Selecting the Ventilator and the Mode
Learning Objectives
On completion of this chapter, the reader will be able to do the following:
2 Describe how CPAP and NIV are used to deliver noninvasive positive-pressure ventilation.
3 Compare the advantages and disadvantages of volume-controlled and pressure-controlled ventilation.
7 Provide examples of the types of patients who would benefit most from each mode of ventilation.
Key Terms
• Assist/control ventilation
• Assisted breaths
• Continuous mandatory ventilation
• Control ventilation
• Full ventilatory support
• Mandatory breaths
• Partial ventilatory support
• Patient-ventilator asynchrony
• Spontaneous breaths
Once the need for mechanical ventilation has been established, the clinician must select the type of ventilator, the ventilator mode, and the breath type for the patient. This chapter focuses on factors that affect the choice of ventilator, patient interface (i.e., artificial airway or mask), control variable (volume or pressure), breath type, and ventilator mode.
Selecting the appropriate ventilator and mode of ventilation can be challenging even for an experienced clinician. The following questions provide a framework for making the selection process manageable:
• Why does the patient need ventilatory support? (Indication)
• Does the ventilatory problem require a special mechanical ventilation mode? (Pathology)
• What therapeutic goals can be achieved by using a specific ventilator? (Treatment goals)
• Does the patient need to be intubated, or can a mask be used? (Patient interface)
• Will ventilatory support be required for a brief period or long term? (Duration)
• How familiar is the staff with the ventilator (or ventilators) under consideration? (Staff training)
If a change is to be made from one type of ventilator to another, the respiratory therapist must know whether the change is being made because a different mode or feature is needed. For example, a patient may have acute respiratory distress syndrome (ARDS) and may need a ventilator that can provide an advanced modality.
If a patient is to be discharged from the hospital to their home or to an extended care facility, a ventilator that would be appropriate in that setting should be selected. For example, a patient with amyotrophic lateral sclerosis may be familiar and comfortable with noninvasive ventilation. A patient with post-polio syndrome may be more familiar with a chest cuirass or tank ventilator (negative-pressure ventilator [NPV]). (Although NPV is not discussed here, it is important to mention that it is sometimes used in the home-care or alternative-care setting. In rare cases NPV has been used for ventilation of acutely ill infants.1,2 [See Chapter 21 for additional information on NPV.])
This chapter focuses on positive-pressure ventilation (PPV). Positive pressure ventilators can function in a wide variety of settings and provide a variety of modes, features, monitors, and alarms.
Noninvasive and Invasive Positive-Pressure Ventilation: Selecting the Patient Interface
A patient can be connected to a positive-pressure ventilator using either a positive-pressure mask or an artificial airway. Face and nasal masks are used to administer noninvasive ventilatory support. Artificial airways, which include translaryngeal airways (oral or nasal endotracheal tubes [ETs]) and tracheostomy tubes, are required for invasive ventilation. About 75% of patients receiving invasive PPV are intubated (95% with an oral ET and 5% with a nasal ET). Tracheostomy tubes are used in the remaining 25% of patients receiving invasive PPV.3
Noninvasive Positive-Pressure Ventilation
There are two methods of providing noninvasive positive-pressure ventilator support:
As previously mentioned, CPAP and NIV are most commonly administered via a face or nasal mask. Ensuring that the mask fits properly will minimize patient discomfort and help prevent air leaks. Mask interfaces are discussed in more detail in Chapter 19.
Continuous Positive Airway Pressure
In hospitalized patients, CPAP has been shown to be an effective method to improve oxygenation. It also is an accepted method used to treat obstructive sleep apnea, especially in the home. In addition, CPAP can be used to assist patients with chronic obstructive pulmonary disease (COPD) who have difficulty breathing. The use of CPAP in COPD patients has received some attention because air trapping can occur in a spontaneously breathing individual with increased airway resistance (Raw). Air trapping in patients with COPD or in patients with acute asthma can lead to an increase in the functional residual capacity (FRC). In the past, CPAP was considered contraindicated in patients with COPD because these patients already had an increased FRC. The concern among some clinicians was based on the assumption that external CPAP or positive end-expiratory pressure (PEEP) would further increase the FRC and would not benefit the patient.
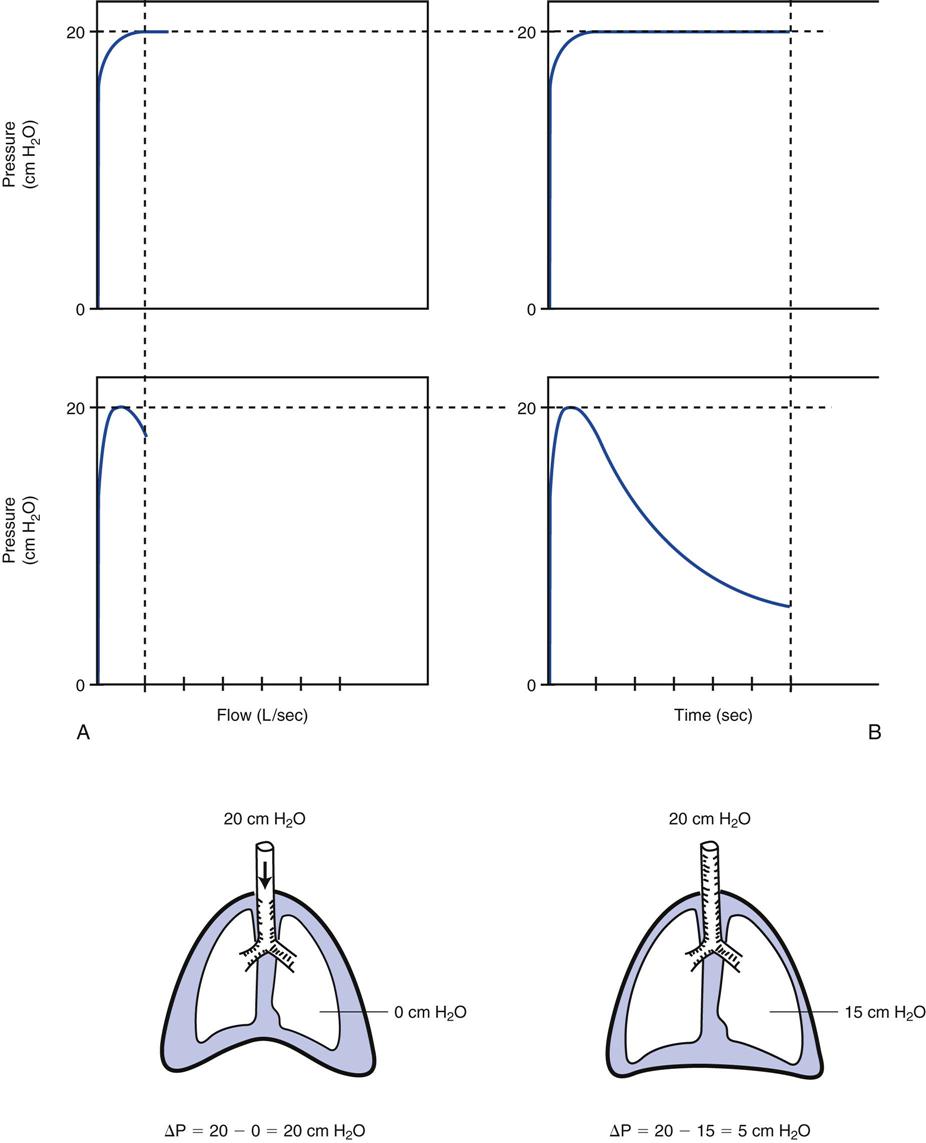
Patients with COPD often have difficulty generating the pressure difference between the alveoli and the mouth to begin inspiratory gas flow. The air trapped in the lungs (called intrinsic PEEP or auto-PEEP) creates a positive alveolar pressure (Palv). If the pressure in the lungs is positive at end exhalation, the pressure must drop below the pressure at the mouth (atmospheric pressure) to start gas flowing into the lung for inspiration. For example, if auto-PEEP is > +5 cm H2O, the patient must exert an effort of at least −5 cm H2O to drop the lung pressure below zero. Once alveolar pressure drops below zero, inspiratory gas flow can start.
Externally applied CPAP may reduce the pressure difference between the mouth and the alveoli when flow limitation (increased Raw) is the cause of auto-PEEP. The patient therefore does not have to work as hard to drop the Palv so that inspiratory gas flow enters the lung. In other words, externally applied CPAP can reduce inspiratory work.4 Mask CPAP set at 80% to 90% of the measured auto-PEEP (usually about 4-10 cm H2O) reduces diaphragmatic work and dyspnea, improves gas exchange, and does not worsen hyperinflation.5–7 In many cases, clinicians prefer using noninvasive positive pressure ventilator support in the form of bilevel positive airway pressure (bilevel PAP) rather than CPAP for patients with Raw-induced auto-PEEP (Box 5-1). Bilevel PAP also is the method most often used to treat acute-on-chronic respiratory failure (see Chapter 4). [An example of an acute-on-chronic respiratory condition is a patient with chronic bronchitis who develops pneumonia (an acute condition).]
Noninvasive Positive-Pressure Ventilation
Numerous of investigators have examined the use of NIV for patients with respiratory failure caused by various neuromuscular disorders, chest wall deformities, COPD, central ventilatory control abnormalities, and acute cardiogenic pulmonary edema (Box 5-2).8–12 Their findings suggest that NIV can reduce the need for intubation in 60% to 75% of these patients.9,10,13,14 Two types of ventilators can be used to provide NIV:
• Pressure-triggered, pressure-limited, flow-cycled devices designed specifically for mask ventilation, (e.g., BiPAP [Philips, Respironics, Murrysville, Pa.])9
• Critical-care ventilators that have a variety of available modes, including in many cases NIV.
Box 5-3 lists some of the advantages and disadvantages of NIV compared with invasive ventilation.4,11,15 Box 4-7 lists accepted indications and contraindications for NIV. If patients are not excluded by the presence of contraindications, NIV offers the clinician an excellent option for a number of acute and chronic conditions requiring mechanical ventilation.
Invasive Positive-Pressure Ventilation
As mentioned previously, a high percentage of patients who need mechanical ventilation require invasive positive-pressure ventilation via an artificial airway. Once the appropriate ventilator has been chosen, the clinician must select a mode of ventilation that is most advantageous for the patient’s condition.
Full and Partial Ventilatory Support
The terms full ventilatory support (FVS) and partial ventilatory support (PVS) describe the extent of mechanical ventilation provided. With FVS the ventilator provides all the energy necessary to maintain effective alveolar ventilation.15 FVS results in arterial partial pressure of carbon dioxide (Paco2) values less than 45 mm Hg or a Paco2 that is normal for the patient (i.e., eucapnic breathing). FVS is provided when ventilator rates are high (8 breaths/min or more) and tidal volume (VT) is adequate for the patient. (See Chapter 6 for information on VT settings and ideal body weight.)16 FVS is typically provided using a ventilator mode that provides a preset volume or pressure when a breath is delivered. The mode must be set so that the patient receives adequate alveolar ventilation regardless of whether the person can breathe spontaneously.15 For example, FVS might include fully controlled and assist/control positive-pressure ventilation.
Partial ventilatory support is any degree of mechanical ventilation in which set machine rates are lower than 6 breaths/min and the patient participates in the work of breathing (WOB) to help maintain effective alveolar ventilation. A variety of ventilator modes can be used for PVS; however, by definition the patient must actively participate in ventilation to maintain adequate levels of Paco2. PVS modes might include intermittent mandatory ventilation (IMV), pressure support ventilation (PSV), volume support, proportional assist ventilation (PAV), and mandatory minute volume (MMV). All these modes are described later in this chapter.
Strategies for PVS are appropriate when attempts are made to discontinue ventilator support. PVS should be avoided in patients with ventilatory muscle fatigue and when a patient has a high WOB.
When treating patients with acute respiratory failure, the initial goal of mechanical ventilation is to supply all the necessary ventilation (FVS) while the ventilatory muscles are given time to rest.17,18 Ideally, after several hours to several days of FVS, the patient’s condition stabilizes and the patient begins to recover. Maintaining complete rest after just a few days on FVS can result in muscle wasting or atrophy; for this reason, some clinicians object to FVS and provide partial support from the very beginning. This is a matter of the clinician’s preference and the patient’s history. Whether FVS is used or not, the patient assumes part of the WOB within a short time, once other factors have been stabilized to prevent muscle wasting.
Mode of Ventilation and Breath Delivery
The breath type and pattern of breath delivery during mechanical ventilation constitute the mode of ventilation. The mode is determined by the following factors:
• Type of breath (mandatory, spontaneous, assisted)
• Targeted control variable (volume or pressure)
• Timing of breath delivery (continuous mandatory ventilation [CMV], IMV, or spontaneous)
Type of Breath Delivery
Mandatory Breaths
As described in Chapter 3, mandatory breaths are breaths for which the ventilator controls the timing, the tidal volume, or the inspiratory pressure. For example, a patient-triggered, volume-targeted, volume-cycled breath is a mandatory breath. The machine controls tidal volume delivery.
Spontaneous Breaths
For spontaneous breaths, the patient controls the timing and the tidal volume. The volume or pressure (or both) delivered is not preset by the clinician but rather is based on patient demand and the patient’s lung characteristics.
Assisted Breaths
Assisted breaths have characteristics of both mandatory and spontaneous breaths. In an assisted breath, all or part of the breath is generated by the ventilator, which does part of the WOB for the patient. If the airway pressure rises above baseline during inspiration, the breath is assisted.19 For example, during the pressure support mode the clinician sets the target pressure but the patient initiates the breath (patient triggered). The ventilator delivers the set pressure above baseline pressure to assist the patient’s breathing effort. The patient cycles the breath (Case Study 5-1).
Targeting Volume as the Control Variable
By choosing either volume or pressure ventilation, the clinician determines the control variable that will be used to establish gas flow to the patient.20 Control variables are independent variables; in volume-control ventilation, for example, the volume selected is constant and independent of what happens to pressure when the patient’s lung characteristics (lung compliance and Raw) change or when the patient’s effort changes. The selection of using volume or pressure ventilation is based on whether consistency of tidal volume delivery is important or limiting of pressure delivery is important.
The primary advantage of volume-control ventilation is that it guarantees a specific volume delivery and volume of expired gas (VE), regardless of changes in lung compliance and resistance or patient effort.21 The goal of volume-targeted ventilation is to maintain a certain level of Paco2.
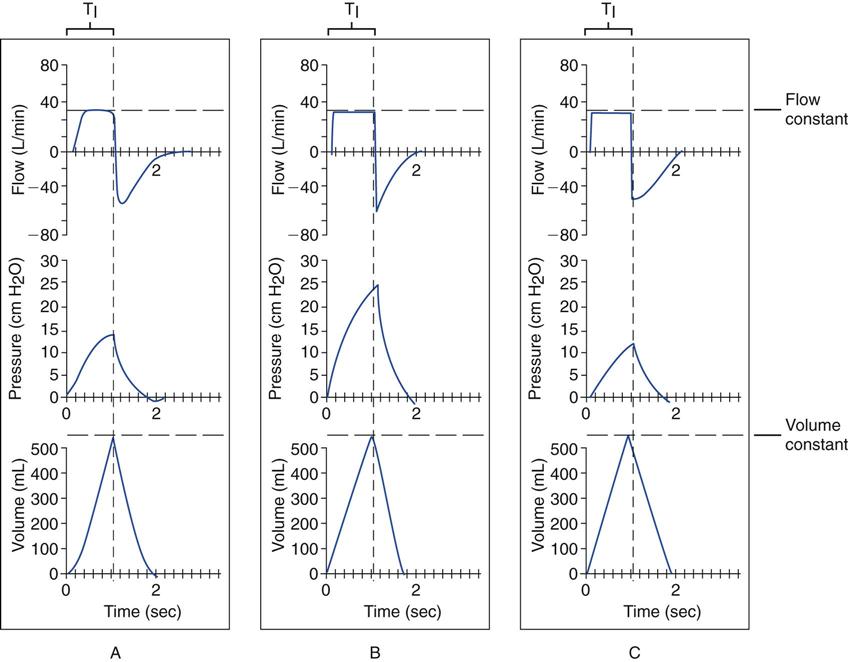
The main disadvantage of volume-targeted ventilation becomes evident when the lung condition worsens. This can cause the peak and alveolar pressures to rise, leading to alveolar overdistention (see Critical Care Concept 5-1 and Fig. 5-1*). Box 5-4 summarizes how changes in lung compliance and airway resistance can affect peak and plateau pressures during volume-controlled ventilation. It is worth noting, however, that these changes are reversible. When the lung condition improves, less pressure is required to deliver the volume, and ventilating pressures decline.
Other disadvantages of volume-controlled breaths are related to flow and sensitivity settings. Specifically, the delivery of flow is fixed on some ventilators and may not match patient demand. Similarly, if the sensitivity level is not set appropriately for the patient, it can make it more difficult for the patient to trigger inspiration. Both situations can lead to patient-ventilator asynchrony and patient discomfort.22,23 The active controls for volume ventilation usually are tidal volume, respiratory rate, inspiratory flow, and a flow pattern. The choice of controls depends on the manufacturer. With some ventilators, the practitioner can set the tidal volume, respiratory rate, and inspiratory time; the flow pattern is not adjustable. (Chapter 6 reviews guidelines for setting the appropriate volume and rate in volume ventilation.)
Targeting Pressure as the Control Variable
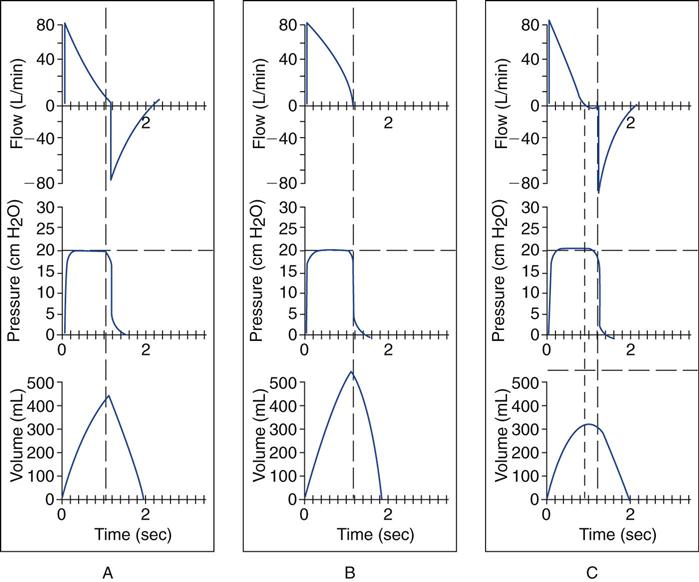
Pressure-control ventilation allows the clinician to set pressure as the independent variable; that is, the pressure remains constant, but volume delivery (the dependent variable) changes as lung characteristics change. Volume delivery therefore must be closely monitored (Critical Care Concept 5-2 and Fig. 5-2).
Pressure-control ventilation has several advantages. First, it allows the clinician to set a maximum pressure, which reduces the risk of overdistention of the lungs by limiting the amount of positive pressure applied to the lung. Second, the ventilator delivers a decelerating flow pattern during pressure-control ventilation (Fig. 5-3). It has been suggested that limiting the peak pressure spares more normal areas of the lungs from overinflation.21 Pressure-control ventilation is therefore considered a component of lung protective strategies.16 It also may be more comfortable for patients who can breathe spontaneously. When the patient makes an inspiratory effort, the negative pressure produced at the upper airway causes the ventilator to vary gas flow to match the patient’s need. This helps reduce WOB, particularly in patients with ARDS, compared with volume-control ventilation.24 Disadvantages of pressure-control ventilation include the following:
• Clinicians are less familiar with pressure-control ventilation (although this is changing).
• VT and  decrease when lung characteristics deteriorate (Box 5-5).
decrease when lung characteristics deteriorate (Box 5-5).
Breath Delivery and Modes of Ventilation
As mentioned previously, the term mode describes a breath type and the timing of breath delivery. Modes of ventilation are often either shorthand terms or acronyms used to describe the way a ventilator performs in a particular situation (i.e., IMV, PSV, VS, PSV, MMV). These terms often are invented by the physicians, therapists, or manufacturers who develop that particular type of ventilation.
The control panel of a ventilator has a dial or touch pad that allows the practitioner to select the mode. Unfortunately, little consistency exists in the way manufacturers name modes; therefore the terminology can be confusing. Basically there are three breath delivery techniques, or modes:
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree