Thoracic Interventional Techniques
Percutaneous Transthoracic Needle Biopsy
Image-guided percutaneous transthoracic needle biopsy (PTNB) of the lung is an important procedure in the diagnosis of thoracic and extrathoracic malignancies. It is also used, though less commonly, in the diagnosis of infectious and inflammatory disease. Suspected malignancies can be quickly and safely diagnosed, and sometimes staged, and appropriate therapies or surgical intervention can be planned. PTNB can also be used to evaluate potentially benign conditions. Although a benign entity such as hamartoma or infection is difficult to confirm, when it is obtained it may obviate the need for surgery. Fluoroscopically directed and ultrasound-directed procedures are fast and relatively inexpensive to perform and allow real-time imaging. Computed tomography (CT) and CT fluoroscopy have made it easier and more feasible to sample smaller and more awkwardly placed lesions with greater accuracy and efficiency.
Methods
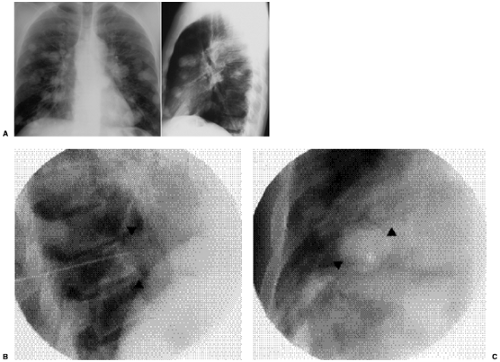
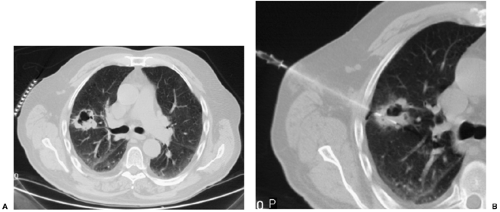
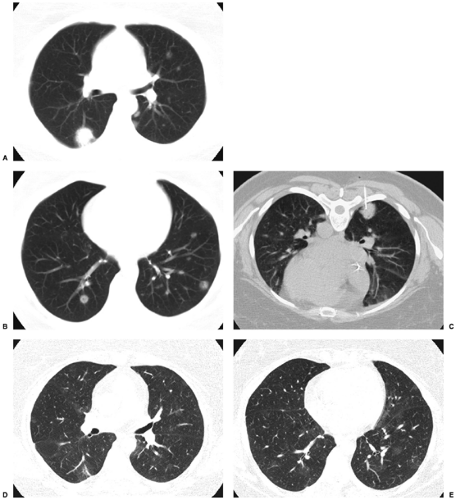
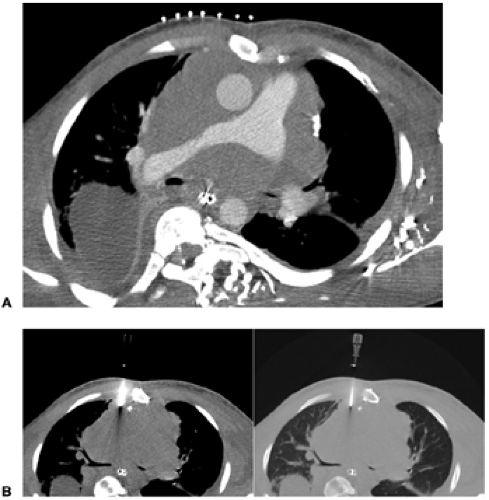
Performing needle biopsies with biplane fluoroscopic guidance can be faster and less expensive than performing the same procedure with CT guidance. When the lesion can be visualized in two planes, a fluoroscopic procedure may be preferred because the lung and lesion can be directly visualized in real-time (Fig. 22.1). Fluoroscopy, however, should not be used when the lesion cannot be reliably demonstrated on both the frontal and lateral chest radiographs or for lesions that are in difficult locations, such as adjacent to the hilum, mediastinum, or juxtavascular. For these lesions, CT is favored (Fig. 22.2). The main disadvantages of CT are its greater cost and longer procedure times. Detection of complications, such as pneumothorax, is frequently delayed because the patient is not imaged in real-time.
In recent years, CT fluoroscopy has become available. CT fluoroscopy provides a real-time cross-sectional image, updated about six times per second. X-ray tube cooling issues often limit the imaging time to 5 seconds per application, so it is most useful for brief looks rather than continuous real-time guidance.
Ultrasound is a very useful imaging modality for guiding interventional procedures. Several advantages include its real-time imaging, lack of ionizing radiation, low cost, and portability. For patients in the intensive care unit, intubated patients, or patients otherwise unable to be safely brought to the radiology department, ultrasound may be the only alternative. Ultrasound can be used to localize fluid collections for thoracentesis for guidance during drainage tube placement or for needle biopsies of lesions adjacent to the pleura or chest wall (1) (Fig. 22.3).
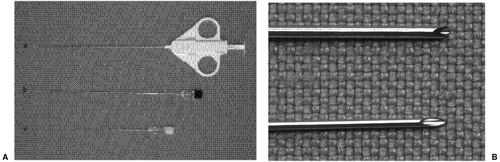
Methods for performing PTNB are use of a fine-caliber needle for aspiration sampling or use of a spring-loaded cutting needle to obtain larger and more intact core samples (Fig. 22.4). Fine-needle aspiration (FNA) is typically less traumatic on the surrounding tissue and has the benefit of allowing the cytopathologist to make a rapid diagnosis. It is best to have the cytopathologist present at the procedure to determine if the specimens are adequate for diagnosis rather than requiring a repeat biopsy. This is particularly helpful when the patient is in need of immediate treatment. Cutting needle systems are helpful when a larger amount of tissue is needed for histologic diagnosis or special staining. Core samples are also more accurate in the diagnosis of benign conditions and for certain
malignancies, such as lymphoma, where the relatively small amount of tissue obtained by FNA may be equivocal or nondiagnostic.
malignancies, such as lymphoma, where the relatively small amount of tissue obtained by FNA may be equivocal or nondiagnostic.
Aspirating needles obtain cells for cytology.
Core needles obtain tissue cores for histology.
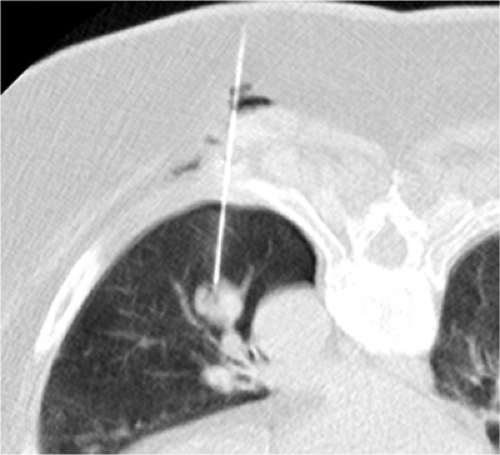 Figure 22.2 Computed tomography-guided needle biopsy of a left lower lobe nodule. Note proximity of nodule to the descending thoracic aorta and left lower lobe pulmonary veins. |
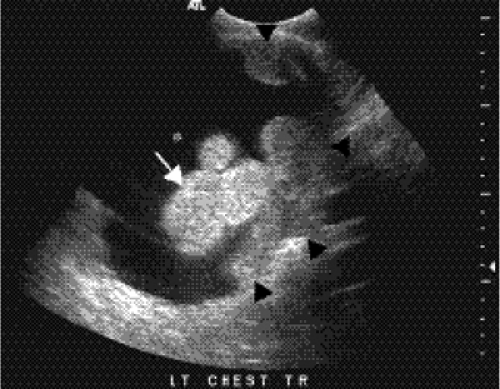 Figure 22.3 Prebiopsy ultrasound image demonstrating a lobulated pulmonary nodule (arrow), pleural thickening (arrowheads), and pleural effusion (asterisk). |
Either method can be performed via direct puncture or coaxial technique. In the latter, a larger caliber guiding needle, typically 19 gauge for lung and 17 gauge for chest wall, is first placed to the margin of the lesion and the biopsy device is passed through the center into the lesion. This allows multiple samples with only one pleural puncture; the risk of pneumothorax increases each time the pleural surface is transgressed. Coaxial systems are often advantageous when the need for multiple biopsy samples is anticipated or when the target lesion is small or difficult to reach.
Tissue sampling with FNA, regardless of the needle type used, can be performed in essentially the same way. By placing a syringe on the needle hub, gentile suction can be applied while agitating the needle tip within the lesion. It is best to release the suction as soon as there is a flash of blood at the needle hub to prevent obscuring cytopathologic visualization of abnormal cells with excessive blood. FNA and core needle systems should be positioned along the periphery of the lesion to reduce the amount of potentially necrotic tissue in the sample (Fig. 22.5). With either FNA or cutting needles, the patient should suspend respiration during the sampling process, particularly when the device is open to the atmosphere.
Indications
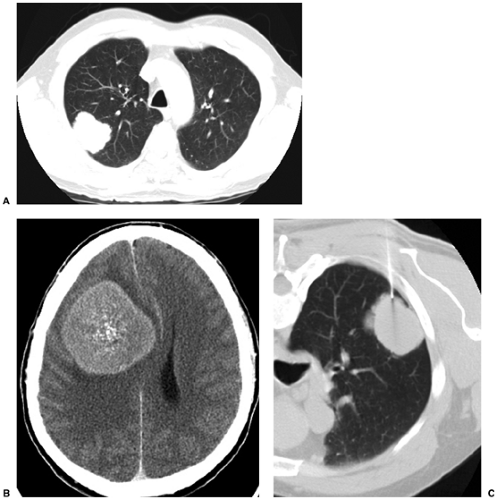
There are many indications for PTNB (Table 22.1), the most common of which is the presence of an indeterminate pulmonary nodule (2,3). Even in patients with a known history of extrathoracic malignancy, the presence of pulmonary metastasis can have significant impact on treatment. Presence of a new mediastinal or hilar mass are also valid indications for PTNB. PTNB can also be used for staging of known malignancies. It is also very useful in obtaining samples for culture and sensitivity testing in suspected infections, particularly in immunocompromised patients.
Table 22.1: Indications for Percutaneous Transthoracic Needle Aspiration Biopsy | |
|---|---|
|
Imaging and Site Preparation
Before performing any procedure, the patient’s laboratory studies should be reviewed. Important tests include prothrombin time, partial thromboplastin time, and platelet count (4). When necessary, conscious sedation can be administered to the patient; however, it is important to keep any sedative light enough for the patient to follow commands appropriately, particularly breath-hold instructions. Patients with persistent coughing may have some temporary relief from a cough suppressant containing codeine, to help minimize motion while the needle is in place. Patients should be monitored with continuous pulse oxymetry and periodic blood pressure and heart rate measurements. Two liters of oxygen via nasal cannula is very helpful in making patients more comfortable and may be necessary for the patient with chronic obstructive pulmonary disease who has breathing difficulties while supine. Supplemental oxygen should be given to any patient receiving sedation.
Bleeding status should be evaluated before performing percutaneous lung biopsy.
The basic technique for either direct puncture or coaxial technique is similar. Based on scout imaging, the patient is placed on the CT table in an appropriate but secure position. The patient can be positioned in almost any orientation—supine, prone, lateral decubitus, or oblique. The two most important factors in choosing a position for the patient are (a) ease of lesion access across the shortest distance with avoidance of the fissures and (b) patient comfort, so they are more likely to remain motionless. For this reason, supine and prone positions are preferred. Easy needle trajectory is not helpful if the patient cannot maintain the position for the duration of the procedure. Once a position has been chosen, radiopaque markers are placed on the skin at the expected entry site and a scout image is obtained to select the level for needle placement. Small peripheral lesions can often present a problem due to their proximity to the ribs, which may prevent a direct trajectory. Angling the CT gantry a few degrees to be in-plane with the ribs is often helpful in displaying the intercostal spaces better and can help with biopsy planning. When imaging the lesion for biopsy planning, it is often helpful to have the patient breathe quietly instead of suspending respirations. This will give a good idea of how much the lesion can be expected to move during the procedure.
Coaxial technique is preferred for lung biopsies, using one pleural puncture.
For procedures where the intercostal space must be traversed, the needle should be positioned so it remains as close to the superior surface of the adjacent rib as possible, because the neurovascular bundle runs directly below the inferior margin of each rib. Crossing the neurovascular bundle with a needle or catheter can result in significant pain and bleeding. The shortest path from skin to lesion should also be chosen. It is best to avoid crossing fissures, vessels, bronchi, and abnormal lung parenchyma, such as emphysema and bullae. Ideally, crossing as little aerated lung as possible is preferred (5) (Figs. 22.6 and 22.7).
After a proper entry site is selected, the site is cleaned and prepped with sterile technique, taking care to disinfect the entry site and surrounding region. A sterile operative field should be maintained at all times, and surgical-site drapes and covers should be used. Shaving any hair from the entry site is also recommended to maintain a clean skin surface. Local anesthesia can be achieved by using 1% to 2% lidocaine solution injected subcutaneously and then deeper into the soft tissues as needed.
Using periodic imaging either via axial CT images or real-time CT fluoroscopy, the biopsy device or introducing needle is carefully inserted through the chest wall to the margin of the target lesion. Ideally, the pleura should be crossed only once, because potential
risk of pneumothorax increases with each pleura transgression. Ideally, the needle should be first positioned in the chest wall to establish the correct trajectory before any pleural punctures. When the chest wall is thin, the lidocaine needle can be used to assist with establishing the trajectory. The patient should be instructed to suspend respiration while crossing the pleura with the needle and to breathe quietly after the needle is across. This will help to prevent a large pleural puncture site and reduce the risk of pneumothorax. While the needle is within the lung or pleural space, the hub should remain closed to the atmosphere while the patient is breathing to limit the amount of air entering the thorax.
risk of pneumothorax increases with each pleura transgression. Ideally, the needle should be first positioned in the chest wall to establish the correct trajectory before any pleural punctures. When the chest wall is thin, the lidocaine needle can be used to assist with establishing the trajectory. The patient should be instructed to suspend respiration while crossing the pleura with the needle and to breathe quietly after the needle is across. This will help to prevent a large pleural puncture site and reduce the risk of pneumothorax. While the needle is within the lung or pleural space, the hub should remain closed to the atmosphere while the patient is breathing to limit the amount of air entering the thorax.
Technical Factors
Typically, three good core or FNA specimens are sufficient to make a diagnosis of malignancy, though more may be necessary if cultures or special pathologic stains are requested. In one study of 38 malignant lesions aspirated with a 25/22 gauge coaxial FNA system, 85% of the lesions were positive for malignancy with one, two, or three passes (6). Only 15% of lesions required up to six needle passes; 69% were positive with a single aspirate alone. When performing FNA, it is helpful to have cytopathology standing by to examine the specimens as they are obtained. This reduces the possibility of a nondiagnostic biopsy
and gives an opportunity to obtain additional material if necessary. In a series of 896 malignant lesions, an 87% positive diagnostic rate after one procedure was shown, which rose to 96% after a second PTNB procedure in 75 patients (7). For patients in whom PTNB is indicated, particularly nonsurgical candidates, a second biopsy procedure should be considered if malignancy is suspected, rather than a more invasive open thoracotomy or thoracoscopic procedure.
and gives an opportunity to obtain additional material if necessary. In a series of 896 malignant lesions, an 87% positive diagnostic rate after one procedure was shown, which rose to 96% after a second PTNB procedure in 75 patients (7). For patients in whom PTNB is indicated, particularly nonsurgical candidates, a second biopsy procedure should be considered if malignancy is suspected, rather than a more invasive open thoracotomy or thoracoscopic procedure.
In general, three tissue samples are sufficient for diagnosis.
PTNB of the chest wall, pleura, and mediastinum are performed in essentially the same manner as biopsies of the lung. Selecting a trajectory that avoids aerated lung reduces or eliminates the risk of pneumothorax (5). Percutaneous biopsy of pleural lesions has been shown to be quite effective (8), and in sampling a pleural lesion or a segment of pleural thickening, choosing a trajectory that passes tangentially to the pleura and lung is preferred. Additionally, careful contrast-enhanced CT may be necessary before the procedure to map locations of vital structures and vessels, which may not otherwise be adequately seen on noncontrast imaging (Fig. 22.8).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree