Radiology of the Pleura
Evaluation of the pleura is in several important ways the evil twin of evaluation of the mediastinum. Whereas plain film assessment of the mediastinum is extremely limited, chest radiograph (CXR) evaluation of the pleura is generally efficacious. Although computed tomography (CT) is a phenomenal tool for assessing mediastinal anatomy and abnormality, pleural CT is often requested for indications of questionable validity. In this chapter we discuss typical pleural abnormalities, their differential diagnosis, and applications of CT.
Pleural Abnormalities
The major pleural findings of abnormality are effusion, pneumothorax, focal or multifocal pleural implants or plaques, and solitary or multiple pleural masses.
Pleural Effusion
As discussed in Chapter 3, pleural effusion is typically gravity dependent. It accumulates in the most dependent portion of the chest, varying with changes in patient position. In the presence of pleural adhesions or scars, loculated effusion may occur. Pleural fluid may track into pleural fissures, even when not loculated. Although this is often easily recognizable based on its tapering cigar-shaped appearance (Fig. 17.1), it sometimes results in confusing appearances.
On standard frontal and lateral radiographs, the posterior costophrenic sulcus is the place to look for small pleural effusions. As effusion enlarges, it may blunt the lateral costophrenic angles, or it may accumulate in a subpulmonic location. Neophyte interpreters of radiographs seem to overcall pleural effusions on frontal radiographs more than any other finding. They are quick to assume that any basilar opacity on a portable radiograph indicates effusion. Most such “effusions” actually represent basilar atelectasis or epicardial fat or cardiomegaly on a hypoventilatory anteroposterior CXR. Our advice is to suggest pleural effusion if there are findings of effusion but to recognize that we cannot expect to diagnose everything with 100% accuracy on limited portable radiographs. In other words, try not to envision something simply because you are afraid of missing it.
As pleural effusions are usually gravity-dependent, the posterior costophrenic sulcus is the place to look for small effusions.
Generally, the biggest challenge in the diagnosis of pleural effusion is to recognize its presence on supine or semisupine radiographs. In that situation, fluid layers posterior to
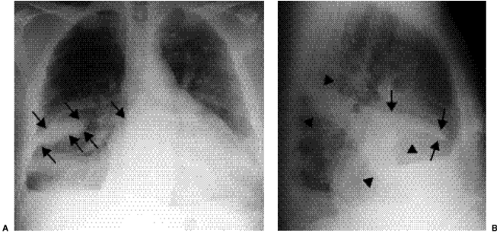
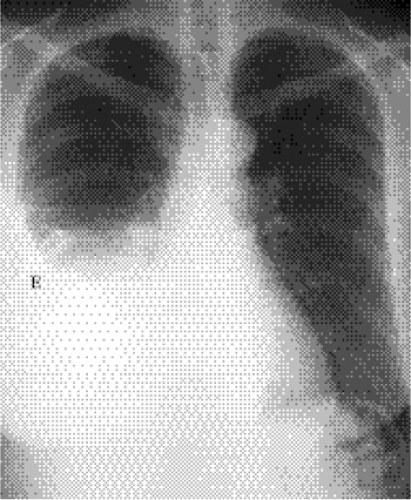
the lung. Because it is visualized en face, there is no sharp edge to outline the margin of effusion against normal pleura or lung. As a consequence, vague opacity is present, typically worst at the bases of the hemithoraces and becoming gradually less obvious as the eye travels cephalad. In the presence of large supine effusion, fluid will typically “cap” over the apex of the hemithorax (Fig. 17.2).
the lung. Because it is visualized en face, there is no sharp edge to outline the margin of effusion against normal pleura or lung. As a consequence, vague opacity is present, typically worst at the bases of the hemithoraces and becoming gradually less obvious as the eye travels cephalad. In the presence of large supine effusion, fluid will typically “cap” over the apex of the hemithorax (Fig. 17.2).
If it is important to know whether there really is pleural effusion in such a patient, solutions are available. As previously discussed in Chapter 3, the first step is to obtain lateral decubitus radiography; the side of suspected effusion should be the down side. Pleural
ultrasonography is an alternative, particularly when a small effusion is suspected, because ultrasonography can be used to guide thoracentesis as well. CT is not a reasonable alternative simply for detection of pleural effusion.
ultrasonography is an alternative, particularly when a small effusion is suspected, because ultrasonography can be used to guide thoracentesis as well. CT is not a reasonable alternative simply for detection of pleural effusion.
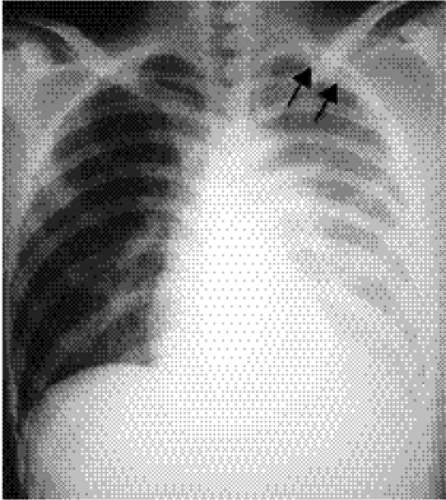 Figure 17.2 Supine left pleural effusion. Increased opacity throughout the left hemithorax with continued visualization of left lung vessels. Note fluid capping left apex (arrows). |
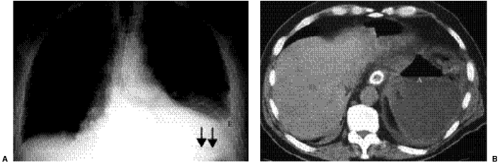
A potentially important effect of large pleural effusions is diaphragmatic inversion. In the presence of diaphragmatic inversion, the two hemidiaphragms move in opposite directions during respiration. As a consequence, air may move back and forth between the two lungs (pendelluft, or pendulum respiration) (1). The net effect is markedly increased dead space and significant dyspnea. Thoracentesis with removal of enough fluid to restore the affected hemidiaphragm to its normal position may result in marked relief of symptoms. Left hemidiaphragmatic inversion is more easily diagnosed because it results in mass effect in the left upper quadrant, displacing the gas-filled stomach (Fig. 17.3).
Large effusions may result in hemidiaphragmatic inversion, with significant dyspnea.
The other potentially important effect of diaphragmatic inversion is that it changes expected anatomic relationships that assist localization of peridiaphragmatic fluid at CT (2). In a patient with a normal convex-upward hemidiaphragm, fluid visualized outside the diaphragmatic outline is supradiaphragmatic (pleural) and fluid visualized inside the diaphragmatic outline is subdiaphragmatic (peritoneal) (2). In the presence of diaphragmatic inversion, these relationships are reversed.
In hospitalized patients, pleural effusions are most commonly seen with congestive heart failure or as a consequence of surgery. The stigmata of recent adjacent surgery (in the chest or in the upper abdomen) will usually be evident or might (rarely) be indicated in the provided clinical history for performance of the radiograph. If effusions are a result of congestive heart failure, they are typically bilateral and reasonably symmetric. Congestive heart failure effusions are occasionally unilateral and not infrequently somewhat asymmetric; in most such patients, right pleural effusion is larger.
When there is unilateral left pleural effusion (or left effusion is significantly larger than right effusion) in a nonsurgical patient, other etiologies should at least be considered (Box 17.1). For differential diagnostic purposes, in this situation you might run through categories of disease. First, because it is the category you do not want to forget, is neoplasm. Pleural metastases are far more common than pleural primary neoplasms. Many
primary neoplasms metastasize to the pleura. Those closest to the pleura (particularly lung and breast cancers) are especially likely, but in a given patient the most likely source of pleural metastases is that patient’s neoplasm. In other words, even a primary neoplasm that is not frequently associated with pleural metastases deserves serious consideration if a patient with that neoplasm develops pleural effusion. Lymphoma is also in the differential diagnosis, especially if there are multiple enlarged thoracic lymph nodes.
primary neoplasms metastasize to the pleura. Those closest to the pleura (particularly lung and breast cancers) are especially likely, but in a given patient the most likely source of pleural metastases is that patient’s neoplasm. In other words, even a primary neoplasm that is not frequently associated with pleural metastases deserves serious consideration if a patient with that neoplasm develops pleural effusion. Lymphoma is also in the differential diagnosis, especially if there are multiple enlarged thoracic lymph nodes.
Box 17.1: Causes of Pleural Effusion
Congestive heart failure
Surgery
Neoplasm—metastatic, primary
Inflammatory disease—infection, autoimmune
Abdominal disease—trauma, infection, inflammation, liver failure
Vascular—pulmonary embolus
Trauma—motor vehicle accident, stab or bullet wound, iatrogenic (catheter or feeding tube malposition)
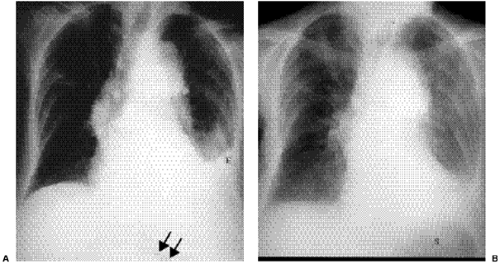
Among abdominopelvic neoplasms, ovarian carcinoma deserves special mention. It frequently spreads to the peritoneum, and pleural effusion in a patient with malignant ascites sometimes reflects leakage of fluid through the diaphragm. Pleural metastases from ovarian carcinoma do occur; they are commonly referred to as Meig syndrome. In fact, the original description of Meig syndrome referred to the association of pleural effusion with benign ovarian fibroma (Fig. 17.4). Over time, this term has become less precise and is now usually applied to any combination of pleural effusion and ovarian mass. Patients with pleural metastases from any primary may have unilateral or bilateral effusions.
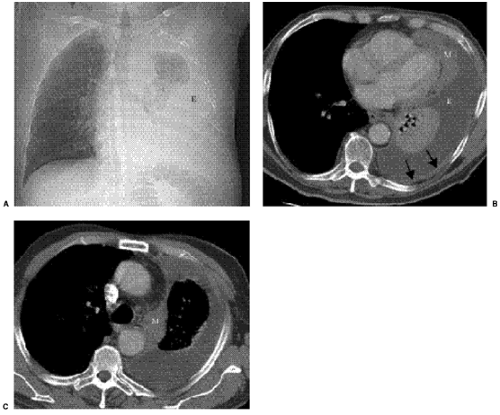
Malignant mesothelioma is the most common pleural primary neoplasm associated with pleural effusion, and most patients with malignant mesothelioma have pleural effusion (Fig. 17.5). Effusion is not usually an isolated finding in this setting. Instead, there is usually also
lobulated pleural mass. A history of asbestos exposure can be a helpful clue, but well-documented asbestos exposure is only established in about half of patients with malignant mesothelioma. In some patients lack of mediastinal shift away from the side of extensive pleural abnormality is a clue to the diagnosis of malignant mesothelioma (Fig. 17.6). Metastatic adenocarcinoma may closely mimic the appearance of malignant mesothelioma. Pleural effusions in patients with malignant mesothelioma are often unilateral.
lobulated pleural mass. A history of asbestos exposure can be a helpful clue, but well-documented asbestos exposure is only established in about half of patients with malignant mesothelioma. In some patients lack of mediastinal shift away from the side of extensive pleural abnormality is a clue to the diagnosis of malignant mesothelioma (Fig. 17.6). Metastatic adenocarcinoma may closely mimic the appearance of malignant mesothelioma. Pleural effusions in patients with malignant mesothelioma are often unilateral.
Most patients with malignant mesothelioma have pleural effusion.
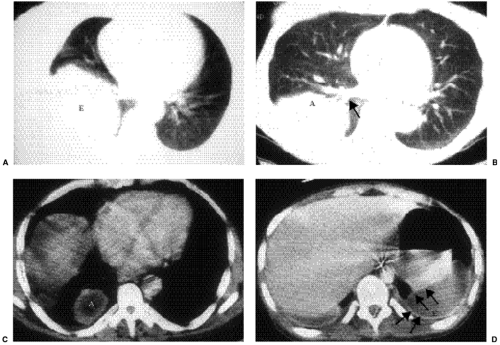
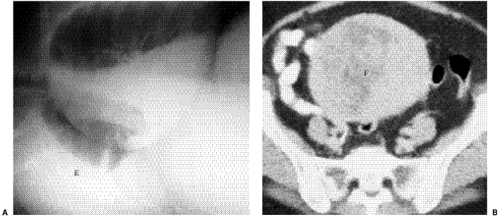 Figure 17.4 Meig syndrome. A. Right lateral decubitus radiograph: layering right pleural effusion (E). B. Pelvic computed tomography: large solid pelvic mass (F) represents an ovarian fibrothecoma. |
Inflammatory disease is the next category to consider. Under this heading, infection is an important consideration. Empyema can occur as a consequence of any pneumonia. Some organisms, such as M. tuberculosis and fungi, have a particular predilection for the pleural space (Fig. 17.7). The differentiation of empyema from lung abscess can generally be accomplished by CXR alone. Empyema typically has right or obtuse angles with the adjacent chest wall, whereas lung abscess usually demonstrates acute angles. Empyema is usually lenticular in shape and therefore is much larger on one of two right-angle projections, whereas lung abscess is more spherical in shape and more similar in size on right-angle projections. In selected instances, CT can aid in this distinction by demonstrating that empyema is more mass-like, deflecting vessels and bronchi in its path, whereas lung abscess is more destructive of lung structures but less mass-like. Smoother margins of
pleural abnormality and the CT “split pleura sign” of enhancing visceral and parietal pleura around an empyema can also aid in the differential diagnosis (3) (Fig. 17.8).
pleural abnormality and the CT “split pleura sign” of enhancing visceral and parietal pleura around an empyema can also aid in the differential diagnosis (3) (Fig. 17.8).
CT signs of empyema include mass-effect on adjacent lung structures, smooth margins, lenticular shape, obtuse or right angles with lung parenchyma, and the “split pleura sign.”
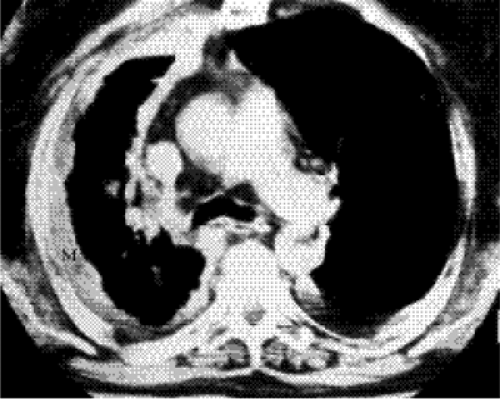 Figure 17.6 Malignant mesothelioma. Despite extensive right pleural abnormality (M), mediastinum is actually shifted to the right. |
However, CXR and CT alone cannot establish the presence or absence of infection in the lung or pleural space. Clinical findings (such as fever and elevated white blood cell count) are important in raising the possibility of infection. The role of imaging is to localize the infection to lung or pleura. The final etiology of pleural effusion is sometimes established on clinical grounds alone. In difficult cases, diagnosis generally relies on thoracentesis and analysis of pleural fluid; patients with lung infection commonly have uninfected pleural fluid (a so-called sympathetic effusion). The need for thoracentesis applies equally well to pleural neoplasm and to most other etiologies of pleural effusion.
Thoracentesis is often required to establish an etiology for pleural effusion, whether effusion is benign or malignant.
Inflammatory pleural effusion also includes a variety of autoimmune and related disorders. Among collagen vascular diseases, pleural effusion is particularly likely in systemic
lupus erythematosus (Fig. 17.9) and rheumatoid arthritis. In fact, pleural effusion is the most common thoracic manifestation of rheumatoid arthritis. As with all extraarticular manifestations of rheumatoid arthritis, pleural effusion is far more common in men than in women. Effusion is also seen in patients with an autoimmune response after myocardial infarction (Dressler syndrome) or cardiac surgery. Pleural effusions in this category may be unilateral or bilateral, symmetric or asymmetric.
lupus erythematosus (Fig. 17.9) and rheumatoid arthritis. In fact, pleural effusion is the most common thoracic manifestation of rheumatoid arthritis. As with all extraarticular manifestations of rheumatoid arthritis, pleural effusion is far more common in men than in women. Effusion is also seen in patients with an autoimmune response after myocardial infarction (Dressler syndrome) or cardiac surgery. Pleural effusions in this category may be unilateral or bilateral, symmetric or asymmetric.
Next for consideration are abdominal etiologies of pleural effusion. Adjacent upper abdominal abnormalities can cause effusion. Common etiologies in this category are splenic trauma, subdiaphragmatic abscess (Fig. 17.10), pancreatitis, and ascites. History is obviously very helpful, and thoracentesis can be very revealing (e.g., if there is elevated pleural fluid amylase in a patient with pancreatitis). Patients with ascites, such as those with liver failure, develop pleural effusions for several reasons, including leak of ascitic fluid through the diaphragm and anasarca as a result of decreased serum albumin. When right subdiaphragmatic abscess is an important concern, ultrasound can be very helpful. Because referring clinicians remain uninformed about ultrasound’s capabilities even at this relatively late date, they instead virtually always order CT, which is in fact better than ultrasound for left upper quadrant fluid collections. Most effusions resulting from abdominal disease are unilateral.
Another category to consider is vascular disease. In particular, pulmonary embolus is extremely difficult to diagnose via CXR. Most patients with pulmonary embolus have a normal CXR. When abnormality is present, it is often nonspecific; pleural effusion and atelectasis are the most common findings. Pleural effusion in pulmonary embolus can be unilateral or bilateral, because emboli are commonly multiple.
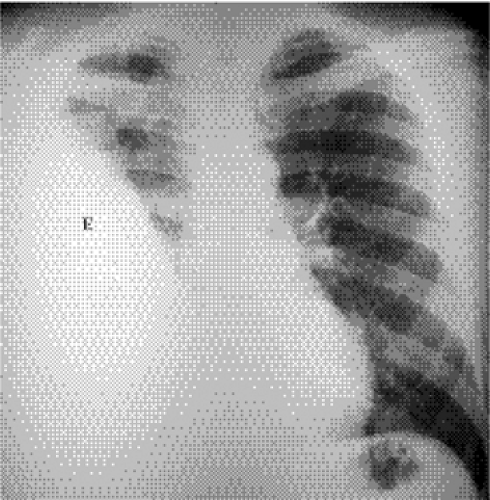
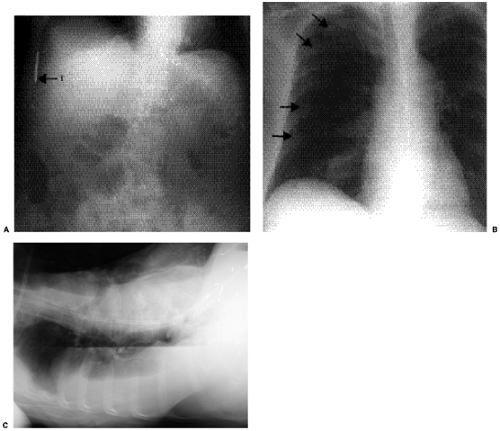
Trauma can result in pleural effusion. There may be obvious trauma, as in patients with multiple rib fractures. A somewhat less obvious example of trauma would be a patient with aortic laceration in the absence of fractures. An even less obvious example would be a malpositioned vascular catheter or feeding tube (4) (Fig. 17.11). Inadvertent placement of a feeding tube into the lung is usually benign as long as it is discovered before a feeding is administered. However, pleural placement is not similarly benign. Tension pneumothorax and empyema are among its important consequences. Traumatic pleural effusion is more commonly unilateral than bilateral.
Congenital and miscellaneous causes probably account for some pleural effusions (such as in lymphangiectasia and in lymphangiomyomatosis). They are sufficiently uncommon causes of pleural effusion that they are not discussed further here.
Pneumothorax
Pleural air tends to accumulate in the nondependent portion of the pleural space. Upright frontal radiography is generally the preferred technique for detecting pneumothorax. As discussed in Chapter 3, lateral decubitus radiography with the suspected side of pneumothorax up is a perfectly acceptable alternative; in experiments with cadavers (5) it was even sometimes better than upright views for detecting pleural air.
Because air accumulates in the non-dependent pleural space, upright or lateral decubitus radiographs are preferred for demonstration of pneumothorax.
The diagnosis of pneumothorax is best made by visualization of the lung edge outlined by pleural air (Fig. 17.12). Apical lucency and absence of vessels are far less reliable criteria that can be produced by bullae, for example. As with diagnosis of pleural effusion, detection of pneumothorax becomes trickier when the patient is supine. In that setting the
nondependent portion of the pleural space is near the hemidiaphragm. Lucency near the lung bases raises concern for pneumothorax, particularly in the presence of the deep sulcus sign (Fig. 17.13), even when no lung edge is visualized. Air in the minor fissure has been reported as another sign of supine pneumothorax (Fig. 17.14). Just as pleural effusion can track into fissures, pneumothorax can be visualized in the major fissure (Fig. 17.12) or even in accessory fissures (Fig. 17.15).
nondependent portion of the pleural space is near the hemidiaphragm. Lucency near the lung bases raises concern for pneumothorax, particularly in the presence of the deep sulcus sign (Fig. 17.13), even when no lung edge is visualized. Air in the minor fissure has been reported as another sign of supine pneumothorax (Fig. 17.14). Just as pleural effusion can track into fissures, pneumothorax can be visualized in the major fissure (Fig. 17.12) or even in accessory fissures (Fig. 17.15).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree