Fig. 17.1
Left main bronchus encircled with a “golden finger” (LMB left main bronchus, T trachea)
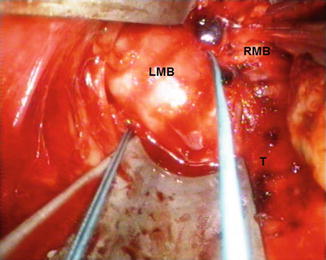
Fig. 17.2
Cranial traction of the left main bronchus in order to place the stapler (LMB left main bronchus, RMB right main bronchus, T trachea)
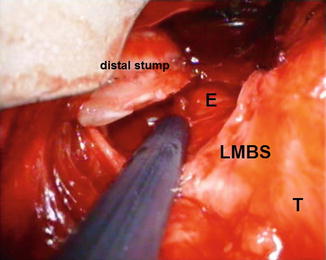
Fig. 17.3
Aspect after stapling of the insufficient left bronchial stump (LMBS left main bronchial stump, T trachea, E oesophagus)
On the right side, after the subcarinal videomediastinoscopic lymphadenectomy, it is the moment of using the sternal retractor which elevates the sternum in order to achieve more space. Due to the angle of the right main bronchus with the trachea and the direct contact with the pulmonary artery (usually very adherent), the dissection is a little more difficult but not impossible. The superior vena cava and the azygos vein are also in close proximity to the main bronchus and need a careful dissection.
The spreadable mediastinoscope is not always necessary during this dissection, the elevated sternum conferring usually enough work space, similar to TEMLA.
Actually, the most important part of the technique on the right side is the separation between the bronchus and the artery. The use of a roticulated stapler is mandatory on the right side and positioning the instrument correctly can be challenging or even impossible sometimes due to the lack of space. Sometimes a longer cartridge (45 mm) can be necessary in order to completely cut the right main bronchus. Bronchoscopy can be useful in order to assess the correct position of the stapler and the relation with the right upper lobe bronchus.
If the initial interventions took about 2 h to be done, afterwards we were able to perform them in about 45 min on the left side and 1 h for the right side. The senior author of this article started these interventions and, later on, other surgeons from the department, after observation of the technique and all having skill in mediastinoscopy, were able to perform it, too.
17.6 Results
Our experience, starting with the first patient in 2010, consists of 10 cases, 8 on the left side and 2 on the right. We have approached the main bronchus to close a postpneumonectomy fistula in 5 cases (4 on the left side and 1 on the right side), and in other 5 cases (also 4 on the left side and 1 on the right side), we stapled the bronchus as a first step in preparation for future pneumonectomies for suppurative lung disease. The procedure was well tolerated in all cases. With the fistula closed, the patients with postpneumonectomy empyema received proper treatment for the infected cavity – open window thoracostomy with daily dressing and finally removal of the distal bronchial stump and closure of the thorax by means of thoracomyoplasty. The removal of the distal bronchial stump before closing the open thoracostomy is not very easy as dissection made in fibrotic tissue in close proximity to pulmonary vessels, but with attention it can be accomplished without further problems.
In the series of patients with suppurative lung disease, one patient died from uncontrolled sepsis 3 months after the transcervical approach. The patient was a 21-year-old young man with tuberculous destroyed lung and pleural empyema, Marfan syndrome and cachexia. He also had an open window thoracostomy with the lung in place, but the infection could not be managed. Collaboration with this patient was very difficult as he also was mentally retarded.
The other four patients had an uneventful evolution, with pneumonectomy performed 3–4 weeks after transcervical bronchial closure. The dissection of the bronchus during postponed pneumonectomy was a little more difficult than usual.
17.7 Complications
We start with the operative incidents. Apart from those described for mediastinoscopy, we would like to emphasise:
Bronchial artery laceration, when we mobilise the subcarinal lymph nodes. This requires careful haemostasis with a clip or a vascular seal with an energy device.
Tracheal or bronchial wall laceration. We must try to include this laceration into the mechanical suture line or to place a manual suture with an endoscopic needle holder and a 3-0 polydioxanone suture with a 1-cm needle. If this is not possible, sternotomy is required for the repair.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


