Theresa A. Gramlich
Basic Concepts of Noninvasive Positive-Pressure Ventilation
Learning Objectives
On completion of this chapter, the reader will be able to do the following:
1 Define noninvasive ventilation and discuss the three basic noninvasive techniques.
2 Discuss the clinical and physiological benefits of noninvasive positive-pressure ventilation (NIV).
4 Compare the types of ventilators used for noninvasive ventilation.
5 Explain the importance of humidification during NIV application.
6 Describe the factors that will influence the FIO2 from a portable pressure-targeted ventilator.
9 List the steps used in the initiation of NIV.
10 Discuss several factors that affect the delivery of aerosols during NIV.
11 Identify several indicators of success for patients on NIV.
13 Recognize potential complications of NIV.
14 Provide optional solutions to complications of NIV.
15 Describe two basic approaches to weaning the patient from NIV.
Key Terms
• Acute cardiogenic pulmonary edema
• Chest cuirass
• Community-acquired pneumonia
• Cor pulmonale
• Delay-time control
• Expiratory positive airway pressure
• Inspiratory positive airway pressure
• Inspissated secretions
• Intermittent positive-pressure breathing
• Intermittent positive-pressure ventilation
• Iron lung
• Nocturnal hypoventilation
• Noninvasive positive-pressure ventilation
• Obstructive sleep apnea
• Pressure targeted ventilators
• Ramp
• Simethicone agents
Noninvasive ventilation is the delivery of mechanical ventilation to the lungs using techniques that do not require an endotracheal airway.1 Before the 1960s nearly all techniques for mechanical ventilation were noninvasive. A tank or chest-wrap device was used to apply subatmospheric pressure to the body or chest area to ventilate the lungs. In the early 1960s researchers found that the survival rate for invasive positive-pressure ventilation delivered via an endotracheal or tracheostomy tube was higher than that for negative-pressure ventilation.1 As a result, invasive positive-pressure ventilation became the standard of practice for the support and management of patients with acute and chronic respiratory failure.
Invasive ventilation is effective and often necessary to support alveolar ventilation; however, it has many associated risks that often result in increased mortality and morbidity and a higher financial cost. Since the early 1980s, alternatives to invasive ventilation have been rapidly increasing and improving. Sufficient evidence now proves that application of positive pressure via a nasal mask, mouthpiece, or full facemask can reduce the need for intubation and its related complications, reduce mortality rates, and shorten the hospital stay for certain patients requiring mechanical ventilatory assistance.2–7
Types Of Noninvasive Ventilation Techniques
The three basic methods of applying noninvasive ventilation are negative-pressure ventilation, abdominal-displacement ventilation (discussed in Chapter 21), and positive-pressure ventilation.
Negative-Pressure Ventilation
Use of negative pressure ventilators peaked in the 1950s with the polio epidemic. Negative-pressure ventilators, or body ventilators, operated on the principle of increasing lung volumes by intermittently applying negative pressure to the entire body below the neck or just to the upper region of the chest. The negative pressure was transmitted across the chest wall, into the pleural space, and into the intraalveolar space. The resulting increase in transpulmonary pressure caused air to enter the lungs. Exhalation was simply passive and depended on the elastic recoil of the lung and chest wall.
The first successful negative pressure ventilator, known as the iron lung, was designed in 1928 by engineer Phillip Drinker and Dr. Charles McKhann. It consisted of a large metal cylinder that enclosed the patient’s entire body below the neck, leaving the head protruding through an airtight rubber neck seal. A simpler and less expensive version of this tank device, developed by J.H. Emerson in 1931, became the ventilator that was predominantly used to treat people paralyzed by polio.
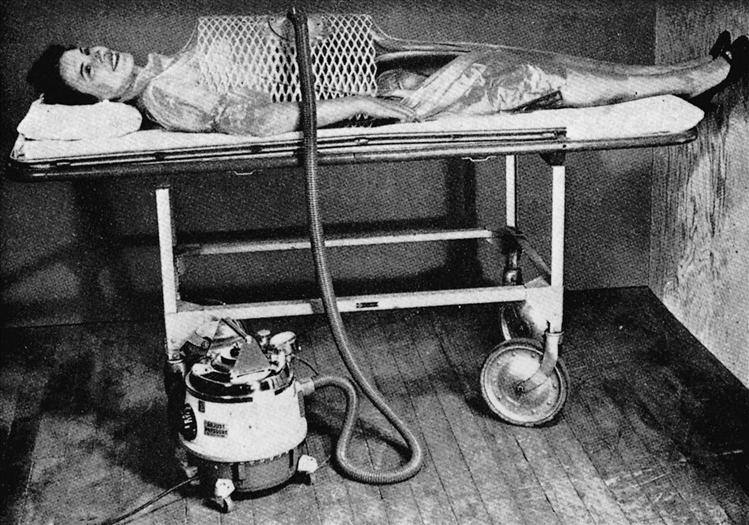
The bulk and lack of portability of the iron lung, along with the difficulty in providing routine care for patient , led to the development of smaller, portable negative-pressure devices. The chest cuirass, or shell ventilator, gained wide popularity during the 1950s. Two versions of this device were primarily used to apply negative pressure only to the thorax and upper abdomen. In one version, the patient’s chest was covered by a metal shell with an air-filled rubber edge that sealed the thorax. In later models, the shell was made of plastic, which made it easier to mold and fit to a patient’s chest. The other type of chest ventilator was a wraparound piece of plastic over a shell that was powered by a vacuum-cleaner motor (Fig. 19-1).
Positive-Pressure Ventilation
The use of positive-pressure ventilation can be traced as far back as 1780, when the first bag-mask apparatus was designed for resuscitative efforts. Positive-pressure ventilation with a mask was first used clinically in the mid-1940s, when Motley et al8 treated patients with acute respiratory failure (ARF) caused by a variety of clini-cal conditions. This intermittent positive-pressure ventilation (IPPV), which used a pressure-targeted ventilator and a mask, later was used primarily to treat ARF complicated by chronic obstructive pulmonary disease (COPD) and asthma. Volume-targeted ventilators and invasive airways were developed in the 1960s and became the standard for providing positive pressure ventilation in the treatment of respiratory failure. Intermittent positive-pressure breathing (IPPB), which used a mask or mouthpiece, became a means of simply delivering aerosolized medication periodically with positive-pressure breaths.
In 1980 clinical evidence began to show that the benefits of IPPB were often overstated and could be accomplished using other simpler and more cost-effective therapies.9 As IPPB lost favor in clinical practice, nasal-mask continuous positive-airway pressure (CPAP) began to emerge as a highly effective therapy in the treatment of obstructive sleep apnea (OSA).10–12 Researchers found that application of low levels of continuous airway pressure through a mask interface created a pneumatic splint that prevented airway collapse during sleep.10
The use of positive-pressure ventilation via mask soon was reported to be successful in the treatment of chronic ventilatory insufficiency and muscle weakness in patients with various neuromuscular illnesses.13–15 In 1989 Meduri et al16 successfully treated a small sample of patients with ARF using pressure-support ventilation through a facemask.
These successes stimulated the production of variable interfaces and small pressure- and volume-targeted ventilators that were lightweight, easy to operate, and ideal for home use. Over the past decade, the use of NIV has increased dramatically, and NIV is now used to treat both acute and chronic respiratory failure in a variety of clinical settings.
Goals Of And Indications For Noninvasive Positive-Pressure Ventilation
The goals of noninvasive positive-pressure ventilation (NIV) and the indications for its use are based on decades of clinical expertise and systematic research. The following sections review the evidence that supports the use of NIV in various disorders associated with acute and chronic respiratory failure.
Acute-Care Setting
In acute respiratory failure, NIV is considered a lifesaving application that offers a number of benefits over invasive positive-pressure ventilation (Box 19-1). The most significant benefit is the avoidance of intubation. Endotracheal intubation is associated with complications such as airway trauma, increased risk of aspiration, nosocomial pneumonia, and considerable patient discomfort, requiring the use of sedatives. Such complications can lead to a longer hospital stay, higher mortality rate, and increased health care costs. Evidence has established that NIV can safely and successfully support ventilation, without endotracheal intubation, until the condition leading to the ARF has been reversed. In addition, evidence strongly indicates that NIV reduces the mortality rate, reduces the duration of ventilator use, and shortens the hospital stay in appropriately selected patients. The avoidance of intubation and invasive ventilation, therefore, is the primary goal of NIV in the acute-care setting.
The physiological goal of NIV in ARF is to improve gas exchange by resting the respiratory muscles and increasing alveolar ventilation. NIV reduces diaphragmatic pressure swings, which suggests that the respiratory muscles are being rested. In addition, when positive end-expiratory pressure (PEEP) is applied during pressure-supported ventilation (PSV), PEEP helps offset auto-PEEP, thereby reducing the work required to initiate inspiration.17 Likewise, pressure support (PS) facilitates inspiration, thus increasing the tidal volume (VT). Resting of the respiratory muscles and improved VT lead to a lower arterial partial pressure of CO2 (PaCO2), better oxygenation, and decreased respiratory rates.
Acute Exacerbation of Chronic Obstructive Pulmonary Disease
During an acute exacerbation of COPD, increased airway resistance and an increased respiratory rate lead to hyperinflation, development of auto-PEEP (air-trapping), and alveolar hypoventilation. As hyperinflation worsens, respiratory muscle activity increases, significantly increasing the oxygen cost of breathing. This becomes a vicious circle of increased demand for ventilation, further air-trapping, hypoventilation, and muscle fatigue. Without intervention, ventilatory failure and death may occur. Conventional medical therapy for these patients has included bronchodilators, antiinflammatory agents, careful oxygen administration, and antibiotics. If these measures failed, endotracheal intubation and invasive ventilation were the next therapeutic steps. Studies of patients with COPD who had acute exacerbations have shown that NIV reduces inspiratory muscle activity and the respiratory rate and increases VT and minute volume, allowing for better gas exchange and respiratory muscle rest.18–21 NIV may help reverse the acute condition when used in conjunction with conventional medical therapy.18
The use of NIV in the treatment of ARF caused by COPD exacerbation has been very successful and has been studied more than any other disorder leading to ARF. The strongest evidence from randomized, control trials has confirmed that use of NIV with a facemask significantly reduces the need for intubation, shortens the duration of mechanical ventilation, shortens the patient’s stay in the intensive care unit (ICU), and reduces complications and the mortality rate.2–7
Compared with patients receiving only conventional medical therapy (e.g., bronchodilators, antiinflammatory agents, oxygen, and antibiotics), patients receiving NIV have shown significant improvement in vital signs, pH and blood gas values, respiratory rate, and breathlessness within the first hour of application.3,6,7,19 These results have been so compelling that NIV currently is considered a standard of care for the treatment of COPD exacerbation in selected patients20,21 (Key Point 19-1).
Asthma
Although the evidence is inconclusive, patients with status asthmaticus complicated by CO2 retention have shown positive outcomes when treated with a trial of NIV. The benefits observed have included improved gas exchange, decreased PaCO2, and rapid improvement in vital signs within the first 2 hours of NIV treatment.22,23 Patients with acute bronchospasm seem to respond better to delivery of adrenergic agents by NIV than by small-volume nebulizer.24 The benefits of NIV include decreased intubations and complications and a reduced mortality rate. Although specific criteria for the selection of asthma patients to receive NIV have not yet been developed, NIV may be appropriate in patients who do not respond to conventional treatment methods.
Hypoxemic Respiratory Failure and Acute Respiratory Distress Syndrome
Evidence of the efficacy of NIV in the treatment of hypoxemic respiratory failure has been inconsistent, probably because of the wide variety of non-COPD parenchymal processes that can cause hypoxemic respiratory failure. Such processes include pneumonia, acute respiratory distress syndrome, trauma, and cardiogenic pulmonary edema. These conditions usually result in severe impairment of gas exchange characterized by refractory hypoxemia, a ratio of arterial partial pressure of oxygen to fractional inspired oxygen (PaO2/FIO2) ratio under 200, and a respiratory rate over 35 breaths/min. Patients who received the usual medical care for hypoxemic acute respiratory failure were compared with patients who received NIV plus the usual medical care.22,25,26 NIV significantly improved gas exchange, reduced the need for intubation, and reduced the mortality rate in these patients. NIV can be as effective at improving oxygenation within the first hour as invasive ventilation and is associated with fewer complications and a shorter ICU stay.27 On the other hand, some researchers have found no significant improvement in patients’ overall condition with NIV unless the patients were also hypercapnic.28 Although many studies have shown promising results with the use of NIV in hypoxemic respiratory failure, the various causes of the disorder make it difficult to apply all of these findings to individual patients.
Community-Acquired Pneumonia
Of the various causes of hypoxemic respiratory failure treated with NIV, pneumonia appears to be one of the most challenging and least consistent for successful outcomes. In a study of patients with COPD and ARF, 38% of the unsuccessful attempts with NIV were associated with the presence of pneumonia.29 On the other hand, the intubation rate, ICU stay, and mortality rate were reduced when NIV was used to treat patients with severe community-acquired pneumonia (CAP).22,25 In the case of CAP, most of the favorable results were from the subgroup of COPD patients who had pneumonia. In a study by Jolliet et al,30 22 of the 24 of non-COPD patients with severe CAP and ARF who received NIV showed initial improvement in oxygenation and a reduced respiratory rate. However, despite the improvement, nearly two thirds of the patients eventually required intubation and mechanical ventilation. Those patients who continued to receive NIV had shorter ICU and hospital stays. Because of the mixed results produced by studies, the current suggestion is that patients with COPD and pneumonia receive an initial trial of NIV. However, caution should be used when non-COPD patients with pneumonia are treated with NIV.
Cardiogenic Pulmonary Edema
Mask CPAP has been used effectively for many years to treat acute cardiogenic pulmonary edema (ACPE).16,31 When patients with ACPE do not respond to conventional pharmacologic and oxygen therapy, the use of mask CPAP with oxygen may expand fluid-filled alveoli, resulting in the following:
Several studies have reported similar success in treating ACPE with NIV by mask using PSV plus PEEP.32–34 Rapid improvement in gas exchange, pH, and reduced intubation rates were noted. Patients who were already hypercapnic responded best. A comparison of NIV with CPAP in the treatment of ACPE showed that patients treated with NIV demonstrated more rapid improvements in PaCO2 and pH, but the mortality and intubation rates were not significantly different.35 Although both NIV and CPAP are equally effective in treating respiratory failure associated with ACPE,36 CPAP is more cost effective and easier to set up. The current recommendation is that CPAP (10-12 cm H2O) be used initially in the treatment of ACPE and that NIV be used only in patients who continue to be hypercapnic and dyspneic thereafter37 (Key Point 19-2).
Chronic-Care Setting
In chronic respiratory failure, NIV is a supportive therapy rather than a lifesaving treatment. Most of the clinical disorders that require this level of support are characterized by chronic hypo-ventilation, nocturnal desaturation, respiratory muscle fatigue, and poor sleep quality. As the disease process progresses, daytime gas exchange worsens and patients often show classic symptoms of chronic hypoventilation (Box 19-2).
Nocturnal use of NIV (4-6 hours) can have certain clinical benefits for patients with chronic hypoventilation disorders (see Box 19-1). The most significant of these are improvement of symptoms associated with chronic hypoventilation and an improved quality of life. Although the physiological mechanism underlying these benefits is not well understood, investigators have hypothesized that NIV benefits these patients in one or all of the following ways38–41:
Restrictive Thoracic Disorders
Restrictive thoracic disorders include chest wall deformities and neuromuscular conditions that result in progressive muscle weakness, hypoventilation, and eventually respiratory failure. Patients with neuromuscular disorders were the first group of patients studied to be successfully converted from invasive ventilation (tracheostomy) to NIV (mouthpiece interface).38 These patients required continuous support; however, NIV also can benefit patients to be ventilatory support only at night or intermittently during the day. In the short-term use group, daytime gas exchange and respiratory muscle strength improve and symp-toms of hypoventilation are alleviated.39–41 Nocturnal use of NIV also eliminates OSA and oxygen desaturation at night, which are common in patients who use negative-pressure ventilatory support.41
Quality of life also seems to improve for patients with neuromuscular disorders who use NIV. A high degree of satisfaction, along with improved mental well-being and psychosocial functioning, has been noted for patients with restrictive thoracic disorders.42 Long-term follow-up case series have shown significantly shortened hospital stays and an overall increased survival times compared with patients who did not receive ventilatory support.43 For these reasons, the consensus is that NIV is the ventilator mode of choice for chronic respiratory failure caused by restrictive thoracic disorders in patients who can protect their own airway44,45 (Key Point 19-3).
Chronic Stable Chronic Obstructive Pulmonary Disease
Evidence of the efficacy of long-term nocturnal NIV is vague and often contradictory in severe stable COPD. Early studies of patients with severe stable COPD focused on the use of intermittent negative-pressure ventilation to rest the muscles of respiration.46,47 Some investigators reported potential benefits, but most patients could not tolerate the devices used, and the benefits were only temporary. In addition, negative-pressure ventilation actually collapsed upper airway structures during sleep and induced OSA.
A number of studies since have been performed on patients with severe stable COPD who used nocturnal NIV. Favorable results from these studies have included reduced daytime PaCO2, reduced nocturnal oxygen desaturation and hypoventilation, improved sleep quality, and improved quality of life.48–50 Other studies have found minimal or no benefit with nocturnal NIV in these patients.51,52 The discrepancy in these findings could be the result of differing patient selection, methods, or ventilator settings. Closer examination of baseline characteristics of the study participants reveals an important finding: the greatest benefits from NIV were seen in individuals who had more severe CO2 retention and more episodes of nocturnal desaturation.
Although the evidence is inconclusive, the current professional consensus and the guidelines from the Center for Medicare and Medicaid Services agree that patients be considered for NIV if they have severe daytime CO2 retention (PaCO2 of 52 mm Hg or higher) and nocturnal hypoventilation, despite the administration of nocturnal oxygen therapy.45
Cystic Fibrosis
The role of NIV in the treatment of advanced cystic fibrosis has not been precisely determined. In general, NIV increases VT, reduces diaphragmatic activity, and improves oxygenation in some patients with cystic fibrosis who have acute exacerbations.53 Intermittent use of NIV could help support these patients for several months while they await lung transplantation.54–56
Nocturnal Hypoventilation
Other disorders associated with nocturnal hypoventilation include central sleep apnea, obesity hypoventilation syndrome, and OSA combined with COPD or congestive heart failure. These disorders also may lead to daytime CO2 retention. If nocturnal hypoventilation is severe, symptoms will be severe and will manifest during the daytime (see Box 19-2). Without intervention, these symptoms can then progress to overt respiratory failure.
The therapy of choice for OSA is CPAP. However, if these patients continue to hypoventilate despite CPAP therapy, NIV may improve daytime gas exchange and symptoms associated with chronic hypoventilation.57 Likewise, patients with central hypoventilation or obesity hypoventilation syndrome who do not respond to first-line therapies (e.g., oxygen, respiratory stimulants, weight loss, supplemental oxygen, or CPAP) should be considered for treatment with NIV (Key Point 19-4).
Other Indications For NIV
Facilitation of Weaning from Invasive Ventilation
Clinical weaning reduces the number of patient ventilator days in the ICU.58,59 Reducing the number of days a patient receives invasive mechanical ventilation reduces the risk of infection and other complications, lowers the mortality rate, and reduces health care costs.58,60 Many respiratory care departments in acute-care facilities have devised weaning protocols for discontinuing ventilation and extubating patients as soon as possible. However, many weaning protocols depend on patient tolerance of daily spontaneous breathing trials to determine the likelihood of successful extubation. (See Chapter 20 for information on weaning and spontaneous breathing trials.) After extubation, the excessive load spontaneous breathing places on the respiratory muscles can lead to fatigue and reintubation.
In addition, NIV can be used after extubation in patients who show fatigue. In these patients NIV reduces the work of breathing (WOB) and maintains adequate gas exchange as effectively as invasive ventilation.61 NIV can also shorten the duration of invasive ventilation.62,63 In one study a group of patients for whom 3 days of spontaneous breathing trials had failed was placed on NIV.64 In these patients, WOB was reduced, adequate gas exchange was maintained, and the ICU and hospital stays were shortened. These patients were less likely to need a tracheotomy.63 Most patients who seem to benefit from NIV during weaning from invasive ventilation suffer from chronic illness (e.g., COPD). Therefore, it is questionable whether the benefits of NIV would apply to patients with other disease processes. Nonetheless, the evidence is strong enough to warrant consideration of NIV in patients for whom spontaneous breathing trials fail and who meet appropriate NIV selection criteria.
“Do Not Intubate” Patients
Patients with terminal or advanced disease who develop ARF are not good candidates for endotracheal intubation and mechanical ventilation. NIV may be an alternative therapy for these patients, although its use remains controversial. Previous studies involving mainly end-stage COPD patients in whom endotracheal intubation was contraindicated, found that most of these patients were successfully supported with NIV and weaned.65,66 Many would not have survived the acute process had they not been placed on NIV. Patients with COPD and acute pulmonary edema may also benefit from support with NIV. However, survival was not improved in patients with ARF arising from other causes such as pneumonia or cancer.67
The argument in favor of using NIV with a patient having “do not intubate” status is that NIV may relieve severe dyspnea and preserve patient comfort. It may also reverse the acute process in disorders such as COPD or pulmonary edema and allow the patient to live longer.68 The argument against NIV is that it could actually prolong the dying process, add to patient discomfort, and consume valuable resources.69 When NIV is used in such cases, the patient and family members should be told that NIV is a form of life support that can be uncomfortable but that may be removed at any time.20
Patient Selection Criteria
The success of NIV and the avoidance of major complications depend on appropriate selection of patients in both the acute- and chronic-care settings. Evidence gained from the use of NIV in various patient populations and clinical settings has led to the development of guidelines that promote the highest chance of success (Table 19-1).
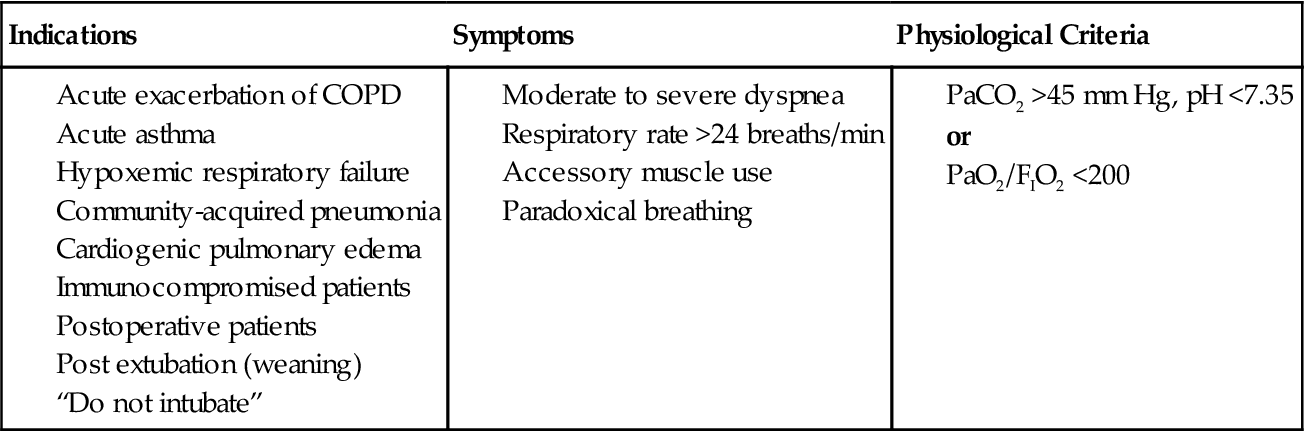
TABLE 19-1
Indications, Symptoms, and Selection Criteria for NIV in Acute Respiratory Failure in Adults
Acute-Care Setting
In the acute-care setting, the selection process must consider the patient’s diagnosis and clinical characteristics, as well as the risk of failure. If this assessment is viewed as a two-step process, the first step is to establish the need for ventilatory assistance according to clinical and blood gas criteria. For example, NIV may be unnecessary for patients with mild respiratory distress, and NIV for a patient who has already deteriorated to severe respiratory failure may delay life-saving intubation and ventilation. The consensus of studies is that patients who need ventilatory assistance show signs and symptoms of distress, including tachypnea (respiratory rate >24 breaths/min), use of accessory muscles, and paradoxical breathing.45 Blood gas criteria should reveal a moderate to severe respiratory failure (i.e., a pH <7.35 and PaCO2 >45 mm Hg, or a PaO2/FIO2 <200).
Once the need for ventilatory support is established, the second step is to exclude patients at increased risk of failure and complications (Box 19-3). Such patients include individuals with respiratory arrest, hemodynamic instability, or other major organ involvement; patients with excessive secretions; and patients unable to protect their airway because of impaired cough or swallowing ability. Patients with any of these disorders are at highest risk for aspiration. Finally, agitated and confused patients or those with facial burns or deformities that preclude a good mask fit are excluded.
A final consideration in the selection of patients with ARF is the potential reversibility of the disease process. Overwhelming evidence supports the use of NIV in acute exacerbations of COPD. Supportive ventilatory assistance allows time for conventional therapies (e.g., bronchodilators, oxygen, antibiotics) to reverse the acute process so that intubation may be avoided. Other causes of ARF may not be treated as successfully as COPD, but a trial of NIV may be warranted if the patient meets the selection criteria. All patients should be monitored closely so that intubation, if necessary, is not unduly delayed (Key Point 19-5).
Chronic-Care Setting
Establishment of the need for intermittent ventilatory assistance in patients with chronic respiratory failure begins with the recognition of typical symptoms of nocturnal hypoventilation and poor sleep quality. These most commonly include the following:
Objective criteria, such as blood gases, often are variable and depend on the rate of progression of the disease process. For patients with restrictive thoracic or central hypoventilation disorders, institution of NIV is recommended when PaCO2 is 45 mm Hg or higher or when sustained nocturnal desaturation occurs, as evidenced by an oxygen saturation by pulse oximeter (SpO2) under 88% for longer than 5 consecutive minutes.44 NIV also may be indicated if the patient with restrictive thoracic disease is symptomatic and has severe pulmonary dysfunction (vital capacity [VC] <50% of the predicted level), even if CO2 retention is absent.44 Patients with nocturnal hypoventilation or OSA may require only nocturnal CPAP for splinting the airway open to overcome hypoventilation. However, NIV should be initiated if patients with moderate to severe OSA do not respond favorably to CPAP. Patients who recover from episodes of ARF or who are hospitalized repeatedly for exacerbations of their condition also should be considered for noninvasive ventilatory assistance (Key Point 19-6).
The conflicting findings of studies on the use of NIV for severe stable COPD make it difficult to develop evidenced-based selection guidelines. A review of studies with favorable outcomes found that COPD patients with severe hypercapnia were most likely to benefit from NIV.50,70 Therefore a consensus of medical experts recommends the use of nocturnal NIV in symptomatic yet medically stable patients with COPD whose daytime PaCO2 is 55 mm Hg or higher.44 The term medically stable in this instance means that the patient is being optimally treated, and OSA and CPAP therapy have been considered and ruled out.44 These experts also recommend a trial of NIV if the PaCO2 is 50 to 54 mm Hg in COPD patients receiving long-term oxygen administration (2 L/min or more) who still have evidence of frequent hypopnea episodes and sustained nocturnal desaturation. In addition, a history of frequent hospitalizations for exacerbations helps to justify the use of NIV in COPD patients.
As for any patient requiring NIV, the ability to protect the airway is crucial. This is especially important for patients with chronic respiratory failure because most of these individuals live at home or in an extended-care setting and may not be monitored closely. Patients with neuromuscular disorders may present an even greater challenge as their disease progresses and they begin to lose oropharyngeal muscle strength and the ability to generate an effective cough. Cough-assisting devices or techniques may help these individuals clear secretions and maintain a patent airway.
Patient motivation must be considered with NIV in the chronic-care setting. Very few, if any, therapeutic results are realized if the patient does not comply with the prescribed therapy. Among patients undergoing long-term treatment with NIV, those with COPD and little CO2 retention were least compliant.71 This emphasizes the importance of selecting patients who are symptomatic and who are motivated by the desire for relief of those symptoms. Table 19-2 summarizes the symptoms and selection criteria for chronic respiratory failure disorders.
TABLE 19-2
Indications, Symptoms, and Selection Criteria for NIV in Chronic Disorders
| Indication | Symptoms | Physiologic Criteria |
Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|