Thoracic Trauma
Trauma is one of the leading causes of death and disability, often affecting young otherwise healthy individuals (1,2). Chest injuries are a significant contributor to trauma-related deaths and disability. After head and neck injuries, which affect the brain and cervical spinal cord, thoracic injuries affect the next most vital structures, including the heart, aorta, lungs, and thoracic spinal cord. This chapter reviews some of the mechanisms of injury to the various organs and structures within the thorax, along with their imaging features and evaluation.
Biomechanics
Thoracic trauma is the result of either penetrating or blunt injuries or a combination of the two. Knife and gunshot wounds are typical examples of penetrating injuries. Motor vehicle accidents, falls from a great height, and direct blows to the chest are common examples of blunt injuries. Explosions can cause combined injuries, with flying debris causing penetrating injuries and the shock wave of the blast causing blunt injuries. Velocity is an important factor contributing to both penetrating and blunt injuries. Relatively slow moving objects, such as knives and clubs, cause limited local injuries along the path of the blade or at the site of impact. Faster moving objects, such as bullets, not only cause damage along their flight paths but can also create compression shock waves, which travel through adjacent tissues and cause additional injuries. High-speed blunt impacts, such as those resulting from motor vehicle accidents or falls, not only cause direct blow injuries, but also result in the variable deceleration of internal structures, leading to shearing stresses and torsional forces at sites of fixation that can lacerate tissues and tear vessels. In addition, sudden or rapid compression of the chest or abdomen can cause an abrupt pressure increase, resulting in rupture of viscera (1,2).
Aortic Injuries
Acute traumatic aortic injury (ATAI) is a devastating and often lethal consequence of thoracic trauma. Proposed mechanisms of injury include the following:
Variable deceleration of the thoracic aorta producing shearing stresses, particularly at points of fixation such as the aortic root, the aortic isthmus (just distal to the left subclavian artery origin near the attachment of the ligamentum arteriosus), and the diaphragmatic hiatus;
Chest or abdominal wall compression, resulting in a sudden increase in the intraaortic pressure;
Chest compression, crushing the aorta between the sternum and spine.
Eighty-five percent of patients with an ATAI will suffer a complete full-thickness tear or rupture of the aortic wall, exsanguinate, and die before reaching the hospital. The remaining 15% of patients with an ATAI will have incomplete partial tears of the aortic wall, forming a pseudoaneurysm. Approximately 50% of these survivors will develop pseudoaneurysm rupture within the first 24 hours after the traumatic event if untreated.
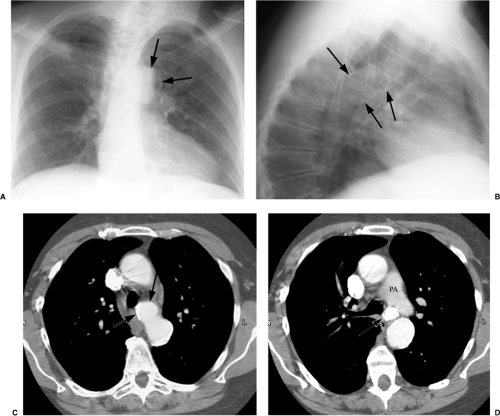
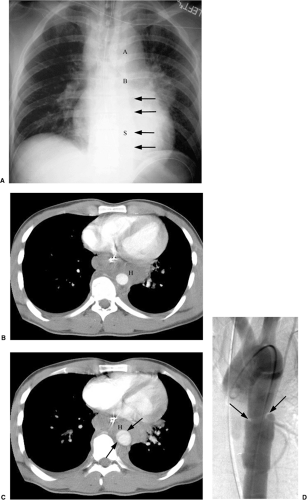
Less than 5% of patients will survive long term with a pseudoaneurysm (3). The chest radiograph and computed tomography (CT) of one such patient with a chronic pseudoaneurysm are shown in Fig. 12.1.
Less than 5% of patients will survive long term with a pseudoaneurysm (3). The chest radiograph and computed tomography (CT) of one such patient with a chronic pseudoaneurysm are shown in Fig. 12.1.
The most common location of traumatic aortic rupture is the aortic root; however, these patients usually do not survive to reach the hospital.
Table 12.1: Chest Radiograph Signs of Mediastinal Hematoma | |
|---|---|
|
ATAI is strongly associated with mediastinal hemorrhage; however, this blood does not arise from the aortic tear itself because the intact adventitia of the pseudoaneurysm maintains aortic integrity and blood flow. The mediastinal hematoma results from concomitant injury to other mediastinal, paraspinal, and intercostal vessels, usually veins and small arteries. Plain chest radiographs do not directly image an aortic tear; only CT and aortography can do this. However, plain films can detect mediastinal hematoma, an indirect sign of ATAI. Therefore, plain films are a useful screening tool and may help guide further imaging evaluation. Although no single plain film finding is totally sensitive or specific for a mediastinal hematoma, the following abnormalities have the greatest diagnostic value: (a) widening of the superior mediastinum; (b) obscuration of the aortic arch; (c) abnormal aortic contour; (d) fullness, opacification, or loss of definition of the aorticopulmonary window; (e) caudal displacement of the left main bronchus; (f) rightward deviation of the trachea; (g) rightward deviation of a nasogastric tube in the esophagus; (h) widening of the paraspinal stripe in the absence of a vertebral fracture; (i) widening of the right paratracheal stripe; and (j) left apical cap and left pleural fluid (Table 12.1) (4). Detection of one or more of these findings should prompt further evaluation with CT aortography. This requires helical CT at a collimation no greater than 3 mm with overlapping reconstructions, coupled with rapid intravenous contrast administration at 4 mL/s.
Direct CT signs of ATAI should be specifically sought and include (a) intraluminal irregularities or areas of low attenuation (polypoid clot, linear-intimal flap), (b) change in caliber of the aorta (pseudoaneurysm, pseudocoarctation), (c) abnormal or irregular aortic wall or contour, (d) abnormal contour of great vessels, and (e) intramural hematoma or dissection (Table 12.2) (5,6). Approximately 90% of these ATAIs should be in the
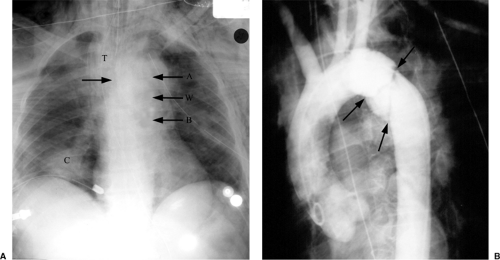
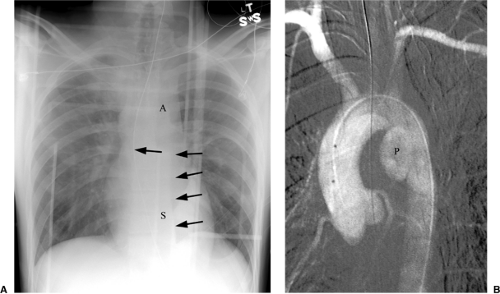
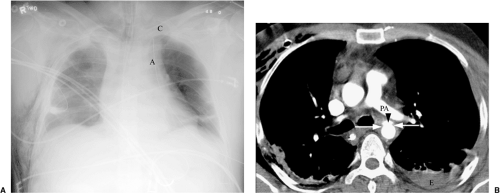
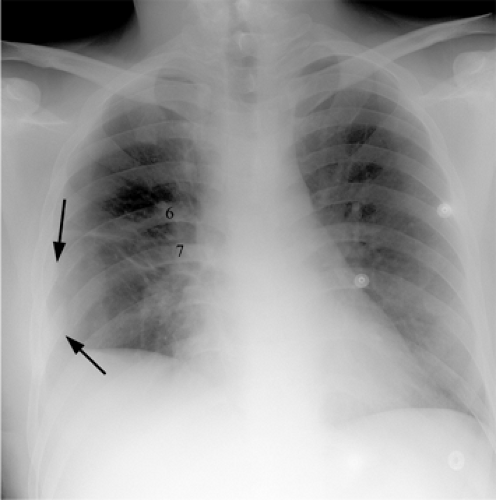
region of the aortic isthmus (3). CT findings of mediastinal fat stranding, mediastinal hemorrhage, perivascular hematoma, and periaortic hematoma are indirect signs of ATAI and are also seen with nonaortic mediastinal injuries. Nonetheless, these findings require clinical follow-up or, in the case of periaortic hematoma, further evaluation with catheter aortography (5). Figures 12.2, 12.3, 12.4 and 12.5 are the chest radiographs and accompanying CTs and/or aortograms from four cases of ATAI. The cases in Figs. 12.2, 12.3 and 12.4 demonstrate the typical location of ATAI at the aortic isthmus, whereas the case in Fig. 12.5 is from the 10% of ATAIs that occur in other locations.
region of the aortic isthmus (3). CT findings of mediastinal fat stranding, mediastinal hemorrhage, perivascular hematoma, and periaortic hematoma are indirect signs of ATAI and are also seen with nonaortic mediastinal injuries. Nonetheless, these findings require clinical follow-up or, in the case of periaortic hematoma, further evaluation with catheter aortography (5). Figures 12.2, 12.3, 12.4 and 12.5 are the chest radiographs and accompanying CTs and/or aortograms from four cases of ATAI. The cases in Figs. 12.2, 12.3 and 12.4 demonstrate the typical location of ATAI at the aortic isthmus, whereas the case in Fig. 12.5 is from the 10% of ATAIs that occur in other locations.
Table 12.2: CT Signs of Acute Traumatic Aortic Injury | ||||||
|---|---|---|---|---|---|---|
| ||||||
The most common location of aortic rupture seen clinically is the proximal descending thoracic aorta at the ligamentum arteriosum.
Osseous Injuries
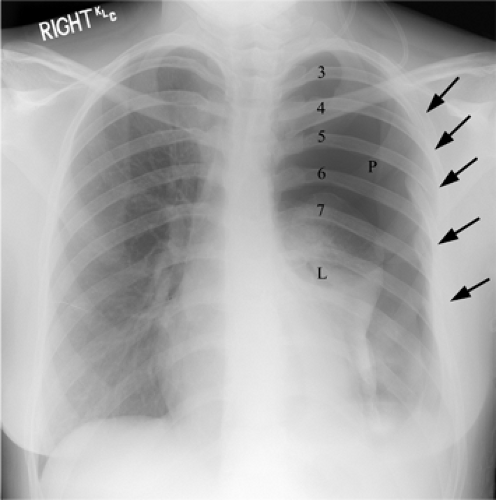
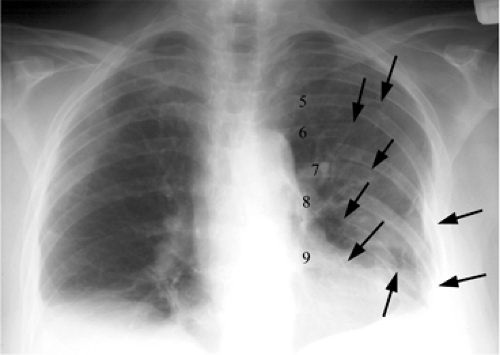
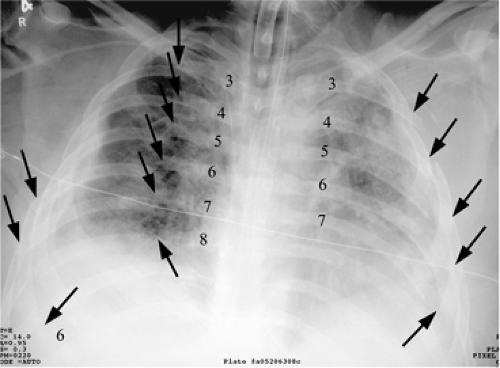
Rib fractures are the most common sequela of chest trauma, occurring in over half of blunt trauma cases (7,8,9). However, many of these injuries are not initially detected because they are uncomplicated nondisplaced fractures or involve radiographically undetectable costochondral separation (2,7,8,10). This is acceptable because the goal of imaging is not so much to detect the rib fracture itself, but rather the potential associated complications of rib fractures (10). These complications include injury to the intercostal vessels, which can lead to hemothorax or an extrapleural hematoma; lung contusion or laceration; pneumothorax; and subcutaneous emphysema (Figs. 12.6 and 12.7) (2,9,10). The most serious consequence of rib fractures is flail chest (2,7). Flail chest is the result of five or more adjacent rib fractures or more than three segmental rib fractures (a single rib fractured in two or more locations) (Figs. 12.8 and 12.9) (2,7,8).
This creates an abnormally mobile segment of the chest wall that will move paradoxically with respiration (2,7,8). Flail chest can lead to respiratory failure in part secondary to associated lung and pleural injuries and in part secondary to pendelluft (2). Pendelluft is the pendulum-like movement of gas from the normal hemithorax to the flail hemithorax during expiration and then back again during inspiration due to the paradoxical motion of the flail segment. In other words, when the normal hemithorax exhales, the flail hemithorax will paradoxically inhale and vice versa. This results in impaired ventilation due to rebreathing of the same air back and forth between the hemithoraces. This can be treated with mechanical ventilation (2,7,8).
This creates an abnormally mobile segment of the chest wall that will move paradoxically with respiration (2,7,8). Flail chest can lead to respiratory failure in part secondary to associated lung and pleural injuries and in part secondary to pendelluft (2). Pendelluft is the pendulum-like movement of gas from the normal hemithorax to the flail hemithorax during expiration and then back again during inspiration due to the paradoxical motion of the flail segment. In other words, when the normal hemithorax exhales, the flail hemithorax will paradoxically inhale and vice versa. This results in impaired ventilation due to rebreathing of the same air back and forth between the hemithoraces. This can be treated with mechanical ventilation (2,7,8).
Fractures of thoracic bones are an indication of the force of trauma and are commonly associated with organ injury.
A fail chest is the fracture of three or more ribs in two or more locations each, or the fracture of five or more adjacent ribs.
Fractures of the first three ribs, particularly the first rib (Fig. 12.10), are a marker of severe trauma (2,7,10). Considerable force is required to break these ribs because they are protected by the clavicle, shoulder, scapula, and heavy surrounding musculature (2,7). These fractures are often associated with airway, spinal, vascular, and brachial plexus injuries. Fractures of the lower three ribs are associated with injuries to the spleen, liver, or kidneys (2,10).
Lower rib fractures are associated with injury to the liver, spleen, and kidneys.
Sternal fractures can result from steering wheel injuries, seat-belt injuries, crush injuries, and aggressive resuscitation (2,8). Sternal fractures can be important because they are associated with other mediastinal injuries; however, they are virtually impossible to detect on frontal radiographs (10). Lateral views or CT are required to detect sternal fractures, which are usually transverse and near the manubrium (2,8,10). Sagittal and/or coronal reconstructions can be useful (8). An associated retrosternal hematoma
is often noted, which if separated from the aorta by a fat plane suggests that the hematoma is not aortic in origin (2,11). Sternoclavicular dislocations can also be detected with CT (8,9).
is often noted, which if separated from the aorta by a fat plane suggests that the hematoma is not aortic in origin (2,11). Sternoclavicular dislocations can also be detected with CT (8,9).
Sternal fractures are associated with mediastinal vascular injury.
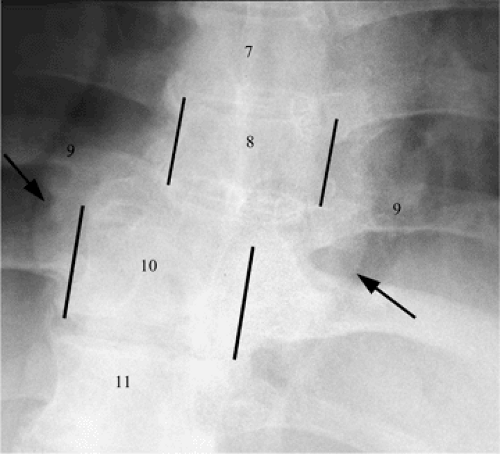
Thoracic vertebral fractures can result from motor vehicle accidents or falls from a great height. They are produced by hyperflexion and/or axial loading and account for 25% to 30% of all spine fractures (1). Most injuries occur at the functional thoracolumbar junction, which extends from T-9 to T-11 (1,7,8,12). The thoracic spinal cord is unusually susceptible to injury. This vulnerability is the result of two main factors. First, the thoracic spinal cord is tightly packed in the spinal canal, predisposing it to injury by displaced fragments of bone or disc material and compression by hematoma and cord edema. Second, the vascular supply to the mid-thoracic cord is quite tenuous and can be disrupted easily, resulting in cord ischemia or infarction with associated neurologic impairment (1). The radiographic findings of thoracic spine fractures can be subtle and difficult to identify (8). Initial evaluation should include the frontal chest radiograph and a cross-table lateral view of the spine. There are both direct and indirect plain film signs of thoracic fractures (Table 12.3). Direct signs include cortical disruption and abnormal vertebral body size, shape, opacity, and location (Fig. 12.11) (1). Indirect signs are secondary to paravertebral hematoma (Fig. 12.5) and can overlap with signs of aortic injury. Indirect signs include widening of the paraspinal stripe, mediastinal widening, left apical cap, and deviation of a nasogastric tube (1,7,8,13). If a thoracic spine fracture is suspected, then further evaluation with CT and/or magnetic resonance imaging (MRI) is indicated. Reformatted sagittal and coronal CT images are helpful (1,8). A mediastinal hematoma that is confined to the posterior compartment suggests a vertebral fracture (8).
A portable chest trauma radiograph may suggest thoracic spine fracture but is insufficient to exclude it.
Table 12.3: Radiographic Findings of Thoracic Spine Fractures | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ||||||||||||
Lung and Pleural Injuries
Contusion in the most common pulmonary parenchymal injury, occurring in approximately half of patients after blunt trauma (2,8,11). The mechanism of injury is local comprehensive and recoil forces within the lung that disrupt small vessels, leading to intraalveolar hemorrhage or a parenchymal bruise (2,9,10,11,14). Interstitial injury with associated capillary leak and edema can also occur but is usually seen with more severe trauma accompanied by blast or shock wave injuries (Fig. 12.12) (14). Contusion appears rapidly and usually reaches its full extent within the first day after trauma (Fig. 12.13). Contusion tends to occur adjacent to solid structure such as the ribs, spine, and solid organs like the heart and liver (2). Contusions may have a varied radiographic appearance, ranging from coarse irregular nodular opacities that may be confluent or discrete to homogenous consolidation with diffuse hazy or focal, poorly defined, fluffy lung opacities, or a combination of these findings (Figs. 12.14 and 12.15) (9,11,14). The presence and extent of
contusion are much better defined with CT than chest radiographs (Figs. 12.14 and 12.15) (2,8,11,14). Contusion may be difficult to distinguish from or may be obscured by other forms of posttraumatic consolidation, including aspiration, edema, and atelectasis (2). Contusion usually begins to resolve within a few days, completely resolving within 1 to 2 weeks (2,8).
contusion are much better defined with CT than chest radiographs (Figs. 12.14 and 12.15) (2,8,11,14). Contusion may be difficult to distinguish from or may be obscured by other forms of posttraumatic consolidation, including aspiration, edema, and atelectasis (2). Contusion usually begins to resolve within a few days, completely resolving within 1 to 2 weeks (2,8).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree