Early reperfusion of the infarct-related coronary artery is an important issue in improvement of outcomes after ST-segment elevation myocardial infarction (STEMI). In this study, the clinical significance of total ischemic time on myocardial reperfusion and clinical outcomes was evaluated in patients with STEMI treated with primary percutaneous coronary intervention and thrombus aspiration and additional triple-antiplatelet therapy. Total ischemic time was defined as time from symptom onset to first intracoronary therapy (first balloon inflation or thrombus aspiration). All patients with STEMI treated with primary percutaneous coronary intervention with total ischemic times ≥30 minutes and <24 hours from 2005 to 2008 were selected. Ischemic times were available in 1,383 patients, of whom 18.4% presented with total ischemic times ≤2 hours, 31.2% >2 to 3 hours, 26.8% >3 to 5 hours, and 23.5% >5 hours. Increased ischemic time was associated with age, female gender, hypertension, and diabetes. Patients with total ischemic times <5 hours more often had myocardial blush grade 3 (40% to 45% vs 22%, p <0.001) and complete ST-segment resolution (55% to 60% vs 42%, p = 0.002) than their counterparts with total ischemic times >5 hours. In addition, patients with total ischemic times ≤5 hours had lower 30-day mortality (1.5% vs 4.0%, p = 0.032) than patients with total ischemic times >5 hours. In conclusion, in this contemporary cohort of patients with STEMI treated with primary percutaneous coronary intervention, triple-antiplatelet therapy, and thrombus aspiration, short ischemic time was associated with better myocardial reperfusion and decreased mortality. After a 5-hour period in which outcomes remain relatively stable, myocardial reperfusion becomes suboptimal and mortality increases.
Early reperfusion of the infarct-related coronary artery is an important issue in the improvement of outcomes after ST-segment elevation myocardial infarction (STEMI). Although the myocardium is damaged during ischemia, it is viable in part early after symptom onset and may be salvaged by rapid reperfusion. The presence of microvascular obstruction increases with longer ischemic times, resulting in an increased infarct size. In previous studies, the best clinical results of reperfusion by primary percutaneous coronary intervention (PCI) have been observed in patients treated within 90 to 120 minutes after symptom onset. Pretreatment with aspirin, heparin, and clopidogrel before hospital admission and the administration of a glycoprotein IIb/IIIa inhibitor during primary PCI is associated with improvements in myocardial reperfusion and clinical outcomes. Furthermore, it has been demonstrated that thrombus aspiration results in an additional improvement of myocardial reperfusion. The application of these innovative pharmacologic and intracoronary treatment strategies could influence the time window to obtain optimal reperfusion and clinical outcomes by primary PCI in patients with STEMI. The aim of this study was to evaluate the impact of total ischemic time on myocardial reperfusion and clinical outcomes in a large contemporary cohort of patients with STEMI treated with primary PCI, thrombus aspiration, and triple-antiplatelet therapy.
Methods
We performed an analysis of ischemic time data from consecutive patients with STEMI presenting to the University Medical Center of Groningen from January 2005 to July 2008. Inclusion criteria were symptoms of chest pain suggestive of acute myocardial infarction lasting ≥30 minutes and <24 hours before hospital admission, electrocardiographic findings of ST-segment elevation >0.1 mV in ≥2 leads, and the performance of a primary PCI procedure. Exclusion criteria were the presence of cardiogenic shock and the existence of a life-threatening disease with a life expectancy of <6 months. Patients treated with acute coronary artery bypass grafting after primary PCI were not enrolled. The University Medical Center of Groningen provides 24-hour emergency cardiac care 7 days a week. It is situated in a region with 750,000 inhabitants and has 7 referral hospitals. When acute coronary syndromes are suspected, 12-lead electrocardiography is performed and the results interpreted by the ambulance physician, aided by a computer algorithm and feedback after fax transmission from our coronary care unit. After confirmation of STEMI, the STEMI treatment protocol is initiated. This includes that the coronary care unit of our center is contacted and informed about the arriving patient, as well as direct activation of the cardiac catheterization team. The patient is directly transported to the catheterization laboratory, thereby bypassing other regional hospitals. In our region, ambulance transfer times vary, to a maximum of 30 minutes. The STEMI protocol was initiated in January 2004 and remained unchanged during the period under study.
All patients were treated with aspirin (500 mg), heparin (5,000 IU), and clopidogrel (600 mg) after confirmation of ST-segment elevation on the first electrocardiogram, usually obtained in the ambulance before hospital admission. During primary PCI, patients received the glycoprotein IIb/IIIa inhibitor abciximab (0.25 mg/kg intravenously) if not contraindicated. Additional heparin was administered during the procedure, guided by the activated clotting time. As the initial step during primary PCI, manual thrombus aspiration was performed in about half of the patients until 2006. After 2006, thrombus aspiration was performed in all patients whenever possible. After the restoration of flow through the infarct-related lesion, a stent was implanted. Balloon pre- and postdilatation were used when necessary to achieve visualization of the infarct-related lesion before stent placement or optimal stent deployment. After primary PCI, patients received aspirin, clopidogrel (>1 month), β blockers, lipid-lowering agents, and angiotensin-converting enzyme inhibitors or angiotensin II receptor blockers.
Total ischemic time was defined as the time from symptom onset to the first intracoronary therapy (first balloon inflation or thrombus aspiration). Information on the time of symptom onset was systematically collected by asking the patient or his or her relatives about the initiation of continuous chest pain before hospital admission.
Angiographic records before and after primary PCI were evaluated by 2 experienced observers blinded for clinical data. On the initial angiogram and on the final angiogram, Thrombolysis In Myocardial Infarction (TIMI) flow grade, angiographic evidence of thrombus in the infarct-related lesion, and distal embolization were assessed. In addition, myocardial blush grade (MBG) was assessed on the angiogram after stenting. The 12-lead electrocardiograms obtained at presentation and 30 to 60 minutes after primary PCI were evaluated by 2 experienced observers blinded to angiographic and clinical data. ST-segment elevation resolution and the presence of Q waves were assessed. Aspirated material was collected and analyzed for patients from 2005 to 2006. Thrombus aspiration was defined as effective when atherothrombotic material was present in the aspirated samples.
Follow-up data at 30 days after primary PCI were collected from hospital records, written questionnaires, and telephone interviews. We report all-cause mortality. Reinfarction was defined as the onset of recurrent symptoms of ischemia combined with new ST-segment elevations and/or a second increase of serum creatine kinase or creatine kinase-MB to ≥2 times the upper limit of the normal range. Target vessel revascularization was defined as PCI or bypass grafting of the infarct-related coronary artery.
The primary end point of our study was optimal myocardial reperfusion, defined as an MBG of 3 and/or ST-segment resolution >70%. Secondary end points were the presence of new Q waves on electrocardiography after primary PCI, enzymatic infarct size as assessed by the maximum creatine kinase-MB level, and mortality, reinfarction, and target vessel revascularization at 30 days after primary PCI.
Patients were classified in 4 time categories of whole hours according to total ischemic time, approaching a distribution in quartiles. Categorical variables are presented as frequency values and proportions, and differences between ischemic time categories were evaluated using chi-square or Fisher’s exact tests. Continuous variables with normal distributions are presented as mean ± SD, whereas variables with non-normal distribution are presented as medians with interquartile ranges. Differences in continuous variables between ischemic time categories were evaluated using 1-way analysis of variance or the Kruskal-Wallis nonparametric test as appropriate. The cumulative incidence of clinical end points was evaluated by the method of Kaplan and Meier, and differences in cumulative event rates according to ischemic time were evaluated using log-rank tests. Univariate and multivariate logistic regression analyses were applied to study the relation between ischemic time and the primary end point, myocardial reperfusion, assessed as MBG of 3 and ST-segment resolution >70%. In multivariate analysis, we adjusted for potential confounders associated with the end points in univariate analysis. We report crude and adjusted odds ratios together with corresponding 95% confidence intervals. For all analyses, 2-sided p values < 0.05 were defined as significant. Statistical analysis was performed using SPSS version 16.0 (SPSS, Inc., Chicago, Illinois).
Results
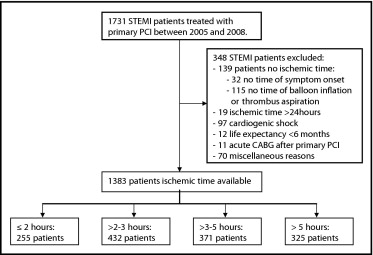
From January 2005 to July 2008, 1,731 consecutive patients with STEMI were treated with primary PCI at our hospital ( Figure 1 ) . Ischemic time was available in 1,383 patients, (79.9%) of all 1731 STEMI patients. Of these, 255 patients (18.4%) had ischemic times ≤2 hours, 432 patients (31.2%) ad times >2 to 3 hours, 371 patients (26.8%) had times >3 to 5 hours, and 325 patients (23.5%) had times >5 hours. The median ischemic time was 3.1 hours (interquartile range 2.3 to 4.8). As listed in Table 1 , prolonged ischemic time was associated with age, female gender, hypertension, diabetes, and smoking status. Angiographic and procedural characteristics are listed in Table 2 . Ischemic time was associated with multivessel disease, the presence of collateral arteries, the use of glycoprotein IIb/IIIa inhibitors, balloon dilatation, and stent implantation. The incidence of TIMI grade 3 flow decreased from 93.3% to 79.9% after 5 hours (p <0.001).
| Variable | Myocardial Ischemic Time (hours) | p Value | |||
|---|---|---|---|---|---|
| ≤2 (n = 255) | >2–3 (n = 432) | >3–5 (n = 371) | >5 (n = 325) | ||
| Ischemic time (hours) | 1.83 (1.50–1.92) | 2.50 (2.25–2.75) | 3.75 (3.33–4.25) | 7.25 (5.87–10.58) | <0.001 |
| Age (years) | 61.6 ± 12.0 | 61.9 ± 12.2 | 62.5 ± 13.0 | 65.2 ± 12.6 | 0.001 |
| Men | 193/255 (75.7%) | 321/432 (74.3%) | 266/371 (71.7%) | 215/325 (66.2%) | 0.006 |
| Hypertension | 84/249 (33.7%) | 143/411 (34.8%) | 118/364 (32.4%) | 139/316 (44.0%) | 0.022 |
| Hypercholesterolemia | 66/217 (30.4%) | 98/357 (27.5%) | 88/315 (27.9%) | 80/280 (28.6%) | 0.763 |
| Diabetes mellitus | 18/254 (7.1%) | 44/426 (10.3%) | 34/368 (9.2%) | 50/323 (15.5%) | 0.003 |
| Myocardial infarction | 18/254 (7.1%) | 42/426 (9.9%) | 36/368 (9.8%) | 31/323 (9.6%) | 0.392 |
| Previous PCI | 18/254 (7.1%) | 28/427 (6.6%) | 25/366 (6.8%) | 20/322 (6.2%) | 0.735 |
| Previous CABG | 4/255 (1.6%) | 9/427 (2.1%) | 15/368 (4.1%) | 10/323 (3.1%) | 0.115 |
| Current smoker | 135/231 (58.4%) | 199/397 (50.1%) | 175/337 (51.9%) | 133/293 (45.4%) | 0.011 |
| Variable | Myocardial Ischemic Time (hours) | p Value | |||
|---|---|---|---|---|---|
| ≤2 (n = 255) | >2–3 (n = 432) | >3–5 (n = 371) | >5 (n = 325) | ||
| Pre-PCI angiography | |||||
| Anterior infarction | 113/255 (44.3%) | 184/432 (42.6%) | 152/371 (41.0%) | 141/325 (43.4%) | 0.763 |
| Multivessel disease | 156/254 (61.4%) | 275/431 (63.8%) | 240/371 (64.7%) | 226/324 (69.8%) | 0.036 |
| Collateral arteries | 65/252 (25.8%) | 95/420 (22.6%) | 91/362 (25.1%) | 108/320 (33.8%) | 0.011 |
| Thrombus before PCI | 141/252 (56.0%) | 236/425 (55.5%) | 211/364 (58.0%) | 181/321 (56.4%) | 0.787 |
| TIMI grade 0 or 1 flow before PCI | 152/253 (60.1%) | 244/428 (57.0%) | 221/369 (59.9%) | 211/323 (65.3%) | 0.096 |
| Procedural | |||||
| Thrombus aspiration | 149/252 (59.1%) | 265/431 (61.5%) | 218/366 (59.6%) | 189/324 (58.3%) | 0.648 |
| Effective | 60/80 (75.0%) | 116/158 (73.4%) | 108/153 (70.6%) | 86/122 (70.5%) | 0.401 |
| Glycoprotein IIb/IIIa inhibitor | 239/253 (94.5%) | 402/430 (93.5%) | 343/369 (93.0%) | 291/325 (89.5%) | 0.022 |
| Balloon dilatation | 123/243 (50.6%) | 216/415 (52.0%) | 203/352 (57.7%) | 211/312 (67.6%) | <0.001 |
| Stent implantation | 231/243 (95.1%) | 397/419 (94.7%) | 330/352 (93.8%) | 284/311 (91.3%) | 0.047 |
| Intra-aortic balloon pump | 6/150 (4.0%) | 14/288 (4.9%) | 14/261 (5.4%) | 15/216 (6.9%) | 0.199 |
| Post-PCI angiography | |||||
| TIMI grade 3 flow after PCI | 236/253 (93.3%) | 385/430 (89.5%) | 321/370 (86.8%) | 259/324 (79.9%) | <0.001 |
| Distal embolization after PCI | 15/233 (6.4%) | 33/389 (8.5%) | 21/348 (6.0%) | 23/300 (7.7%) | 0.925 |
| Thrombus after PCI | 3/253 (1.2%) | 6/431 (1.4%) | 10/370 (2.7%) | 9/323 (2.8%) | 0.082 |
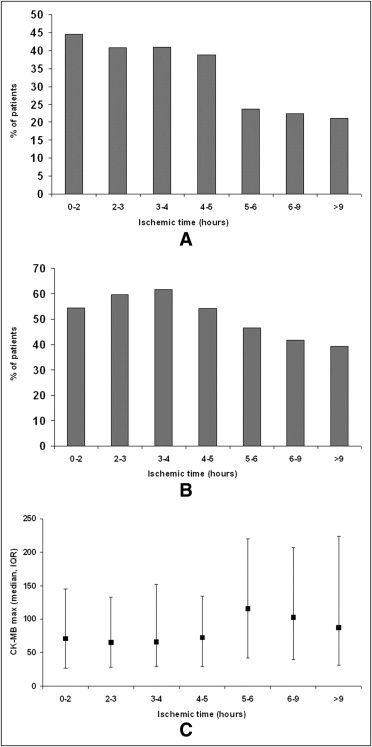
MBG was analyzed in 1,358 patients (98.2%) after primary PCI. In the first 5 hours of ischemic time, MBG of 3 varied from 44.6% to 40.1% but decreased to 22.3% after 5 hours (p <0.001; Table 3 , Figure 2 ). ST-segment resolution could be analyzed in 1,243 patients (89.9%). Complete ST-segment resolution varied from 54.5% to 59.8% in the first 5 hours but decreased to 42.4% after 5 hours (p <0.001; Table 3 , Figure 2 ). Multivariate analysis showed that after correction for predictive baseline and procedural variables in the univariate analysis, ischemic time was a significant predictor of MBG of 3 and ST-segment resolution >70% ( Table 4 ). In addition, the presence of Q waves and the maximum value of creatine kinase-MB were associated with prolonged total ischemic time ( Table 3 , Figure 2 ).
| Variable | Myocardial Ischemic Time (hours) | p Value | |||
|---|---|---|---|---|---|
| ≤2 (n = 255) | >2–3 (n = 432) | >3–5 (n = 371) | >5 (n = 325) | ||
| Myocardial reperfusion | |||||
| MBG 3 | 112/251 (44.6%) | 173/425 (40.7%) | 146/364 (40.1%) | 71/318 (22.3%) | <0.001 |
| ST-segment resolution >70% | 126/231 (54.5%) | 234/391 (59.8%) | 197/333 (59.2%) | 122/288 (42.4%) | 0.002 |
| Measures of infarct size | |||||
| Q waves | 186/238 (78.2%) | 315/403 (78.2%) | 268/343 (78.1%) | 251/295 (85.1%) | 0.047 |
| Creatine kinase-MB maximum (U/L) | 71.0 (26.9–145.0) | 65.5 (28.0–132.8) | 68.9 (29.1–147.7) | 98.2 (36.0–222.3) | <0.001 |
| Clinical outcome at 30 days | |||||
| Mortality | 4/255 (1.6%) | 6/430 (1.4%) | 6/371 (1.6%) | 13/325 (4.0%) | 0.032 |
| Reinfarction | 4/255 (1.6%) | 3/430 (0.7%) | 6/371 (1.6%) | 5/325 (1.5%) | 0.647 |
| Target vessel revascularization | 11/255 (4.3%) | 14/430 (3.3%) | 22/371 (5.9%) | 19/325 (5.8%) | 0.134 |

Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


