Chapter 15 Supraventricular Arrhythmias, Part II Atrial Flutter and Atrial Fibrillation
Please go to expertconsult.com for supplemental chapter material.
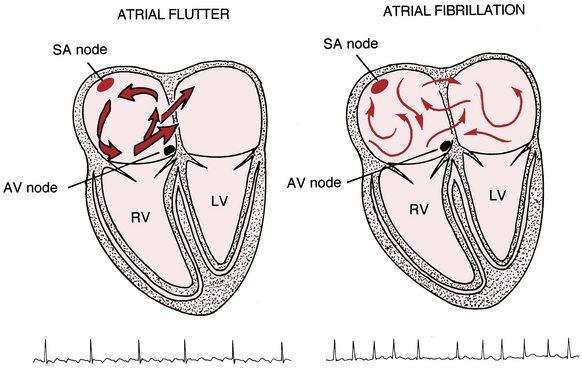
The supraventricular (common narrow complex) tachycardias discussed so far have organized atrial activity (manifest by discrete P waves) and, with some notable exceptions, 1:1 atrioventricular (AV) conduction.∗ Atrial fibrillation (AF) and atrial flutter (AFL) are two related (and sometimes missed or mistaken) arrhythmias with very rapid atrial rates that greatly exceed the ventricular rate (Fig. 15-1). This finding implies that some degree of physiologic (functional) AV block† is almost always present. Furthermore, both arrhythmias involve reentrant mechanisms with impulses rapidly and continuously spinning around, “chasing their tails,” in the atrial muscle itself (see Fig. 15-1). Therefore, instead of true P waves, one sees continuous F (flutter) or f (fibrillatory) waves.
Atrial Flutter
Location of Conduction Pathways
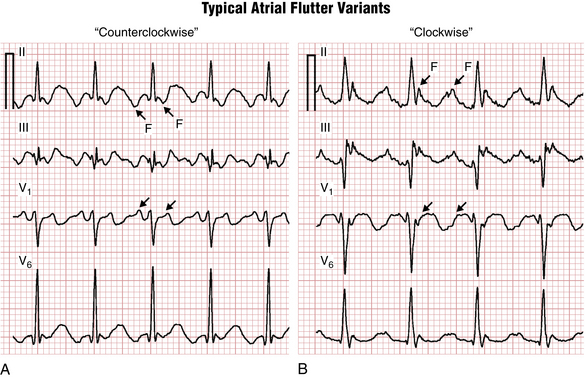
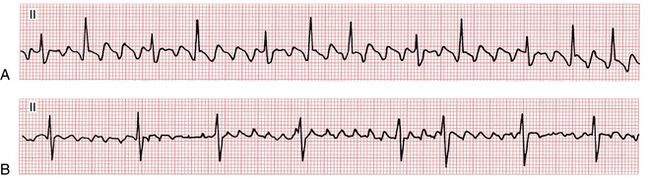
The classic “sawtooth” pattern of F waves that are predominantly negative in leads II, III, and aVF and positive in V1 with a very regular ventricular (QRS) rate of about 150/min (functional 2:1 AV block) is suggestive of the counterclockwise (common) type of typical right atrial flutter (Fig. 15-2A). Less frequently the same circuit gets initiated in the opposite direction, producing “clockwise” flutter. The polarity of the F waves will then be reversed: positive in leads II, III, and aVF, and negative in lead V1 (Fig. 15-2B). Clockwise and counterclockwise flutter can occur in the same patient and both are usually isthmus-dependent.‡ Clinically, the development of atrial flutter most often indicates the presence of underlying structural/electrical atrial disease.
Conduction to the Ventricles
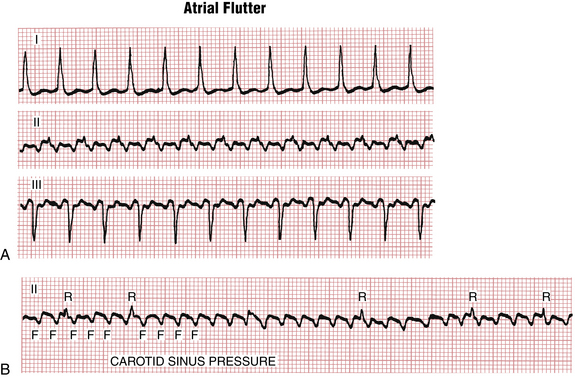
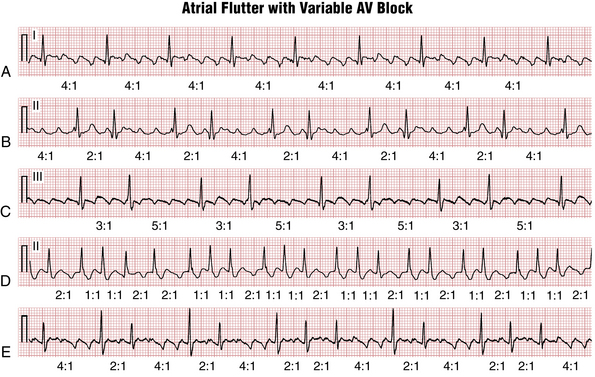
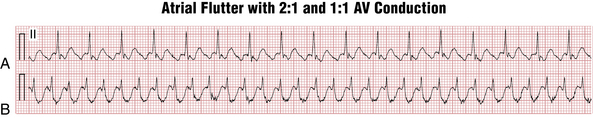
The atrial rate during typical atrial flutter, as noted, is around 300 cycles/min (range usually between about 240 to 330 cycles/min). Slower rates can be due to drugs that slow atrial conduction. Fortunately, the AV node cannot conduct electrical signals at that rate to the ventricles—although a bypass tract in the Wolff-Parkinson-White (WPW) syndrome (see Chapter 12) can! Thus, with atrial flutter, physiologic AV block develops (usually with a 2:1 A/V ratio) (Figs. 15-2 and 15-3). In the presence of high vagal tone, AV nodal disease, or AV nodal blocking drugs (e.g., beta blockers, digoxin, and certain calcium channel antagonists) higher degrees of AV block can be seen, for example with a 4:1 conduction ratio (Figs. 15-3 and 15-4).
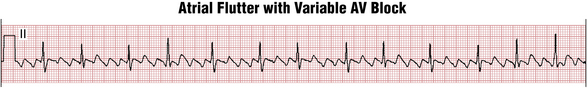
Often the AV nodal conduction shows more complex patterns and the degree of AV block varies in a periodic way, producing flutter/QRS ratios with repeating patterns (Fig. 15-4) of RR intervals (group beating). This phenomenon is believed to be due to multiple levels of block within the conduction system. Variable AV block may be due to other mechanisms (e.g., AV Wenckebach) and produce noninteger ratios of F waves to QRS complexes (Fig. 15-5).
On the other hand, atrial flutter with 1:1 AV conduction (Fig. 15-6), although uncommon, can occur in three major settings:
• In high catecholamine states (strenuous physical activity, infection, with high fever, shock, etc.)
• With certain antiarrhythmic medications (such as flecainide) that slow down the flutter rate (for example, from 300 to 250/min or less) to the point where 1:1 conduction through AV node becomes possible
• In the presence of a bypass tract (WPW pattern) capable of rapid conduction (short refractory period)
Atrial flutter with sustained 1:1 AV conduction represents an emergency situation, requiring consideration of immediate synchronized electrical cardioversion because of the dangerously rapid ventricular rate.
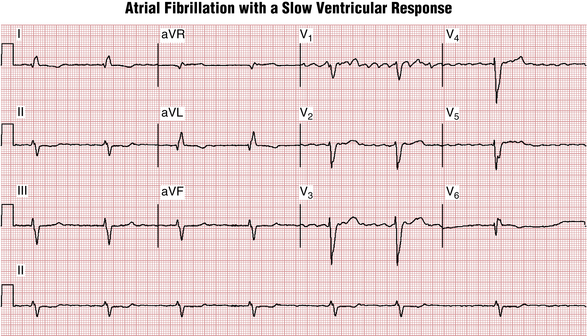
Atrial Fibrillation
Unlike atrial flutter, the reentrant waves of atrial fibrillation (AF) cannot be localized to any repetitive and stable circuit in the atria. Most cases of AF are thought to originate in the area of pulmonary vein–left atrial junctions. With time, more and more of the atrial tissue becomes involved in the active maintenance of the arrhythmia, associated with the simultaneous formation of multiple unstable reentrant circuits throughout the atria (see Fig 15-1).
Milder degrees of atrial activity “disorganization” or drugs that slow atrial activation may produce coarse AF with high amplitude f waves resembling atrial flutter (Fig. 15-7).