Fig. 2.1
Set of general instruments required for mediastinoscopy: (a) scalpel, (b) electrocautery, (c) dissection forceps, (d) Mayo and Metzenbaum scissors, (e) right-angle dissector and (f) Farabeuf retractors
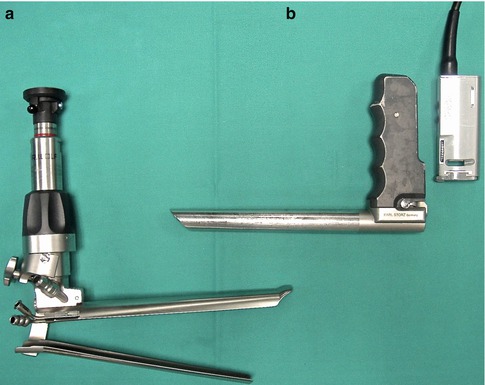
Fig. 2.2
Video-mediastinoscopes: (a) spreadable video-mediastinoscope and (b) non-spreadable video-mediastinoscope
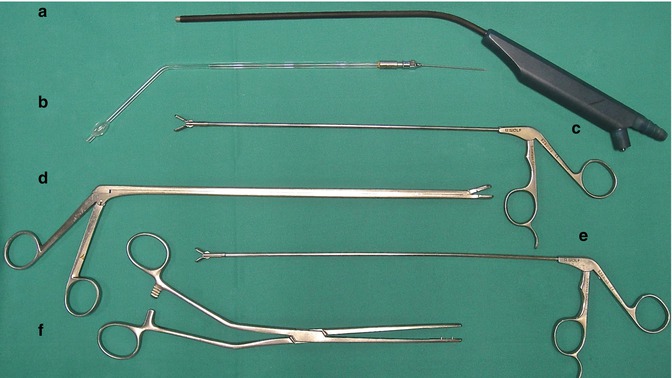
Fig. 2.3
Set of specific instruments required for mediastinoscopy: (a) dissection-suction-coagulation device, (b) glass tube for test puncture, (c) grasper, (d and e) biopsy forceps and (f) forceps to retrieve inserted gauzes
Standard mediastinoscopes and video-mediastinoscopes are in a right-angle shape, the vertical arm being the handle and the horizontal arm the scope proper. The scope is in the form of a truncated irregular cone and can be made either in one piece or in two spreadable blades (Fig. 2.2). The latter has a removable double tube that can be mounted inside the scope and is used for continuous suction and irrigation of the operative field (Fig. 2.4).
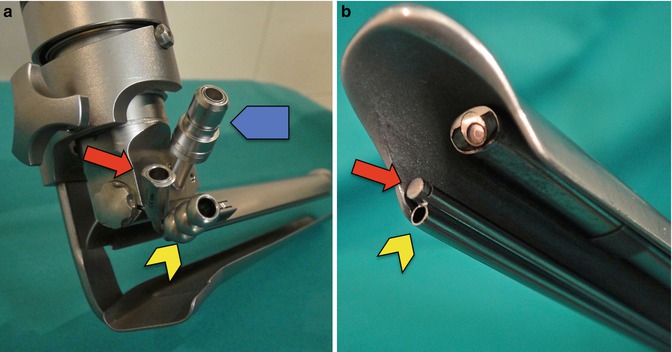
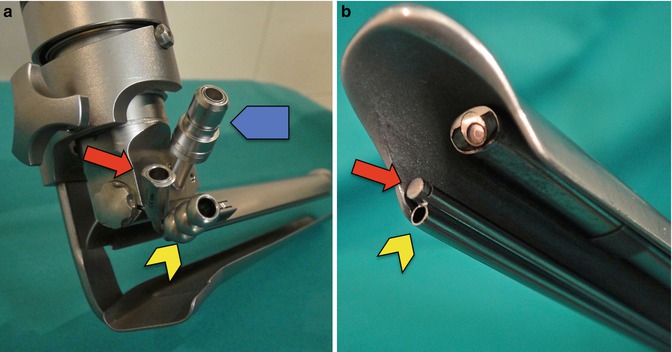
Fig. 2.4
Spreadable video-mediastinoscope: double tube inserted inside the scope for suction (yellow arrow) and irrigation (red arrow) of the operative field. The blue arrow shows the connection to the light source. (a) External view. (b) Internal view
2.5.2 Surgical Procedure
The patient is positioned in the supine decubitus under general anaesthesia and orotracheal intubation. Double-lumen intubation will be required if exploration of the pleural cavities is anticipated, by either mediastino-thoracoscopy or standard intercostal thoracoscopy. Hyperextension of the neck is achieved by a long cushion positioned under the patient’s shoulders. A round rubber cushion keeps the head in place and avoids displacement during the operation (Fig. 2.5). The operative field is prepared and draped as for median sternotomy, from under the mandible cranially to the xiphoid caudally and from nipple to nipple laterally. An extra drape is put over the sternum below the sternal notch to be easily removed if emergency sternotomy is required (Fig. 2.6). A peripheral vein in one arm or hand is cannulated for infusion of fluids and medication. An additional vein access in a foot is recommended for fast infusion of fluids and blood in case of copious bleeding from a mediastinal vessel (Fig. 2.7). Intraoperative monitoring includes EKG, blood pressure and right arm pulse (Fig. 2.8). The latter is useful to control excessive pressure exercised on the innominate artery during mediastinoscopy. The pulse wave will diminish or even disappear if the innominate artery is compressed against the anterior chest wall by the mediastinoscope. Compression can be easily relieved by repositioning the mediastinoscope. The surgeon stands or sits at the head of the patient, and the assistant and the scrub nurse either stand or sit on the right side. The television monitor for video-mediastinoscopy is positioned at the patient’s feet, slightly on the left.





Fig. 2.5
Hyperextension of the neck for mediastinoscopy

Fig. 2.6
Operative field prepared and draped

Fig. 2.7
Access to a foot vein for fast infusion of fluids or blood in case of haemorrhage from a mediastinal vessel

Fig. 2.8
Access to a hand vein and pulse metre in one finger for intraoperative control of compression of the innominate artery
A 5-cm collar incision is performed immediately cranial to the sternal notch. A low cervical incision gains a few centimetres and allows the mediastinoscope to be inserted more deeply into the mediastinum. The incision is carried out through the subcutaneous tissue and the platysma. Anterior jugular veins in the midline can be ligated if they interfere with the dissection. The pretracheal muscles are separated laterally with Farabeuf retractors. If the thyroid grand is found in the midline, it can be retracted cranially to expose the trachea. At this point, the anterior tracheal wall is identified. The pretracheal fascia is held with forceps and incised with scissors (Fig. 2.9). An index finger is inserted into the incision, anterior to the trachea, and the pretracheal fascia is torn as caudally as the finger allows (Fig. 2.10).
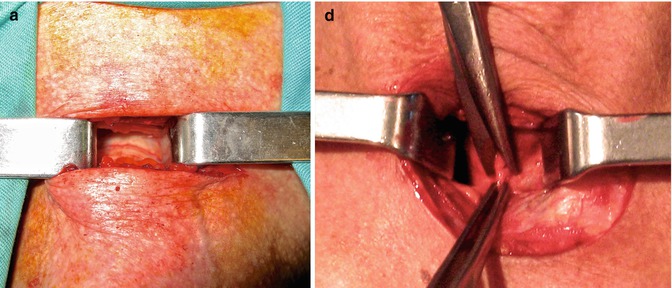

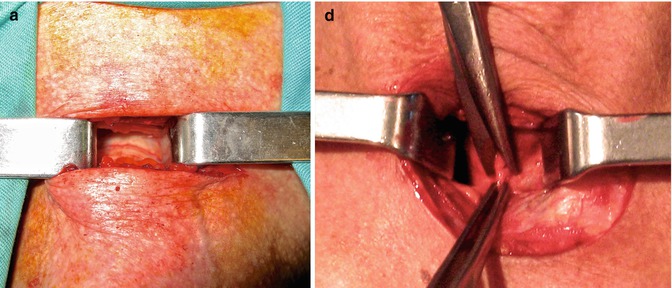
Fig. 2.9
(a) Anterior wall of the trachea and (b) incision of the pretracheal fascia

Fig. 2.10
Finger dissection and palpation of the pretracheal space
This initial palpation with the index finger should be able to identify the pulse of the innominate artery, anteriorly and on the right, as well as that of the aortic arch, in the midline and on the left. The finger separates the peritracheal fatty tissue from the anterior and lateral walls of the trachea; feels the consistency and adhesion of the surrounding tissues, tumours or lymph nodes; and creates a pretracheal space for the insertion of the mediastinoscope.
The mediastinoscope is inserted along the anterior wall of the trachea. When the neck is hyperextended, the mediastinoscope is inserted parallel to the trachea. In case of neck rigidity, the mandible interferes with the mediastinoscope, but it still can be inserted in a more perpendicular way to direct its tip to the target lesion (Fig. 2.11). In patients with laryngectomy and tracheostomy, the cervical incision is performed caudal to the tracheostomy, and the mediastinoscope is inserted as in a regular case (Fig. 2.12). From this point on, the exploration is performed much more comfortably if the surgeon sits on a chair at the patient’s head, and the height of the operating table is at a lower level than the surgeon’s shoulders to avoid any strain on the surgeon’s shoulders and elbows. The pulsation of the innominate artery and of the ascending aorta should be identified. The pretracheal fascia is then further dissected caudally with the dissection-coagulation-suction device till the carina and both main bronchi are clearly seen. In most cases, dissection can be followed along the whole length of both main bronchi. On the right, the azygos vein should be identified at the tracheobronchial angle. This is an important landmark, because, according to the lymph node map proposed by the International Association for the Study of Lung Cancer, nodes caudal to the lower rim of the azygos vein are now called, for taxonomical reasons and for prospective evaluation, hilar nodes although they are located in the mediastinum [55] (Fig. 2.13 and Table 2.1). The right pulmonary artery runs anterior to the subcarinal space and can be followed over the right main bronchus. The left pulmonary artery is identified over the left main bronchus, and nodes caudal to its upper rim are called hilar nodes [55]. The dissection already performed to identify these anatomical landmarks of the superior mediastinum allows the surgeon to assess the peritracheal tissues, to see the mediastinal lymph nodes, mediastinal tumours or any other lesions that are the target of the exploration.
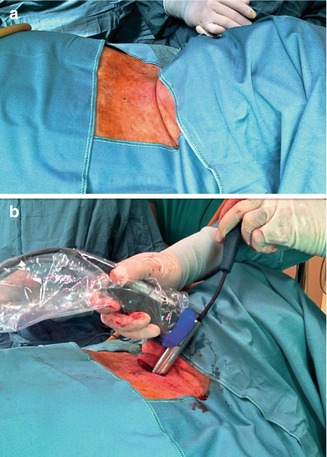
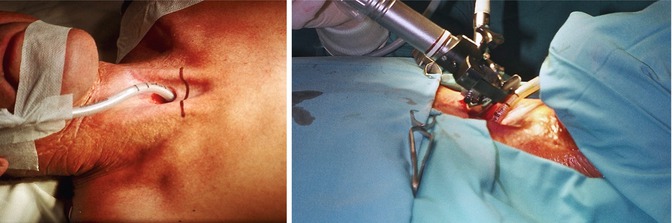
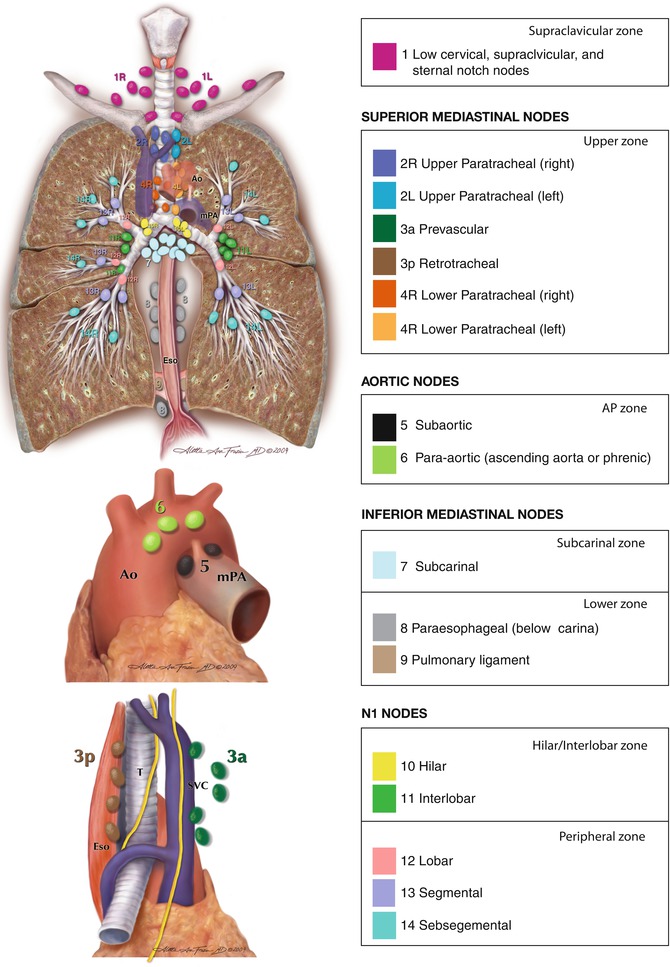
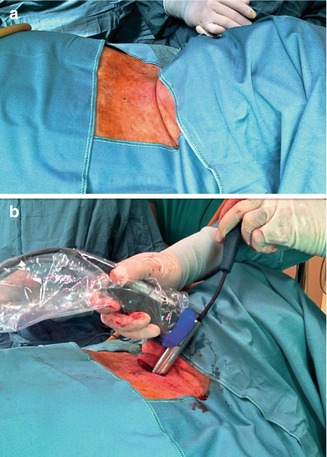
Fig. 2.11
Insertion of the mediastinoscope in a rigid neck. The mediastinoscope is inserted in a more perpendicular way to the trachea than in patients with good neck hyperextension
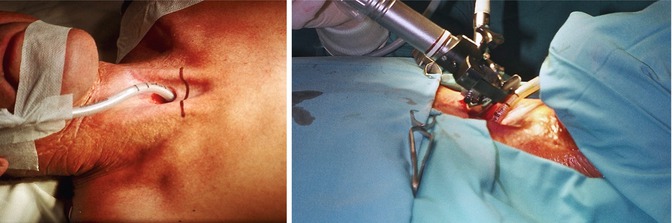
Fig. 2.12
Mediastinoscopy in a patient with total laryngectomy and tracheostomy
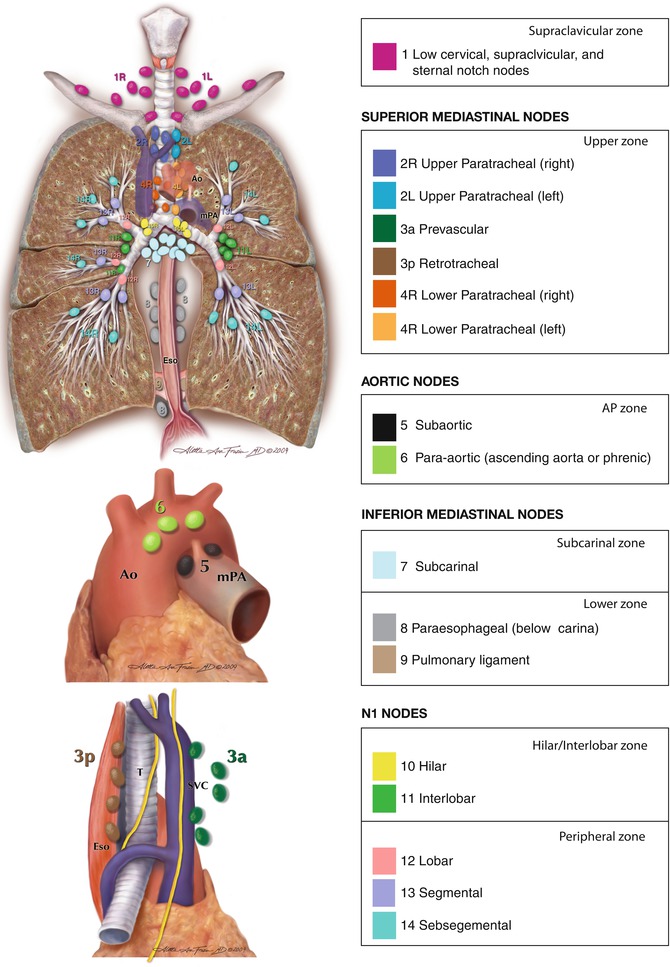
Fig. 2.13
International Association for the Study of Lung Cancer lymph node map (Reproduced with permission from Rusch et al. [55]. Copyright © 2009 Aletta Ann Frazier, MD)
Table 2.1
Anatomical limits for each lymph node station and station grouping by nodal zones in the map proposed by the International Association for the Study of Lung Cancer
Lymph node station | Anatomical limits |
|---|---|
Supraclavicular zone | |
#1: Low cervical, supraclavicular and sternal notch nodes | Upper border: lower margin of cricoid cartilage |
Lower border: clavicles bilaterally and, in the midline, the upper border of the manubrium. 1R designates right-sided nodes, 1L left-sided nodes in this region | |
For lymph node station 1, the midline of the trachea serves as the border between 1R and 1L | |
Upper zone | |
#2: Upper paratracheal nodes | 2R: Upper border: apex of the right lung and pleural space and, in the midline, the upper border of the manubrium |
Lower border: intersection of caudal margin of innominate vein with the trachea | |
As for lymph node station 4R, 2R includes nodes extending to the left lateral border of the trachea | |
2L: Upper border: apex of the lung and pleural space and, in the midline, the upper border of the manubrium | |
Lower border: superior border of the aortic arch | |
#3 Prevascular and retrotracheal nodes | 3a: Prevascular |
On the right: upper border: apex of chest. Lower border: level of carina Anterior border: posterior aspect of sternum. Posterior border: anterior border of superior vena cava | |
On the left: upper border: apex of chest. Lower border: level of carina. Anterior border: posterior aspect of sternum. Posterior border: left carotid artery | |
3p: Retrotracheal | |
Upper border: apex of chest. Lower border: carina | |
#4: Lower paratracheal nodes | 4R: includes right paratracheal nodes and pretracheal nodes extending to the left lateral border of the trachea |
Upper border: intersection of caudal margin of innominate vein with the trachea | |
Lower border: lower border of the azygos vein | |
4L: includes nodes to the left of the left lateral border of the trachea, medial to the ligamentum arteriosum | |
Upper border: upper margin of the aortic arch | |
Lower border: upper rim of the left main pulmonary artery | |
Aortopulmonary zone | |
#5: Subaortic (Aortopulmonary window) | Subaortic lymph nodes lateral to the ligamentum arteriosum |
Upper border: the lower border of the aortic arch | |
Lower border: upper rim of the left main pulmonary artery | |
#6: Para-aortic nodes (ascending aorta or phrenic) | Lymph nodes anterior and lateral to the ascending aorta and aortic arch |
Upper border: a line tangential to the upper border of the aortic arch | |
Lower border: the lower border of the aortic arch | |
Subcarinal zone | |
#7: Subcarinal nodes | Upper border: the carina of the trachea |
Lower border: the upper border of the lower lobe bronchus on the left; the lower border of the bronchus intermedius on the right | |
Lower zone | |
#8: Para-oesophageal nodes (below carina) | Nodes lying adjacent to the wall of the oesophagus and to the right or the left of the midline, excluding subcarinal nodes |
Upper border: the upper border of the lower lobe bronchus on the left; the lower border of the bronchus intermedius on the right | |
Lower border: the diaphragm | |
#9: Pulmonary ligament nodes | Nodes lying within the pulmonary ligament |
Upper border: the inferior pulmonary vein | |
Lower border: the diaphragm | |
Hilar/interlobar zone | |
#10: Hilar nodes | Includes nodes immediately adjacent to the mainstem bronchus and hilar vessels including the proximal portions of the pulmonary veins and main pulmonary artery |
Upper border: the lower rim of the azygos vein in the right; upper rim of the pulmonary artery on the left | |
Lower border: interlobar region bilaterally | |
#11: Interlobar nodes | Between the origin of the lobar bronchi |
a#11s: between the upper lobe bronchus and bronchus intermedius on the right | |
a#11i: between the middle and lower bronchi on the right | |
Peripheral zone | |
#12: Lobar nodes | Adjacent to the lobar bronchi |
#13: Segmental nodes | Adjacent to the segmental bronchi |
#14: Subsegmental nodes | Adjacent to the subsegmental bronchi |
With the mediastinoscope, the following mediastinal nodal stations can be reached: supraclavicular, right and left superior and inferior paratracheal, right and left hilar and subcarinal. Quite often, the para-oesophageal nodes can also be removed or biopsied (Fig. 2.13 and Table 2.1). However, the thoroughness of mediastinoscopy depends on its objective. For diagnostic purposes, biopsy of the abnormal lesions might be enough for pathological studies or culture. For nodal staging in cases of bronchogenic carcinoma with abnormal lymph nodes on CT or PET, biopsy of the abnormal contralateral nodes to prove N3 disease may be enough, unless special studies or protocols require a more thorough exploration. For abnormal ipsilateral nodes to the tumour, biopsy of the abnormal nodes to confirm N2 disease has to be complemented with the assessment of the contralateral nodes to confirm or rule out N3 disease; otherwise, it may pass unnoticed. The ESTS recommends to explore and to take biopsies of the right and left inferior paratracheal lymph nodes and of the subcarinal lymph nodes for a mediastinoscopy to be considered acceptable in standard clinical practice [30]. However, biopsies from these three nodal stations may be insufficient for patients in whom the mediastinum looks normal on CT and PET but require mediastinoscopy for other indications. For these patients, the revised ESTS guidelines recommend the use of the video-mediastinoscope and to perform lymphadenectomy instead of taking biopsies of a few nodes. The idea behind this recommendation is to identify nodal disease that may be missed if only a few nodes are biopsied or removed [56].
Biopsies of tumours or lymph nodes are taken with biopsy forceps. Tissues must be well dissected and identified before biopsies are taken. Mediastinal lymph nodes are black or dark blue, and veins may be mistaken for nodes. In case of doubt, it is advisable to puncture the structure to be biopsied with a needle attached to a glass tube connected to suction and see if blood comes out of it. If blood is seen in the tube, the needle is withdrawn, and the puncture site compressed with gauze for a few minutes. If there is no bleeding, then the biopsy can be taken safely. This manoeuvre is not so necessary if the video-mediastinoscope is used, because structures can be better recognised. During dissection with the dissection-suction-coagulation device, small lymph nodes or nodal fragments can be aspirated. If these samples are considered important for diagnosis, the aspirate can be filtered at the end of the operation, and the samples recovered for pathological study (Fig. 2.14). Quantification of nodal disease has prognostic implications [57]. To facilitate the counting of explored and involved lymph nodes, each removed node or all the fragments of a single node are kept in an individual container that is labelled with the name of the patient and the name or the number of the nodal station (Fig. 2.15).



Fig. 2.14
The aspirate obtained during mediastinoscopy is filtered at the end of the operation, and aspirated fragments are recovered

Fig. 2.15
Each container has one complete lymph node or fragments of the same lymph node. In this particular case, 20 nodes were removed or biopsied: six from the right inferior paratracheal nodal station (#4R), seven from the left inferior paratracheal nodal station (#4L), two from the subcarinal nodal station (#7), two from the subaortic nodal station (#5) and three from the left para-oesophageal nodal station (#8L)
All biopsy sites should be controlled for haemostasis before closing. The azygos vein, the superior vena cava, the small tributary veins to the superior vena cava, the pulmonary arteries and the bronchial arteries should be carefully checked. Gauze compression for a few minutes is usually enough to control small blood oozing from fatty tissue. To avoid tumour implantation in the cervical incision, the biopsy specimens and the gauzes used for haemostasis must be removed along the mediastinoscope to minimise contact with the incision (Fig. 2.16).
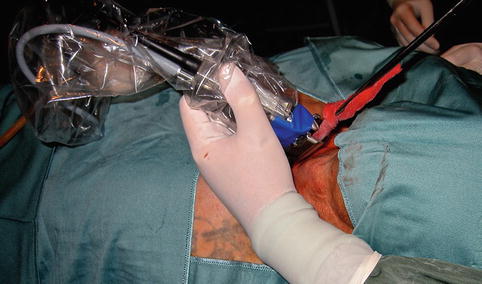
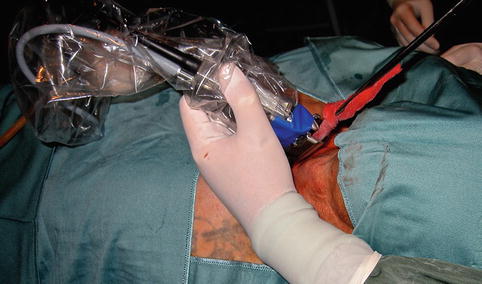
Fig. 2.16
Removal of a gauze along the mediastinoscope avoiding contact with the cervical incision
For closure, the pretracheal muscles are not sutured to the midline, and the incision is closed in two layers: platysma and subcutaneous tissue together with absorbable 2-0 sutures and the skin with intradermal absorbable 3-0 sutures.
Patients are usually awakened and extubated in the operating room and taken to the recovery room till they are fully awake. Oral intake can be restarted 6 h after the operation. If the hospital has an outpatient surgery programme, the patient can be sent home. Readmission rate ranges from 1 to 5 %, mainly because of supraventricular arrhythmias and pneumothorax [58–61]. Postoperative chest x-rays are not required unless the patient has respiratory symptoms, the mediastinal pleura was opened or bleeding occurred during the procedure.
2.5.3 Technical Variants
From the cervical incision, the mediastinoscope can be slipped behind the sterno-clavicular insertions of the sternocleidomastoid muscle to reach the scalene fat pad [62]. This topic is covered in Chap. 1 of this book.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


