The Platelet Inhibition and Patient Outcomes (PLATO) trial showed that ticagrelor reduced the risk for cardiovascular events in patients with acute coronary syndromes compared to clopidogrel but was associated with increased incidence of dyspnea. This substudy assessed whether ticagrelor affects pulmonary function in patients with acute coronary syndromes: 199 patients enrolled in the PLATO trial and receiving randomized treatment with ticagrelor 90 mg twice daily (n = 101) or clopidogrel 75 mg/day (n = 98) took part in the pulmonary function substudy. Patients with advanced lung disease, congestive heart failure, or coronary artery bypass graft surgery after the index event were excluded. Pulse oximetry (blood oxygen saturation), spirometry (forced expiratory volume in 1 second, forced vital capacity, and forced expiratory flow between 25% and 75% of forced vital capacity before and 20 minutes after inhalation of a β 2 agonist), lung volumes (total lung capacity, functional residual capacity, residual volume), and diffusion capacity were performed after patients received study medication for 30 to 40 days. Tests were then repeated <10 days before and approximately 30 days after the discontinuation of study medication. After a mean treatment duration of 31 days, there were no differences between the groups for any of the pulmonary function parameters. At the end of treatment (mean 211 days) and after the discontinuation of study medication (mean 32 days after the last dose), there was also no evidence of a change in pulmonary function in either group. For example, forced expiratory volume in 1 second values before β 2 agonist inhalation in the ticagrelor and clopidogrel groups were 2.81 ± 0.73 and 2.70 ± 0.84 L, respectively, at the first visit and did not change significantly at subsequent visits. In conclusion, no effect of ticagrelor on pulmonary function was seen in this cohort of patients with acute coronary syndromes compared to clopidogrel.
Ticagrelor is an oral, reversibly binding platelet P2Y 12 receptor inhibitor that yields greater inhibition of platelet aggregation than clopidogrel and has been shown in the Platelet Inhibition and Patient Outcomes (PLATO) study to reduce the risk for major adverse cardiovascular events in patients with acute coronary syndromes (ACS) compared to clopidogrel. Dyspnea can occur as an adverse effect of ticagrelor therapy, tends to occur early in the course of treatment, and is usually of mild or, less frequently, moderate severity. Despite the more common occurrence of episodes of dyspnea with ticagrelor compared to clopidogrel and placebo in a prospective study in patients with stable coronary artery disease, there were no changes of cardiac or pulmonary function measurements, including measures of left ventricular function, spirometry, and pulmonary diffusion. Consequently, the mechanism for ticagrelor-related dyspnea remains to be established. To extend the findings in patients with stable CAD, we performed a pulmonary function substudy in ticagrelor- and clopidogrel-treated patients with ACS participating in the PLATO study.
Methods
The design of the PLATO study has been reported previously. In brief, patients with moderate- to high-risk non–ST-segment elevation ACS or ST-segment elevation myocardial infarction planned for primary percutaneous coronary intervention were randomized to receive either clopidogrel or ticagrelor for up to 12 months. Patients with histories of dyspnea and/or histories of heart failure, asthma, chronic obstructive pulmonary disease or other respiratory diseases were included. This pulmonary function substudy was performed at 15 centers in 5 countries (the Czech Republic, Hungary, India, Poland, and the United States). Patients were invited to participate either at enrollment into the main study or any time during the first month of study treatment and provided informed consent according to a protocol approved by the local ethics committee or internal review board. Additional inclusion criteria for the substudy were the provision of informed consent for the substudy and ability to perform the pulmonary function tests, while additional exclusion criteria were discontinuation of study medication before the first pulmonary function assessment, advanced lung disease such as chronic obstructive pulmonary disease or asthma requiring, in the past year, oral steroid medication or an emergency room visit, any unstable medical condition that in the judgment of the clinician would confound the results of pulmonary function under study, symptomatic heart failure, or coronary artery bypass graft surgery performed for the index event.
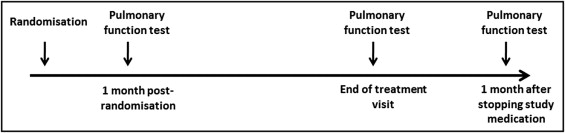
The primary objective of this study was to evaluate the effects of ticagrelor in comparison to clopidogrel on forced expiratory volume in 1 second (FEV 1 ) after the completion of study treatment (6, 9, or 12 months depending on phase of entry into the PLATO study). The secondary objectives were (1) to compare the effects of ticagrelor and clopidogrel on FEV 1 after 1 month of treatment and 1 month after the discontinuation of treatment and (2) to compare the effects of ticagrelor and clopidogrel on other measures of pulmonary function (including other spirometric measures, lung volumes, oxygen saturation, and diffusion capacity). Because it was not feasible to study pulmonary function in an ACS population before the administration of study medication, the first assessment of pulmonary function was performed at approximately 30 days (range 30 to 40) after randomization, and further assessments were performed at the end of study treatment (<10 days before the discontinuation of treatment) and approximately 30 days after the discontinuation of study treatment ( Figure 1 ) . The following order of pulmonary function tests were performed: (1) blood oxygen saturation (SpO 2 ) using pulse oximetry; (2) functional residual capacity, total lung capacity, and residual volume by plethysmography; (3) single-breath diffusion capacity for the lungs, measured using carbon monoxide; and (4) FEV 1 , forced vital capacity, mean forced expiratory flow between 25% and 75% of forced vital capacity before and 20 minutes after inhalation, via metered-dose inhaler and spacer device, of a short-acting β 2 agonist such as salbutamol or albuterol.
Observed values for pulmonary function variables are presented as mean ± SD for data collected at each visit. Additionally, the percentage of predicted normal values for FEV 1 were calculated to correct for differences in baseline demographics. Actual FEV 1 and the percentage of predicted normal FEV 1 were analyzed using analysis of covariance adjusting for the variables of treatment, age, gender, and height. The number of patients in each group showing >10% increases in FEV 1 over time was determined. One hundred twenty-five patients were required in each group to detect a 25-ml difference in FEV 1 between treatment groups at 80% power and a significance level of 0.05.
Results
Five participating countries enrolled 199 patients (101 in the ticagrelor group and 98 in the clopidogrel group); 166 patients (80 ticagrelor, 86 clopidogrel) completed the end-of-treatment visit after a mean duration of study treatment of 211 days, while 5 patients missed the visit without withdrawing from the study and 28 patients withdrew from the study before this visit (17 ticagrelor, 11 clopidogrel) because of withdrawal of consent (13 ticagrelor, 9 clopidogrel), severe noncompliance (1 ticagrelor), or adverse events or safety concerns (3 ticagrelor, 2 clopidogrel); and 147 patients (71 ticagrelor, 76 clopidogrel) completed the final visit at a mean of 32 days after the discontinuation of study treatment, while 22 patients (12 ticagrelor, 10 clopidogrel) withdrew from the study before the final visit and 2 patients missed the visit without withdrawing consent. Recruitment was less than intended, because the start of the study was delayed and recruitment into the main study was completed before the intended sample size could be reached. Baseline demographic data were well matched between the 2 groups ( Table 1 ). The median duration of treatment with study medication was 191 days in the ticagrelor group (range 93 to 289) and 189 days in the clopidogrel group (range 121 to 286).
| Characteristic | Ticagrelor | Clopidogrel |
|---|---|---|
| (n = 101) | (n = 98) | |
| Age (years) | 59 ± 11 | 60 ± 11 |
| Men | 79 (78%) | 79 (81%) |
| Caucasian | 90 (89%) | 88 (90%) |
| Asian or Asian American | 11 (11%) | 9 (9%) |
| African American | 0 | 1 (1%) |
| Weight (kg) | 80 ± 14 | 82 ± 16 |
| Nonsmoker | 39 (39%) | 42 (43%) |
| Ex-smoker | 37 (37%) | 31 (32%) |
| Occasional smoker | 0 | 1 (1%) |
| Habitual smoker | 25 (25%) | 24 (25%) |
| Unstable angina pectoris | 12 (12%) | 11 (11%) |
| NSTEMI | 15 (15%) | 24 (25%) |
| STEMI | 74 (73%) | 61 (62%) |
| Other final diagnosis | 0 | 2 (2%) |
| Current dyspnea at enrollment in pulmonary substudy | 4 (4%) | 6 (6%) |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


