Chapter 14 Supraventricular Arrhythmias, Part I Premature Beats and Paroxysmal Supraventricular Tachycardias
Please go to expertconsult.com for supplemental chapter material.
General Principles: Triggers and Mechanisms of Tachyarrhythmias
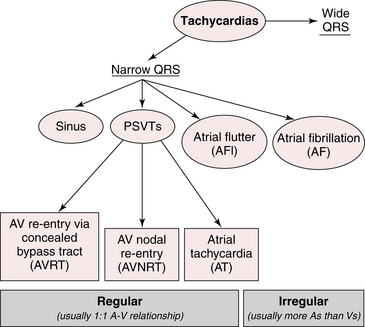
This chapter and the next focus on disturbances of cardiac rhythm with a rapid rate, namely: supraventricular and ventricular tachyarrhythmias (Fig. 14-1).
Key Pathophysiologic Concept
For any rapid, abnormal heart rhythm to occur, two major factors have to be present:
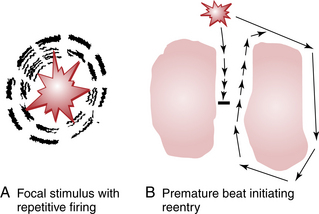
Tachyarrhythmias, both supraventricular and ventricular, in turn, usually start with premature beats that initiate arrhythmias by either focal or reentrant mechanisms (Fig. 14-2).
The sinus or sinoatrial (SA) node (see Chapter 13) is the physiologic (natural or intrinsic) pacemaker of the heart. The SA node normally initiates each heartbeat, producing (normal) sinus rhythm. However, pacemaker stimuli can arise from other parts of the heart, including the atrial muscle or pulmonary vein area, the atrioventricular (AV) junction, or the ventricles.
Ectopic beats are often premature; that is, they come before the next sinus beat is due. Examples include atrial premature beats (APBs), AV junctional premature beats (JPBs), and ventricular premature beats (VPBs). Ectopic beats can also come after a pause (delay) in the normal rhythm, as in the case of AV junctional or ventricular escape beats (see Chapter 13). Ectopic beats originating in the AV junction (node) or atria are referred to as supraventricular (i.e., literally coming from above the ventricles).
This chapter and Chapter 15 describe the major supraventricular arrhythmias, and Chapter 16 deals with ventricular tachycardias.
Atrial and Other Supraventricular Premature Beats
APBs∗ result from ectopic stimuli and are beats arising from loci in either the left or right atrium, or interatrial septum, but not the SA node itself. The atria, therefore, are depolarized from an ectopic site. After an atrial or junctional depolarization, the stimulus may spread normally through the His-Purkinje system into the ventricles. For this reason, ventricular depolarization (QRS complex) is generally not affected by APBs or JPBs. The major features of APBs are listed in Box 14-1 and are depicted in Figures 14-3 to 14-6.
BOX 14-1 Major Features of Atrial Premature Beats
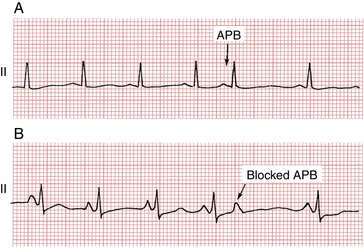
• The atrial depolarization (P′ wave) is premature, occurring before the next sinus P wave is due.
• The QRS complex of the atrial premature beat (APB) is usually preceded by a visible P wave that usually has a slightly different shape or different PR interval from the P wave seen with sinus beats. The PR interval of the APB may be either longer or shorter than the PR interval of the normal beats. In some cases the P wave may be subtly hidden in the T wave of the preceding beat.
• After the APB a slight pause generally occurs before the normal sinus beat resumes. This delay is due to “resetting” of the sinoatrial (SA) node pacemaker by the premature atrial stimulus. This slight delay contrasts with the longer, “fully compensatory” pause often (but not always) seen after ventricular premature beats (VPBs) (see Fig. 16-9).
• The QRS complex of the APB is usually identical or very similar to the QRS complex of the preceding beats. Remember that with APBs the atrial pacemaker is in an ectopic location but the ventricles are usually depolarized in a normal way. This sequence contrasts with the generation of VPBs, in which the QRS complex is abnormally wide because of abnormal depolarization originating in the ventricles (see Chapter 16).
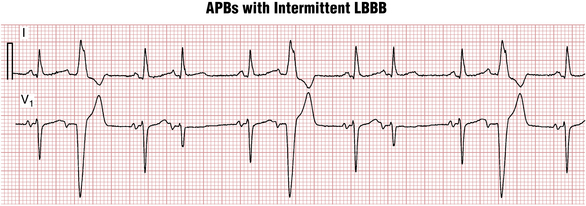
• Occasionally, APBs result in aberrant ventricular conduction, so that the QRS complex is wider than normal. Figures 14-5 and 14-6 show examples of such APBs causing delayed (aberrant) depolarization of the right and left ventricles, respectively.
• Sometimes when an APB is very premature, the stimulus reaches the atrioventricular (AV) junction just after it has been stimulated by the preceding beat. Because the AV junction, like other cardiac tissues, requires time to recover its capacity to conduct impulses, this premature atrial stimulus may reach the junction when it is still refractory. In this situation the APB may not be conducted to the ventricles and no QRS complex appears. The result is a blocked APB. The ECG shows a premature P wave not followed by a QRS complex (see Fig. 14-3B). After the blocked P wave, a brief pause occurs before the next normal beat resumes. The blocked APB, therefore, produces a slight irregularity of the heartbeat. If you do not search carefully for these blocked APBs, you may overlook them.
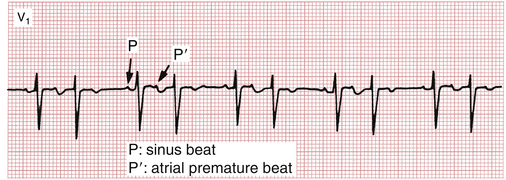
Figure 14-4 Sinus rhythm with atrial bigeminy. Each sinus beat is coupled to an atrial premature (early) beat followed by a slight postectopic pause. This sequence is one of the causes of group beating pattern and must be distinguished from second-degree atrioventricular (AV) heart block in which the sinus P waves come “on time” and one is not conducted (see Chapter 17).
APBs may occur frequently or sporadically. Two APBs occurring consecutively are referred to as an atrial couplet. Sometimes, as shown in Figure 14-4, each sinus beat is followed by an APB. This pattern is referred to as atrial bigeminy.
Clinical Significance
APBs, conducted and blocked, are very common. They may occur in people with normal hearts or with virtually any type of organic heart disease. Thus, the presence of APBs does not imply that an individual has cardiac disease. In normal people these premature beats may be seen with emotional stress, excessive intake of caffeinated drinks, or the administration of sympathomimetic agents (epinephrine, isoproterenol). APBs may also occur with hyperthyroidism. APBs may produce palpitations; in this situation, patients may complain of feeling a “skipped beat” or an irregular pulse. APBs may also be seen with various types of structural heart disease. Frequent APBs are sometimes the forerunner of atrial fibrillation or flutter (see Chapter 15) or other supraventricular tachyarrhythmias discussed later.
Paroxysmal Supraventricular Tachycardias
Premature supraventricular beats (Box 14-2) may occur singly or repetitively. A sudden run of three or more such consecutive nonsinus beats constitutes an episode of paroxysmal supraventricular tachycardia (PSVT). Episodes of PSVT may be brief and nonsustained (i.e., lasting from a few beats up to 30 sec). Sustained episodes (greater than 30 sec) may last minutes, hours, or longer.


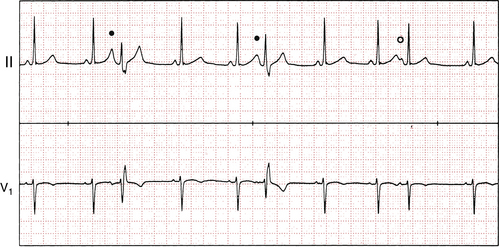
 ) is conducted with normal ventricular activation. Notice how the first two premature P waves come so early in the cardiac cycle that they fall on the T waves of the preceding sinus beats, making these T waves slightly taller.
) is conducted with normal ventricular activation. Notice how the first two premature P waves come so early in the cardiac cycle that they fall on the T waves of the preceding sinus beats, making these T waves slightly taller.