The comparative effectiveness of angiotensin-converting enzyme (ACE) inhibitors versus angiotensin II type 1 receptor blockers (ARBs) in real-world older heart failure (HF) patients remains unclear. Of the 8,049 hospitalized HF patients aged ≥65 years discharged alive from 106 Alabama hospitals, 4,044 received discharge prescriptions of either ACE inhibitors (n = 3,383) or ARBs (n = 661). Propensity scores for ARB use, calculated for each of 4,044 patients, were used to match 655 (99% of 661) patients receiving ARBs with 661 patients receiving ACE inhibitors. The assembled cohort of 655 pairs of patients was well balanced on 56 baseline characteristics. During >8 years of follow-up, all-cause mortality occurred in 63% and 68% of matched patients receiving ARBs and ACE inhibitors, respectively (hazard ratio [HR] associated with ARB use 0.86, 95% confidence interval [CI] 0.75 to 0.99, p = 0.031). Among the 956 matched patients with data on the left ventricular ejection fraction (LVEF), the association between ARB (vs ACE inhibitor) use was significant in only 419 patients with LVEFs ≥45% (HR 0.65, 95% CI 0.51 to 0.84, p = 0.001) but not in the 537 patients with LVEFs <45% (HR 1.00, 95% CI 0.81 to 1.23, p = 0.999; p for interaction = 0.012). HRs for HF hospitalization associated with ARB use were 0.99 (95% CI 0.86 to 1.14, p = 0.876) overall, 0.80 (95% CI 0.63 to 1.03, p = 0.080) in those with LVEFs ≥45%, and 1.14 (95% CI 0.91 to 1.43, p = 0.246) in those with LVEFs <45% (p for interaction = 0.060). In conclusion, in older HF patients with preserved LVEFs, discharge prescriptions of ARBs (vs ACE inhibitors) were associated with lower mortality and a trend toward lower HF hospitalization, findings that need replication in other HF populations.
Most heart failure (HF) patients are older adults, and HF is the leading cause of hospitalization for older Medicare beneficiaries. Inhibition of the renin-angiotensin system by angiotensin-converting enzyme (ACE) inhibitors or angiotensin II type 1 receptor blockers (ARBs) forms the foundation of the evidence-based therapy for patients with HF and reduced ejection fractions. National HF guidelines vary in their recommendations regarding whether ACE inhibitors or ARBs should be used as the drugs of first choice. The efficacy of ACE inhibitors and ARBs has been compared in randomized clinical trials of patients with HF and reduced ejection fractions and those with post–myocardial infarction left ventricular systolic dysfunction. However, these randomized clinical trials have often excluded older HF patients and those with HF with preserved ejection fraction (HF-PEF). In the present study, we examined the comparative effectiveness of ACE inhibitors versus ARBs on outcomes in real-world older HF patients with reduced or preserved ejection fractions.
Methods
The present study was based on the Alabama Heart Failure Project registry, which has been previously described. Briefly, the Alabama Heart Failure Project was conducted by AQAF, Alabama’s quality improvement organization, as a quality improvement project. Extensive data on baseline demographics, medical history including the use of medications, hospital course, discharge disposition including medications, and physician specialty were collected via chart abstraction from 8,555 patients discharged from 106 Alabama hospitals with primary discharge diagnoses of HF from 1998 to 2001. Of the 8,555 patients, 8,049 were discharged alive. After excluding patients receiving both ACE inhibitors and ARBs (n = 93) and those receiving neither of these drugs (n = 3,314), the study sample consisted of 4,642 patients, of whom 4,044 (87%) were aged ≥65 years. Discharge prescriptions of ACE inhibitors were given to 3,383 patients (84%), and 661 patients (16%) received discharge prescriptions of ARBs. Lisinopril was the most common ACE inhibitor (30% [1,028 of 3,383]), and losartan was the most common ARB (57% [378 of 661]).
The study was designed using propensity score matching to assemble a balanced cohort in which patients receiving ACE inhibitors and ARBs would be balanced on baseline characteristics. The probability for the receipt of ARBs was estimated for each of the 4,044 patients using a nonparsimonious multivariate logistic regression model in which the receipt of ARBs was the dependent variable and 56 baseline characteristics were used as covariates. We then used a greedy matching protocol, enabling us to match 655 of the 661 patients receiving ARBs with 655 patients receiving ACE inhibitors, thus assembling a cohort of 655 pairs of patients who were well balanced on all 56 measured baseline characteristics.
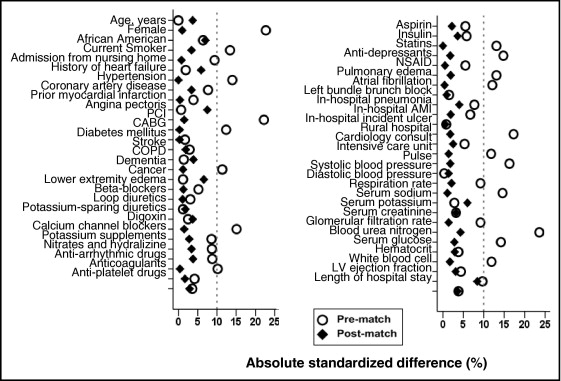
Baseline characteristics were compared using Pearson’s chi-square and Wilcoxon’s rank-sum tests for the prematch data and McNemar’s test and paired-samples Student’s t tests for postmatch comparisons, as appropriate. Absolute standardized differences that directly quantified bias in the means (or proportions) of covariates across the 2 treatment groups were estimated and findings expressed as percentages of the pooled standard deviations were presented as Love plots. Kaplan-Meier plots and Cox regression analyses were used to determine the association of discharge prescription of ARBs versus ACE inhibitor use with all-cause mortality and hospitalization during >8 years of follow-up. A formal sensitivity analysis was conducted to quantify the degree of a hidden bias that would be required to explain away a significant association among matched patients. Additional sensitivity analyses were conducted using multivariate-adjusted (using all covariates used in the propensity model) and propensity-adjusted Cox regression models using prematch data of 4,044 patients. All statistical tests were 2 tailed, with p values <0.05 considered significant. SPSS for Windows version 18 (SPSS, Inc., Chicago, Illinois) was used for data analysis.
Results
Overall, matched patients (n = 1,310) had a mean age of 78 ± 7 years, 69% were women, and 19% were African American. Imbalances in baseline characteristics before matching and balances achieved after matching between patients prescribed ACE inhibitors and ARBs at discharge are listed in Table 1 and shown in Figure 1 . Before matching, patients prescribed ARBs were more likely to be women and had a higher prevalence of hypertension and coronary revascularization, a lower prevalence of atrial fibrillation and renal insufficiency, and a similar prevalence of coronary artery disease and diabetes mellitus. They were also less likely to receive digoxin, but they had no differences in the receipt of other drugs, such as diuretics and β blockers. However, these differences were balanced after matching. Postmatch Love plot data suggested substantial covariate balance across the groups for all measured covariates (i.e., absolute standardized differences <10% for all covariates after matching; Figure 1 ).
| Variable | Prematch | Postmatch | ||||
|---|---|---|---|---|---|---|
| ACE Inhibitors (n = 3,383) | ARBs (n = 661) | p Value | ACE Inhibitors (n = 655) | ARBs (n = 655) | p Value | |
| Age (years) | 78 ± 8 | 78 ± 7 | 0.998 | 78 ± 8 | 78 ± 7 | 0.505 |
| Women | 1,994 (59%) | 461 (70%) | <0.001 | 452 (69%) | 455 (70%) | 0.857 |
| African Americans | 770 (23%) | 133 (20%) | 0.136 | 115 (18%) | 133 (20%) | 0.204 |
| Current smokers | 314 (10%) | 38 (6%) | 0.277 | 33 (5%) | 38 (6%) | 0.542 |
| Nursing home residents | 214 (6%) | 28 (4%) | 0.003 | 27 (4%) | 28 (4%) | 0.890 |
| Medical history | ||||||
| Previous HF | 2,470 (73%) | 477 (72%) | 0.654 | 491 (75%) | 474 (72%) | 0.286 |
| Hypertension | 2,436 (72%) | 516 (78%) | 0.001 | 510 (78%) | 510 (78%) | 1.000 |
| Coronary artery disease | 1,851 (55%) | 387 (59%) | 0.070 | 370 (57%) | 381 (58%) | 0.539 |
| Percutaneous coronary intervention | 407 (12%) | 133 (20%) | <0.001 | 132 (20%) | 128 (20%) | 0.782 |
| Coronary artery bypass graft | 793 (23%) | 191 (29%) | 0.003 | 186 (28%) | 187 (29%) | 0.951 |
| Diabetes mellitus | 1,456 (43%) | 290 (44%) | 0.692 | 286 (44%) | 287 (44%) | 0.956 |
| Atrial fibrillation | 995 (29%) | 159 (24%) | 0.005 | 157 (24%) | 158 (24%) | 0.948 |
| Dementia | 319 (9%) | 42 (6%) | 0.011 | 44 (7%) | 42 (6%) | 0.823 |
| Cancer | 76 (2%) | 16 (2%) | 0.784 | 10 (2%) | 16 (1%) | 0.815 |
| Clinical findings | ||||||
| Pulse (beats/min) | 89 ± 23 | 86 ± 22 | <0.001 | 86 ± 21 | 86 ± 22 | 0.746 |
| Systolic blood pressure (mm Hg) | 152 ± 32 | 152 ± 31 | 0.945 | 153 ± 31 | 152 ± 31 | 0.803 |
| Diastolic blood pressure (mm Hg) | 81 ± 19 | 79 ± 19 | 0.031 | 79 ± 18 | 79 ± 19 | 0.699 |
| Respiration (breaths/min) | 24 ± 6 | 23 ± 6 | 0.001 | 23 ± 6 | 23 ± 6 | 0.836 |
| Peripheral edema | 2,341 (69%) | 473 (72%) | 0.228 | 463 (71%) | 467 (71%) | 0.808 |
| Pulmonary edema by chest x-ray | 2,348 (69%) | 418 (63%) | 0.002 | 421 (64%) | 415 (63%) | 0.730 |
| Laboratory data | ||||||
| Serum sodium (mEq/L) | 139 ± 5 | 139 ± 5 | 0.520 | 138 ± 5 | 138 ± 5 | 0.280 |
| Serum potassium (mEq/L) | 4.3 ± 0.6 | 4.2 ± 0.6 | 0.460 | 4.3 ± 0.7 | 4.2 ± 0.6 | 0.565 |
| Serum creatinine (mEq/L) | 1.4 ± 0.9 | 1.5 ± 0.9 | 0.029 | 1.45 ± 0.8 | 1.5 ± 0.9 | 0.794 |
| Estimated glomerular filtration rate (ml/min/1.73 m 2 ) | 57 ± 26 | 51 ± 20 | <0.001 | 51 ± 19 | 51 ± 20 | 0.438 |
| Blood urea nitrogen (mg/dl) | 25 ± 14 | 27 ± 15 | 0.001 | 27 ± 16 | 27 ± 15 | 0.607 |
| Serum glucose (mg/dl) | 152 ± 69 | 149 ± 68 | 0.371 | 151 ± 73 | 149 ± 68 | 0.595 |
| Hematocrit (%) | 37 ± 6 | 36 ± 6 | 0.005 | 37 ± 5 | 36 ± 6 | 0.763 |
| White blood cell count (×10 3 /μl) | 9 ± 5 | 9 ± 4 | 0.345 | 9 ± 3 | 9 ± 4 | 0.581 |
| LVEF | ||||||
| <45% | 1,477 (44%) | 257 (39%) | 0.025 | 282 (43%) | 255 (39%) | 0.782 |
| ≥45% | 967 (28%) | 221 (33%) | 201 (31%) | 218 (33%) | ||
| Unknown | 939 (28%) | 183 (28%) | 172 (26%) | 182 (28%) | ||
| Hospital and care characteristics | ||||||
| Incident pneumonia | 837 (25%) | 142 (22%) | 0.074 | 152 (23%) | 141 (22%) | 0.466 |
| Incident acute myocardial infarction | 139 (4%) | 19 (3%) | 0.134 | 17 (3%) | 19 (3%) | 0.735 |
| Incident pressures ulcer | 253 (8%) | 48 (7%) | 0.846 | 47 (7%) | 48 (7%) | 0.915 |
| Rural hospital | 1,108 (33%) | 165 (25%) | <0.001 | 160 (24%) | 165 (25%) | 0.749 |
| Cardiology consult | 1,815 (54%) | 372 (57%) | 0.215 | 359 (55%) | 367 (56%) | 0.657 |
| Intensive care unit | 96 (3%) | 34 (5%) | 0.002 | 31 (5%) | 33 (5%) | 0.798 |
| Length of stay (days) | 6 ± 5 | 6 ± 4 | 0.380 | 6.3 ± 3.8 | 6.4 ± 4.3 | 0.515 |
| Discharge medications | ||||||
| β blockers (heart failure) | 774 (23%) | 160 (24%) | 0.459 | 162 (25%) | 159 (24%) | 0.847 |
| Loop diuretics | 2,961 (88%) | 576 (87%) | 0.784 | 574 (88%) | 570 (87%) | 0.740 |
| Digoxin | 1,729 (51%) | 228 (44%) | <0.001 | 293 (45%) | 288 (44%) | 0.781 |
| Potassium-sparing diuretics | 542 (16%) | 112 (17%) | 0.556 | 102 (16%) | 111 (17%) | 0.500 |
| Potassium supplements | 1,629 (48%) | 347 (53%) | 0.041 | 354 (54%) | 343 (52%) | 0.542 |
All-cause mortality occurred in 63% and 68% of matched patients receiving ARBs and ACE inhibitors, respectively (hazard ratio [HR] for ARB use vs ACE inhibitor use 0.86, 95% confidence interval [CI] 0.75 to 0.99, p = 0.031; Table 2 , Figure 2 ). A hidden covariate that is a near perfect predictor of mortality would need to decrease the odds of discharge prescription of ARBs by 7.7% to potentially explain away this association. Among the 956 matched patients with data on the ejection fraction, the association between ARB use (vs ACE inhibitor use) was significant in only 419 patients with left ventricular ejection fractions (LVEFs) ≥45% (HR 0.65, 95% CI 0.51 to 0.84, p = 0.001; Figure 2 ) but not in the 537 patients with LVEFs <45% (HR 1.00, 95% CI 0.81 to 1.23, p = 0.999; Figure 2 ). This difference was statistically significant (p for interaction = 0.012). Multivariate-adjusted and propensity score–adjusted associations of ARB (vs ACE inhibitor) use and all-cause mortality in the 4,044 prematch patients are listed in Table 2 .



