation of the clinician. Whenever an alarm activates on a ventilator or monitoring device, the clinician should first make sure that the patient is adequately ventilated and oxygenated. Initially, this can be accomplished by visually assessing the patient’s level of consciousness, use of accessory muscles, and chest wall movements. During this initial assessment, the alarm should be checked and silenced. Auscultation of the chest can establish the presence of adequate breath sounds, and checking the SpO2 can provide information about the patient’s heart rate and oxygen saturation. If the patient is in acute distress, with labored breathing, pallor, diaphoresis, and apparent anxiety, along with deterioration of breath sounds and a decreasing SpO2, immediate action is required. When a serious problem is detected, the patient may need to be disconnected from the ventilator and manually ventilated with a resuscitation bag. (When the patient is safe and in stable condition, the clinician can review the cause of the alarm activation and obtain help from other personnel if necessary.)
A resuscitation bag can be used temporarily for ventilation in a patient. When it is used properly, the resuscitation bag allow for the assessment of lung characteristics because the clinician can check (“feel”) a patient’s lung and chest-wall compliance and airway resistance manually. Manual ventilation must be performed cautiously to avoid inappropriate patterns of ventilation, excessive pressures (i.e., >40 cm H2O), and barotrauma.1,2 Additionally, ventilator disconnection of a patient with ARDS who is ventilated with a high level of PEEP (15-25 cm H2O) can cause derecruitment of the lung, resulting in desaturation. Manual ventilation must also be used judiciously because disconnecting the patient from the ventilator can also result in contamination of the patient’s airway, which in turn can increase the patient’s risk of developing ventilator-associated pneumonia (see Chapter 14).
Identifying The Patient In Sudden Distress
The term patient-ventilator asynchrony is typically used to describe the phenomenon that occurs when patients are unable to breathe comfortably with the mechanical ventilator. The phrase “fighting the ventilator” is sometimes used to describe a individual who is apparently doing well while receiving mechanical ventilation but suddenly develops acute respiratory distress.3,4 This situation is particularly challenging for most clinicians because the patient is unable to verbalize his or her discomfort (Key Point 18-1). (Sometimes clinicians can gain valuable information from patients simply by asking direct [“yes” or “no”] questions.5)
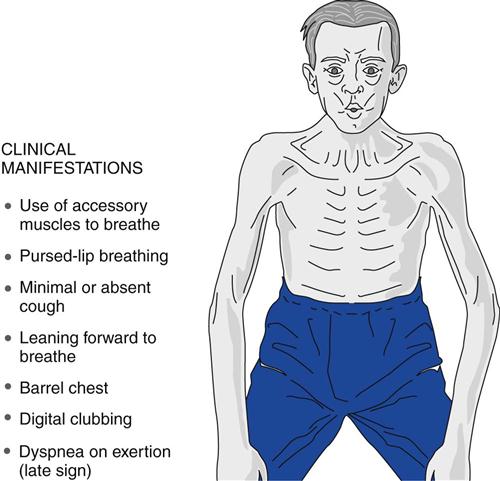
The sudden onset of dyspnea can be identified by observing the physical signs of distress (Fig. 18-2), including tachypnea; nasal flaring; diaphoresis; accessory muscle use; retraction of the suprasternal, supraclavicular, and intercostal spaces; paradoxical or abnormal movement of the thorax and abdomen; abnormal findings on auscultation; tachycardia; arrhythmia; and hypotension.3,4 Pulse oximetry, capnograph readings, ventilator graphics, peak inspiratory pressure (PIP), plateau pressure (Pplateau), and exhaled volumes may have changed and may provide information to help identify the cause of the problem.
Patient-ventilator asynchrony (dyssynchrony) can be caused by a number of factors. Box 18-2 lists the most common causes of sudden respiratory distress in patients receiving mechanical ventilation. (See the section in Chapter 17 on steps to reduce the work of breathing [WOB] during mechanical ventilation.)
Evaluation of the ventilator graphics and settings can be used to resolve most of these problems. For example, autotriggering of breaths can occur if the sensitivity setting (inspiratory trigger) is too sensitive, resulting in an excessive number of triggered breaths. Patient-ventilator asynchrony is often associated with a patient’s feelings of panic, which can be relieved by encouraging the patient to not “fight the ventilator” and relax while breathing with the ventilator. Selection of the appropriate mode and correct adjustment of the ventilator can eliminate most problems and reduce the need for sedation. (See Chapter 17 for more detailed information on patient-ventilator asynchrony.)
Identifying the cause of patient-ventilator asynchrony can be accomplished using a relatively simple approach (Box 18-3). If the patient is in severe distress, the first step is to disconnect the patient from the ventilator and carefully ventilate the patient using a manual resuscitation bag (i.e., avoiding excessive airway pressure). If the patient’s distress resolves immediately, the problem is with the ventilator; if the distress does not resolve, the problem is typically due to the patient experiencing anxiety or pain (Key Point 18-2).
Patient-Related Problems
The most common patient-related problems encountered during mechanical ventilation involve the placement and patency of the artificial airway, or the presence of a pneumothorax, bronchospasm, and excessive secretions (see Box 18-2).
Airway Problems
Examples of acute airway problems include kinking of the endotracheal tube (ET), impingement of the tube on the carina, and displacement of the tube upward, above the vocal cords or into the right mainstem bronchus (Box 18-4). Rupture of the innominate artery can also occur (this is usually seen with tracheostomy tubes) (Box 18-5).4 An unusual case study reported a fatal tracheal-innominate artery fistula caused by fixed positioning of the Hi-lo Evac tube to the left upper molar.6 This type of ET is used for continuous aspiration of the subglottic secretions. Apparently, the continuous suction pressure against the soft tissue of the trachea for an extended period resulted in erosion of the tissue and, eventually, exposure of the innominate artery. This catheter has been redesigned to reduce the risk of this complication.
A quick check of the patient’s oral cavity can sometimes reveal whether the ET is kinked or the patient is biting it. The clinician can easily determine whether the tube has been inserted too far or if it is too shallow in the airway by looking at the tube’s centimeter markings at the airway opening. A properly positioned oral ET typically shows a centimeter marking at the teeth at approximately 23 cm for men (range, 22-24 cm) and 21 cm for women (range, 20-22 cm). If the centimeter markings are less than the ranges cited, the tube is too high in the airway. If the marking is greater than the ranges cited, the tube has migrated deeper into the airway.
If a serious airway problem cannot be resolved quickly, the clinician should ventilate the patient manually to assess airway patency. If the patient cannot be ventilated in this manner, an appropriately sized suction catheter should be passed through the artificial airway. If the catheter does not pass freely (and the patient is not biting on the ET), the tube is most likely obstructed. The cuff should then be deflated, which may allow some air to move around the tube in spontaneously breathing patients. If the obstruction cannot be cleared, the tube must be removed immediately and the patient ventilated with a resuscitation bag until reintubation is possible.7,8
Pneumothorax
Pneumothorax is another possible problem that must be detected during positive pressure ventilation (PPV) and treated quickly. Pneumothorax can be recognized as increased WOB if a patient is conscious. For example, the patient may have nasal flaring, use of accessory muscles, uneven chest wall movement, and absence of breath sounds on the affected side. Auscultation and percussion of the chest, cardiovascular assessment, and ventilating pressure evaluations usually can distinguish a pneumothorax from other problems. Table 8-1 provides physical and radiologic findings commonly seen in patients with pulmonary disorders such as pneumothorax, asthma, emphysema, pneumonia, and pleural effusion.
If a tension pneumothorax is strongly suspected and cardiopulmonary arrest is imminent, a 14- or 16-gauge needle is inserted into the second intercostal space at the midclavicular line, over the top of the rib on the affected side. If the patient’s condition is stable, a confirming chest radiograph can be obtained with chest tube placement and pleural drainage. The following case study describes the case of a patient with sudden respiratory distress.
Bronchospasm
Bronchospasm may be manifested as dyspnea, wheezing, evidence of increased WOB (i.e., such as heightened use of accessory muscles), lack of coordination of chest or abdominal wall movement, retraction of the suprasternal, supraclavicular and intercostal spaces, and increased Raw [as evidenced by increased (PIP) and transairway pressure (PIP − Pplateau]. Wheezing associated with increased Raw from airway hyperreactivity, such as occurs with asthma, can be treated with bronchodilators and parenteral corticosteroids. Wheezing can also be associated with cardiogenic problems and pulmonary emboli.
Secretions
Evaluation of the patient’s secretions can be useful to differentiate a variety of problems. (See Table 12-2 for a list of sputum findings and possible associated problems.) Drying of secretions is most often associated with inadequate humidification (Key Point 18-3). Copious amounts of secretions can occur with pulmonary edema and certain pulmonary disorders (e.g., cystic fibrosis). Depending on their characteristics, secretions may also suggest the presence of a respiratory infection; however, this is not usually a problem with a sudden onset. It is essential that the patient is provided appropriately warmed and humidified air.8 Suctioning should be performed only when indicated rather than according to a fixed schedule. Bronchial hygiene may include postural drainage and percussion and therapeutic bronchoscopy. (Chapter 12 presents additional information on bronchial hygiene and therapeutic bronchoscopy.)
Pulmonary Edema
Pulmonary edema can be either cardiogenic or noncardiogenic in origin and should be managed accordingly. Cardiogenic pulmonary edema can occur suddenly and often manifests with thin, frothy, white to pink secretions. In cases where cardiogenic pulmonary edema is suspected, the clinician should check for additional evidence of a cardiac problem, such as electrocardiographic findings, elevated blood pressure, evidence of neck vein distention, a history of heart disease, and data from a pulmonary artery catheter, if available (see Chapter 11). Cardiogenic pulmonary edema and heart failure can often be managed successfully with medications that reduce preload, increase contractility, and reduce afterload, such as furosemide (Lasix), digoxin (Lanoxin), enalapril maleate (Vasotec), and morphine.
Noncardiogenic pulmonary edema or pulmonary edema that is caused by an increase in pulmonary capillary permeability (e.g., ARDS) usually develops over a day or two and is not a sudden-onset problem. The management of ARDS is discussed in Chapter 13.
Dynamic Hyperinflation
Auto-PEEP causes dynamic hyperinflation of the lungs and can lead to difficulty with ventilator triggering.9 Auto-PEEP can also cause cardiovascular problems, such as hypotension and reduced cardiac output. One of the best ways to detect the presence of auto-PEEP is through the evaluation of the ventilator waveforms. Auto-PEEP should be suspected whenever flow does not return to baseline in either a flow-time scalar (see Fig. 17-11) or a flow-volume loop (see Fig. 10-41). Efforts to reduce auto-PEEP can be aided by reducing the inspiratory time (TI), minute ventilation ( ), and Raw. (Chapter 17 provides additional information on auto-PEEP.) As previously mentioned, auto-PEEP hinders a patient’s ability to trigger the ventilator (see Fig. 7-1). (See Chapter 7 for a discussion of how raising the applied PEEP [extrinsic PEEP] can be used to ease breath triggering in patients with chronic obstructive pulmonary disease [COPD] when auto-PEEP cannot be completely eliminated.)
), and Raw. (Chapter 17 provides additional information on auto-PEEP.) As previously mentioned, auto-PEEP hinders a patient’s ability to trigger the ventilator (see Fig. 7-1). (See Chapter 7 for a discussion of how raising the applied PEEP [extrinsic PEEP] can be used to ease breath triggering in patients with chronic obstructive pulmonary disease [COPD] when auto-PEEP cannot be completely eliminated.)
Abnormalities in Respiratory Drive
Inadequate output from the respiratory centers of the brain can occur as a result of heavy sedation, acute neurologic disorders, or neuromuscular blockage.10 However, these conditions are more likely to reduce respiratory function than to produce sudden respiratory distress. Increased output from the respiratory centers is associated with pain, anxiety, increased peripheral sensory receptor stimulation, medications, increased ventilatory needs, and inappropriate ventilator settings.
Change in Body Position
Changes in the patient’s position can be associated with accidental extubation, bending and twisting of the patient circuit, and in some cases alterations in patient’s level of oxygenation. Reductions in oxygenation can occur with repositioning of the patient so that the diseased lung is placed in a dependent position. It can also occur with sudden airway obstruction by a mucous plug, secretions, or clot migration that leads to a pulmonary embolus. (Changing the patient’s body position can cause a thrombus to dislodge and migrate, causing a pulmonary embolus.)
Drug-Induced Distress
It is important to recognize that when acute respiratory distress develops in a ventilated patient in the ICU and the cause cannot be readily identified, possible causes may be related to medications the patient takes or possible chemical dependency. For example, intravenous morphine, which is commonly used to relieve pain, can cause nausea, hypotension, disorientation, hallucinations, fever, constipation, and respiratory arrest. This may be especially true in the older patients, whose ability to metabolize and clear medications may be diminished.
Patients with chemical dependency (alcohol, drug, or tobacco) present additional clinical management issues, particularly if the ICU staff is unaware of a patient’s chemical dependency. Sudden interruption of use of the chemical by the patient may cause symptoms of withdrawal syndrome, such as anxiety, restlessness, irritability, insomnia, and inability to focus attention.
Abdominal Distention
Abdominal distention can be associated with air being introduced into the stomach (e.g., via a nasogastric tube) and with a number of disorders, including ascites, abdominal bleeding or obstruction, and liver or kidney disorders. Some of these conditions have a slower onset than others, but all cause an upward pressure on the diaphragm, restricting its downward movement. This restriction of diaphragm movement can lead to atelectasis in the basilar areas of the lungs, ventilation/perfusion abnormalities, and hypoxemia.
Pulmonary Embolism
Pulmonary embolism (PE) is another acute onset problem that can lead to patient-ventilator asynchrony. The rapid onset of hypoxemia from a large embolus leads to all the signs of distress previously described. The patient typically demonstrates the presence of bilateral breath sounds, indicating that both lungs are being ventilated (i.e., PE interferes with perfusion not ventilation). With PE the heart rate, blood pressure, and respiratory rate are elevated. Even with high ventilator rates and flows, the patient may use accessory muscles to breathe and may become very pale. Checking airway patency and ventilating pressures and increasing the FIO2 may not reverse the arterial oxygen desaturation (SaO2). Disconnection from the ventilator and manual ventilation will also not help relieve the distress.
Pulmonary embolism is an emergency that often leaves the clinician feeling helpless to determine the cause and treatment (Case Study 18-1). Capnography findings can, however, provide a clue to the presence of a PE. A decrease in the end-tidal carbon dioxide (PETCO2) value compared with previous readings and a widening of the arterial-to-end-tidal partial pressure CO2 gradient (P[a-et]CO2) may suggest the presence of an embolus. Demonstration of the presence of a PE usually requires a pulmonary angiogram and computerized tomography. Thrombolytic therapy, such as the use of alteplase (recombinant tissue plasminogen activator, recombinant [tPA]; Actilyse) or reteplase (Retavase), may be appropriate.
Ventilator-Related Problems
Clinicians typically rely on algorithms to identify problems with the patient-ventilator circuit. A relatively quick way to identify whether the problem is a ventilator related is to determine whether the patient’s respiratory distress is relieved by manual ventilation with 100% oxygen. If the intervention relieves the respiratory distress, then the problem is probably associated with the ventilator or with the applied ventilator-management strategy.
Leaks
Activation of low-pressure, low-volume, and low  alarms typically indicate that a leak in the patient-ventilator circuit is present. (As discussed later in this chapter, the presence of a leak can be verified by analyzing the various ventilator graphics that are available on most ICU ventilators.) Leaks are commonly caused by disconnection of the patient from the ventilator; if this is the problem, the ventilator circuit simply needs to be reconnected to the patient’s artificial airway.
alarms typically indicate that a leak in the patient-ventilator circuit is present. (As discussed later in this chapter, the presence of a leak can be verified by analyzing the various ventilator graphics that are available on most ICU ventilators.) Leaks are commonly caused by disconnection of the patient from the ventilator; if this is the problem, the ventilator circuit simply needs to be reconnected to the patient’s artificial airway.
Leaks can also occur around the cuff of the ET. To determine whether this is the problem, the clinician should auscultate over the tracheal area for abnormal breath sounds during inspiration. To correct a cuff leak, the cuff is reinflated and the cuff pressure is rechecked. If a minimum leak technique is used, the cuff leak and tracheal air sounds should be present at peak inspiration under normal conditions. (See Chapter 4 for more detailed information on checking the circuit and evaluating for leaks.) Small ETs, such as those used with neonates, do not have cuffs and therefore allow for a minimum amount of air to leak around the tube. Migration of the ET into the upper airway, above the vocal cords, is another possible cause of a leak associated with the ET.
Circuit leaks also can occur at junctions in the patient circuit where connections exist. These may include connections at water traps, humidifiers, and HMEs; inline closed-suction catheters; temperature probes; inline metered-dose inhaler chambers; proximal airway pressure lines; capnograph (CO2) sensors; and unseated or leaking exhalation valves. Another, less common source of leaks is a pleural drainage system. In this situation, compensation for pleural leaks sometimes can be accomplished by increasing volume delivery to the patient. The amount of air leaking through the pleural drainage system can be determined by comparing the inspiratory and expiratory tidal volume (VT).
Leak checks are typically performed when equipment is prepared for patient use, but these checks also can be performed while the equipment is in use, for example, if a patient circuit is changed. Newer ICU ventilators can automatically perform the patient-ventilator circuit test. A leak check can also be performed manually if a leak develops during patient ventilation. While the patient is ventilated manually, the clinician changes the ventilator mode to volume-controlled ventilation (VC-CMV) and sets the VT to 100 mL, the flow to 20 L/minute, the inspiratory pause to 2 seconds, and the pressure limit to maximum. The patient Y-connector is occluded with sterile gauze, and the ventilator is cycled manually. The circuit pressure that develops during inspiration should plateau and hold at that level, falling no more than 10 cm H2O during a 2-second pause. If the pressure falls more than this, a significant leak is present and must be corrected. If the leak cannot be corrected quickly and easily, a change of equipment may be necessary.
Inadequate Oxygenation
A condition of inadequate oxygenation is usually signaled by activation of a low SpO2 alarm. Patients typically demonstrate tachycardia (although bradycardia may also occur) along with other signs of hypoxemia. (See Table 4-1 for the signs and symptoms of hypoxia.) Note that arterial blood gas analysis is required to confirm the presence of hypoxemia. It is important to recognize that worsening hypoxemia can be an ominous sign of deteriorating lung function.
Inadequate Ventilatory Support
Inappropriate  and ventilator settings can cause an increased WOB, which can ultimately lead to patient-ventilator asynchrony. Respiratory acidosis and hypoxemia may also be seen in cases where the patient experiences an increased WOB. (Chapter 17 contains more information on the effects of increased WOB.)
and ventilator settings can cause an increased WOB, which can ultimately lead to patient-ventilator asynchrony. Respiratory acidosis and hypoxemia may also be seen in cases where the patient experiences an increased WOB. (Chapter 17 contains more information on the effects of increased WOB.)
Trigger Sensitivity
The ventilator’s trigger sensitivity level can be improperly set. Auto-triggering is a sign that the trigger sensitivity is set too low. Lack of ventilator response to a patient’s inspiratory efforts may be the result of incorrect sensitivity settings, low-flow settings, or a poorly responsive internal demand valve. The trigger sensitivity may also be altered when a nebulizer is being used that is powered by an external gas source, which can blunt the machine’s ability to sense a patient breath. Other causes are water in the inspiratory line and the presence of auto-PEEP.
Inappropriate sensitivity can be corrected easily by simply by increasing or decreasing the sensitivity setting. If this does not solve the problem, the other causes mentioned must be addressed individually.
Inadequate Flow Setting
A low inspiratory gas flow can be corrected by increasing the flow setting or by changing the flow pattern, such as using a descending ramp rather than a rectangular flow pattern. A concave inspiratory pressure scalar during VC-CMV indicates active inspiration with inadequate flow (Fig. 18-3).11 Changing the mode of ventilation also may be an effective means of providing adequate flow to the patient. For example, switching from VC-CMV to pressure ventilation with a volume target (e.g., pressure-regulated volume control) can change the flow pattern and sometimes relieve distress.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree