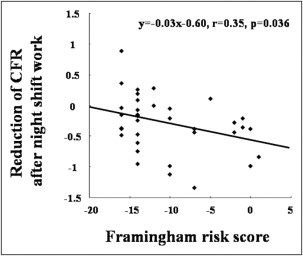
Nightshift work, which is known to cause mental stress and disrupt normal biological diurnal rhythms, leads to endothelial dysfunction resulting in increased risk for cardiovascular disease. This study aimed to investigate the acute effect of night-shift work on coronary microcirculation through assessment of coronary flow reserve (CFR) by transthoracic Doppler echocardiography. This study consisted of 36 women nurses who underwent transthoracic Doppler echocardiographic examinations after working a nightshift and on a regular day without previous nightshift work. Flow velocity in the distal portion of the left anterior descending coronary artery was measured at baseline and during adenosine infusion. CFR was calculated as the ratio of hyperemic to basal mean diastolic flow velocity. CFR after night work was lower than that on a regular workday (3.8 ± 0.6 vs 4.1 ± 0.6, p <0.001). Degree of decreases in CFR after night work was correlated to Framingham risk score (r = 0.35, p = 0.036). In conclusion, this study demonstrated that coronary microcirculation was impaired after nightshift work in women nurses.
Nightshift work is known to cause disturbances in normal circadian rhythms of various psychophysiologic functions beginning with sleep deprivation and inevitable mental stress. Previous studies have reported that nightshift work is associated with increased risk for cardiovascular disease and other long-term conditions such as hypertension, glucose intolerance, and depression. Presence of endothelial dysfunction is an independent predictor of future cardiovascular events in patients with or at high risk for cardiovascular disease. Several investigations have demonstrated impaired peripheral vascular endothelial function after nightshift work in medical personnel. This study therefore aimed to investigate whether coronary microcirculation was impaired after nightshift work in women nurses and, if so, to study its relation to clinical characteristics and neural and humoral processes including Framingham risk score, adrenal function, and estradiol concentration.
Methods
This study consisted of 36 women nurses (mean age 32 ± 9 years). Coronary flow reserve (CFR) in the left anterior descending coronary artery was estimated and represented the status of coronary microcirculation. CFR was measured noninvasively by transthoracic Doppler echocardiography (TTDE) at approximately 9 a . m . in each subject at the following time points: (1) on a regular day without previous nightshift work (baseline) and (2) after working a nightshift. Blood samples were taken immediately before each CFR examination. Smoking was not permitted during the protocol. The presence or absence of the following 5 cardiovascular risk factors in each subject was evaluated using medical records: hypertension, hypercholesterolemia, diabetes, smoking, and obesity (body mass index >30 kg/m 2 ). Framingham risk score was then calculated. The study was approved by the institutional review board of each participating institution. Written informed consent for participation was obtained from each subject.
TTDE was performed using a Sequoia 512 (Siemens Medical Solutions, Mountainview, California) or a Vivid 7 (GE Medical Systems, Milwaukee, Wisconsin) as previously described. Coronary blood flow velocity in the distal portion of the left anterior descending coronary artery coronary artery was estimated at baseline and after intravenous infusion of adenosine triphosphate (ATP) at a rate of 140 μg/kg per minute for 2 minutes to produce hyperemia. CFR was calculated as the ratio of hyperemic to basal mean diastolic flow velocity (MDFV).
Values were expressed as mean ± SD. Comparisons of laboratory and echocardiographic data between 2 time points were made with paired t test. Linear regression analysis was used for correlation of variables of interest. Differences in hemodynamics and transthoracic Doppler echocardiographic results after ATP infusion between the 2 time points were evaluated by 2-way repeated-measures analysis of variance testing for group effect (2 different times), ATP effect, and interaction. Differences were considered statistically significant at a p value <0.05.
Results
All subjects had no history of cardiovascular disease and none were taking any medications except for hypercholesterolemia in 1 subject, smoking in 8 subjects, and hypercholesterolemia and smoking in 1 subject. These subjects did not receive contraceptive hormonal therapy. Mean body mass index was 20.9 ± 3.4 kg/m 2 . All subjects had normal results on their echocardiographic examinations. Average duration of nightshift work was 7.6 ± 6.1 years (range 0.1 to 23) and mean number of nightshifts per month was 5.4 ± 1.9 times the level observed at the start of the study. Tables 1 and 2 present baseline hemodynamic and laboratory results, respectively. Because young nurses working the nightshift were enrolled in this study, mean Framingham risk score was low (−10.4 ± 5.6, range −16 to 1).
| Variable | Regular Workday | After Nightshift Work | Overall p Value ⁎ |
|---|---|---|---|
| Heart rate (beats/min) | |||
| Baseline | 69 ± 10 | 67 ± 9 | 0.5 |
| Adenosine triphosphate infusion | 73 ± 10 | 73 ± 10 | |
| Systolic blood pressure (mm Hg) | |||
| Baseline | 101 ± 13 | 101 ± 11 | 0.8 |
| Adenosine triphosphate infusion | 97 ± 11 | 97 ± 13 | |
| Mean diastolic flow velocity (cm/s) | |||
| Baseline | 0.17 ± 0.04 | 0.16 ± 0.04 | 0.06 |
| Adenosine triphosphate infusion | 0.67 ± 0.18 | 0.60 ± 0.15 |
⁎ Interaction of nightshift work with adenosine triphosphate effect by 2-way repeated-measures analysis of variance.
| Variable | Regular Workday | After Nightshift Work | p Value |
|---|---|---|---|
| Leukocyte count (/mm 3 ) | 6,079 ± 1886 | 6,013 ± 1900 | 0.8 |
| High-sensitive C-reactive protein (mg/dl) | 0.082 ± 0.11 | 0.089 ± 0.13 | 0.5 |
| Total cholesterol (mg/dl) | 184 ± 24 | 183 ± 29 | 0.7 |
| Low-density lipoprotein cholesterol (mg/dl) | 100 ± 20 | 99 ± 25 | 0.6 |
| High-density lipoprotein cholesterol (mg/dl) | 67 ± 14 | 67 ± 14 | 0.9 |
| Triglyceride (mg/dl) | 70 ± 34 | 65 ± 43 | 0.3 |
| Glucose (mg/dl) | 96 ± 12 | 92 ± 7 | 0.1 |
| Estradiol (pg/ml) | 119 ± 118 | 102 ± 111 | 0.4 |
| Cortisol (μg/dl) | 11 ± 5 | 10 ± 3 | 0.3 |
| Norepinephrine (pg/ml) | 238 ± 170 | 235 ± 168 | 0.8 |
| Epinephrine (pg/ml) | 31 ± 36 | 31 ± 20 | 0.9 |
Results of CFR measurements are summarized in Figure 1 . CFR was lower after nightshift work than on a regular workday. Values of MDFV before and after ATP infusion at 2 different time points are listed in Table 1 . Two-way analysis of variance showed no significant interaction in MDFV between the 2 groups during ATP infusion. Tables 1 and 2 present results of hemodynamics and laboratory tests, respectively. There were no significant interactions in heart rate and systolic blood pressure between the 2 groups during ATP infusion. There was no significant difference in any laboratory variable between the 2 time points.

Ten subjects who had hypercholesterolemia and/or smoking tended to have larger decreases of CFR after nightshift work than other subjects (−0.48 ± 0.38 vs −0.23 ± 0.47, p = 0.1). Degree of decreases in CFR after nightshift work was correlated to Framingham risk score as shown in Figure 2 . There were no significant relations between degree of decreases in CFR after night work and other clinical and laboratory parameters ( Table 3 ).
| Variable | r | p Value |
|---|---|---|
| Age | 0.01 | 0.9 |
| Duration of nightshift work | 0.04 | 0.8 |
| Number of nightshifts per month | 0.02 | 0.9 |
| Body mass index | 0.20 | 0.2 |
| Systolic blood pressure | 0.06 | 0.7 |
| Leukocyte count | 0.05 | 0.8 |
| High-sensitive C-reactive protein | 0.1 | 0.5 |
| Total cholesterol | 0.32 | 0.05 |
| Low-density lipoprotein cholesterol | 0.31 | 0.06 |
| High-density lipoprotein cholesterol | 0.04 | 0.8 |
| Triglyceride | 0.04 | 0.8 |
| Glucose | 0.03 | 0.9 |
| Estradiol | 0.08 | 0.6 |
| Cortisol | 0.2 | 0.2 |
| Norepinephrine | 0.05 | 0.8 |
| Epinephrine | 0.1 | 0.6 |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


