The future of cardiology rests in the hands and minds of cardiovascular trainees and fellowship programs. Education and training is rapidly changing, and the paradigm of “see one, do one, teach one” has now been replaced by formal assessments of competency, the incorporation of practice improvement and systems-based practice, and a focus on duty hours. To keep up with the expanding knowledge and science in cardiovascular medicine, the cardiology community needs to understand new educational initiatives and formulate pathways to teach, mentor, and educate trainees to become competent cardiovascular specialists. The author highlights some of the present and future issues facing cardiovascular training.
Over the past decade, there has been an explosion of cardiovascular science and technology. We have also witnessed unprecedented shifts in graduate medical education, notably from passive to active learning and from global to focused assessment of knowledge gaps. The paradigm of physician training is undergoing a sea change, from a “see one, do one, teach one” mentality to a comprehensive, competency-based curriculum and evaluation. Will this new education structure lead to better trained physicians and improved patient outcomes? Nobody knows, at least not yet. What is clear, however, is that change in postgraduate education is here to stay.
Cardiovascular Training Today: An Overview
Fellowship training in cardiology remains highly sought after, rigorous, and complex. American Board of Internal Medicine (ABIM) board eligibility in internal medicine is a requirement to commence fellowship training, and the number of cardiovascular trainees and fellowship training programs in the United States has been stable over the years. According to the 2010 National Resident Matching Program statistics, there are 169 cardiovascular training programs with 1,184 applicants for 718 available positions. Fellowship programs are often limited in the number of training spots, because of the availability of funding as well as key clinical faculty mentors. Typically, 2/3 of the matched applicants are graduates of American medical schools, and <20% are women. Nearly all the available spots for cardiology fellowships are filled during the match; the remaining coveted positions are quickly taken after a brief postmatch scramble.
Presently, applicants for fellowship, typically second-year internal medicine residents, apply to fellowship programs via the Electronic Residency Application Service. This electronic server allows applicants to send a common application to programs with a single mouse click, thereby allowing applicants to apply to a variety of programs. Since its institution, the number of applicants per program has increased substantially. A typical internal medicine applicant has roughly 16 months from the beginning of internship to decide on a fellowship track, seek out mentors and participate in research, obtain letters of recommendation, and submit an application resulting in commencement of training >1 year later. Some applicants chose to apply during their third year of internal medicine residency or beyond, which allows more time to mature in their clinical or research roles but leads to delays in beginning specialty training.
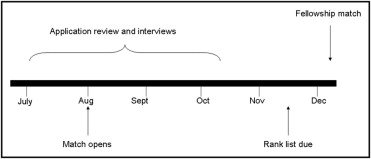
Recently, on the basis of recommendations from a variety of societies and interested parties, a new scheme for specialty fellowship has been developed that delays the National Resident Matching Program specialty match until the late fall of the applicants’ final year of residency ( Figure 1 ) . This new timeline will allow trainees to gather more experience and training programs to more accurately estimate their own needs. Opposition to this change in timing of the match has raised concern over the shortened time between the match and having to potentially move to a new city, limited time to obtain medical licensure and visas, and difficulty in finding staff to interview in the late summer and fall months. Nevertheless, the amended specialty National Resident Matching Program dates will begin July 2012.
Fellowship in cardiovascular medicine presently encompasses 3 to 4 years of full-time training ( Figure 2 ) . Fellows participate in core training in general cardiology as well as each of the subsections within cardiology, including cardiac catheterization, imaging, electrophysiology, vascular, heart failure, research, and elective. There is now renewed interest in the possibility of blending the third year of internal medicine residency with cardiovascular training, and the ABIM is considering beginning a few pilot programs to test the concept. This would shorten total training time of internal medicine plus cardiology from 6 to 5 years. Certain issues remain, such as the recruitment of early-track fellows as well as the possible detrimental effects this might have on internal medicine training and their programs.
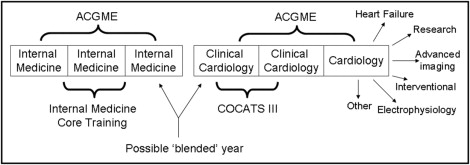
The Accreditation Council for Graduate Medical Education (ACGME) requires 24 months of clinical training in cardiovascular medicine and 3 years of continuity clinic. Thereafter, trainees are ABIM board eligible for the cardiovascular medicine certification examination. In addition to the ACGME and ABIM, there are numerous stakeholders in the fellowship training process, which often leads to some confusion as to what exactly is expected from trainees and programs ( Figure 3 ) . After general cardiovascular training, fellows may then choose to subspecialize in a variety of areas requiring further years of education and training. Many of these specialized training tracks are sanctioned by the ABIM (electrophysiology, interventional cardiology, heart failure), while others are not (advanced imaging, vascular, research).

During the final stages of fellowship, trainees focus on getting jobs as cardiovascular specialists. This can be a daunting experience and is often the first job search for many. Approximately 2/3 of the present cardiology workforce is composed of general cardiologists, while the remaining 1/3 includes interventional, electrophysiology, and pediatric specialists. Despite the present-day contraction of the private practice of cardiology, there is still considerable need for clinical cardiologists in the United States. Because of increasing rates of cardiovascular disease in the United States with an aging population, there is increasing demand for cardiac specialists, and it is estimated that roughly twice the number of cardiac specialists will be needed by 2050. However, it will be hard, if not impossible, to meet these demands given the present financial constraints that academic centers are under regarding postgraduate training. The ever increasing cost of medical school is also an important issue to consider, and it is estimated that >20% of medical students graduate with >$200,000 of debt. Thus, to spend ≥6 years in cardiovascular training, as well as decreasing reimbursement for procedures, may be viewed as a disincentive, often pointing potential cardiologists toward different careers.
Accreditation Council for Graduate Medical Education Regulations and Fellowship Training
The ACGME evaluates, accredits, and oversees medical training programs in the United States, and its mission is to improve health care by “assessing and advancing the quality of resident physicians education through accreditation” and to ensure quality during the learning and training experience. The ACGME establishes guidelines for programs and surveys fellows and programs periodically to ensure compliance and obtain feedback. ACGME regulations, along with the ABIM, societies, local, state, and national organizations, and graduate medical education offices, provide a framework for fellowship programs and allows consistency in training ( Figure 3 ).
The present ACGME model is based on 6 broad competencies for medical training and education ( Table 1 ), and the specialty requirements are structured along these lines. Fellows are expected to learn information, translate knowledge into clinical practice, act maturely, develop relations with staff members and patients, understand ways to evaluate and improve care, and work within an ever changing medical environment. The competencies are meant to be a framework used in all aspects of training, including written curricula and evaluations, and provide structure for training programs to standardize education. Adherence to this model and documentation is a major focus of the ongoing accreditation and review process.
| Competency | Description |
|---|---|
| Patient care | Compassionate, appropriate, effective care for the treatment of health problems and the promotion of health |
| Medical knowledge | Established and evolving biomedical, clinical, and cognate sciences and the application of this knowledge to patient care |
| Professionalism | Commitment to carrying out professional responsibilities, adherence to ethical principles, and sensitivity to a diverse patient population |
| Interpersonal and communication skills | Effective information exchange and teaming with patients, their families, and other health professionals |
| Practice-based learning and improvement | Investigation and evaluation of patient care, appraisal and assimilation of scientific evidence, and improvements in patient care |
| Systems-based practice | Awareness of and responsiveness to the larger context and system of health care and the ability to effectively call on system resources to provide care that is of optimal value |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


