25
Pulmonary Hypertension
 Pulmonary Hypertension and Right Heart Failure
Pulmonary Hypertension and Right Heart Failure
PH is a disorder where flow to the pulmonary arterial circulation is restricted related to increased pulmonary vascular resistance (PVR), ultimately leading to right heart failure. The pulmonary circulation is normally a low-pressure, low-resistance circulation. Mild PH is generally defined as a mean pulmonary artery pressure (mPAP) above 25 mmHg at rest and PVR greater than 300 dynes·sec·cm−5 (>3.75 Wood units), whereas severe PH constitutes mPAP above 50 mmHg and PVR greater than 600 dynes·sec·cm−5 (>7.5 Wood units). 1
1. Idiopathic pulmonary arterial hypertension (IPH), familial pulmonary hypertension (FPH), and PH associated with conditions such as connective tissue disorders, portal hypertension, pulmonary veno-occlusive disease, HIV, and anorexigens
3. PH with lung diseases and/or hypoxemia
4. PH due to chronic thromboembolic disease
 Pathophysiology
Pathophysiology
PH is a panvasculopathy, mostly affecting small and medium-sized arterial vessels with a wide range of abnormalities, including intimal hyperplasia, medial hypertrophy, adventitial proliferation, and plexiform arteriopathy. Multiple pathogenic pathways have been implicated in the development of PH. There is a vasoconstriction phase, starting with altered vascular endothelial and smooth muscle function, leading to vasoconstriction and localized thrombosis. With progression of the disease, vascular remodeling, proliferation, and formation of plexiform lesions 3 result in increased PVR and end with right heart failure and death. The plexiform lesion, a histologic hallmark of FPH and IPH, is a result of monoclonal proliferation of endothelial cells and migration and proliferation of smooth muscle cells. 4 The basis for current medical therapies is that endothelial dysfunction leads to an imbalance between vasoconstrictors (endothelin 1, thromboxane A2) and vasodilators (prostacyclin, nitric oxide). 5
The endothelium releases thromboxane A2, which is a potent vasoconstrictor, cell proliferator, and powerful platelet activator, in addition to prostacyclin, a potent vasodilator and inhibitor of platelet aggregation. 6 This mediator imbalance results in pulmonary vasoconstriction, disordered endothelial cell proliferation, and proliferation of intimal cells, leading to the characteristic plexiform lesions.
 Clinical Manifestations
Clinical Manifestations
Physical examination focuses on signs of both PH and right heart failure. Accentuation of the pulmonic component of the second heart sound and an early systolic murmur reflecting tricuspid regurgitation (that enhances with spontaneous inspiration) might be the only findings on physical exam. Jugular venous distention, hepatojugular reflux, peripheral edema, hepatomegaly, and ascites are signs of advanced PH.7,8 Correct evaluation is essential for appropriate management, and echocardiography is the most appropriate next step. Findings such as RV hypertrophy and/or dilation, LV filling impairment, or paradoxical interventricular septal motion are indicative of right heart failure. To confirm the diagnosis, a right heart catheterization (RHC) assessment of PVR, right atrial (RA) and RV pressures, and LV pressures is required.
 Right Ventricle and Pathophysiology of Right Heart Failure
Right Ventricle and Pathophysiology of Right Heart Failure
An encircling muscular band separates the RV into the inflow portion, the sinus, and the outflow portion (or conus). This muscular band is referred to as the crista supraventricularis and is made up of the infundibular septum and the parietal band. Two other muscular bands are present in the RV: the septal and moderator bands. The moderator band is an important landmark of the RV that is well visualized by echocardiography. It is attached to the right ventricular outflow tract (RVOT) and runs from the septum to the anterior RV wall.9,10
The RV contracts in a fashion resembling peristalsis, beginning with contraction of the inlet portion, followed by the apex, and ending with contraction of the infundibulum. It pumps on average the same stroke volume as the LV but generates only about 25% of the stroke work, owing to the low-pressure, low-resistance, and high-compliance nature of the pulmonary circulation. 11 As a result, the normal RV’s wall thickness is half that of the LV and accordingly more compliant. Because of the RV’s reduced contractile reserve compared to the LV’s, it is much more sensitive to increases in afterload. Functionally and anatomically, the RV is adapted for generation of sustained low-pressure perfusion. 12 The dissimilarity in ventricular afterload is responsible for the difference in ventricular pressure-volume loops between the two ventricles. The LV has a square-shaped pressure-volume loop, whereas the RV pressure-volume loop is triangular. The triangular shape depicts the shorter pre-ejection period that is due to the RV systolic pressure, which rapidly exceeds pulmonary artery diastolic pressure. This means the normal RV has a longer period of ejection and shorter periods of isovolumic contraction and relaxation. 13 The RV pressure-volume loop becomes more square shaped with increases in RV afterload. In addition, the orientation of the interventricular septum (IVS) and geometry of the ventricles change with any increase in RV volume or pressure overload. 14
Ventricular interdependence results from the close anatomic association between the LV and RV; they share the IVS and are enclosed within the same pericardial sac. The IVS contributes to both LV and RV function15,16 and is responsible for approximately one third of the RV stroke work under normal conditions; it is a major determinant of overall RV performance. 17 Ventricular interdependence is mediated mainly through the IVS and plays an essential part in the pathophysiology of RV dysfunction. In the setting of RV infarction and loss of RV free wall contractility, it is the septum that continues to generate RV systolic pressure. RV ejection fraction (RVEF) is very sensitive to increases in RV afterload (i.e., pulmonary artery pressures); high afterload leads to increased RV wall tension and oxygen demand and RV ischemia. As the RV enlarges to accommodate the increase in pressure, this results in dilation of the tricuspid annulus and creates tricuspid regurgitation (TR). Eventually this results in a rise in RV end-diastolic and RA pressures, with associated clinical signs of RV failure. 18 Whereas the RV is normally perfused during both diastole and systole, the systolic component becomes compromised with raised chamber pressures. 19 Thus, maintaining perfusion pressure is essential, especially when RV systolic pressure is elevated. Vlahakes et al. examined the mechanism of RV failure in dogs under anesthesia and the importance of maintaining perfusion pressure. After producing RV failure with increasing PA pressures, infusion of phenylephrine raised aortic pressure, thereby increasing myocardial perfusion pressure and reversing RV failure, as shown by the increase in cardiac output. 20
Normally the IVS is shifted toward the RV free wall during systole and diastole, which contributes to RV ejection. However, in conditions with increased RV pressure or volume overload, the IVS paradoxically shifts toward the LV. The shifted septum alters LV geometry, leading to decreased LV preload, increased LV end-diastolic pressure, low cardiac output, and a diminished contribution to RV ejection. 21 As noted earlier, systemic vasoconstrictors and maintenance of perfusion pressure can be used to restore RV ejection and blood supply.22,23
 Echocardiographic Examination of the Pulmonary Hypertensive Patient
Echocardiographic Examination of the Pulmonary Hypertensive Patient
Echocardiographic evaluation of patients with PH includes a complete exam with particular focus on the right side of the heart. This includes examining the anatomy and function of the RA and RV (including their influence on left heart function), the TV and PV, and connecting vascular structures (superior and inferior venae cavae [SVC, IVC], pulmonary artery [PA]). The following is a brief description of the standard echocardiographic views required for evaluation of the right heart, as well as detailed descriptions of evaluating these structures in patients with PH. In addition, Kasper et al. have described five additional views of the right heart, of which three specifically increase visualization of the RV myocardium and evaluation of the PV. 24 Use of echocardiography in estimating right heart hemodynamics will also be discussed.
Standard Transesophageal Echocardiographic Views
• Transgastric (TG) mid-papillary short-axis view demonstrates the anterolateral position of the RV in relation to the LV, as well as ventricular interdependence.
• TG RV inflow view shows a “two-chamber” view of the right heart with a focus on the TV, subvalvular apparatus, and RV free wall.
• Midesophageal (ME) four-chamber view displays both the RA and RV in relation to the left atrium (LA) and LV and allows for evaluation of chamber sizes, function, and anatomic variants.
• ME RV inflow-outflow view demonstrates the “wrapping” nature of the RA, RV, and PA in relation to the left heart. This view allows assessment of the RA, TV, RV, PV, and PA.
• ME bicaval view displays the LA, RA, and their separation, the interatrial septum. The SVC and IVC, as well as RA appendage, are in view in the standard bicaval view, and a modified view can reveal the coronary sinus and TV.
• ME ascending aortic short-axis view shows the relationship of the main and right PA to the ascending aorta and SVC, useful in identifying PA dilation and PA thrombus.
• ME ascending aortic long-axis view is similar to the short-axis view, with a focus on of the right PA and ascending aorta.
• Upper esophageal (UE) aortic arch short-axis view demonstrates the main PA, PV, and the distal RVOT in some patients. These structures are often in parallel alignment with the ultrasound beam, ideal for Doppler interrogation.
Additional Transesophageal Echocardiographic Views
• TG RV basal short-axis view demonstrates an en face view of the TV as well as the basal septal and free wall portions of the RV.
• TG RV apical short-axis view demonstrates a short-axis cross-section of the RV including apical septal and free wall portions.
• TG RV inflow-outflow view provides an orientation of the pulmonary valve that is ideal for Doppler interrogation.
• Deep TG RV inflow-outflow view provides another parallel view of the pulmonary valve for Doppler interrogation and often provides a portion of the TV annulus for M-mode or tissue Doppler interrogation.
• Deep TG RV outflow view demonstrates the RVOT, often with a parallel orientation for Doppler interrogation.
Right Ventricle
In response to chronically elevated RV afterload, the RV exhibits several changes readily identified by echocardiography. The responses are generally seen as volume-accommodating dilatory changes and pressure-related changes such as RV enlargement, hypertrophy, and abnormal septal motion. With increasing severity and chronicity of PH, RV failure ensues, and this is evident on echocardiography as RV systolic failure. The adaptive changes of the RV are described next.
Right Ventricular Enlargement
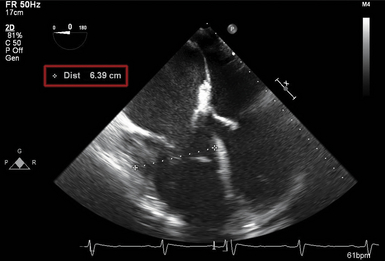
Chronic pressure and volume overload of the RV leads to a dilated chamber that is rapidly and easily appreciated on echocardiography. RV size is typically qualitatively assessed in the ME four-chamber view via comparison with LV size. At end-diastole, the normal RV typically occupies two thirds of the cross-sectional area of the LV area. With mild enlargement, the RV increases in size greater than two thirds of the LV area. With moderate enlargement, the RV is equal in cross-sectional area. Severe enlargement yields an RV that is larger in cross-sectional area than the LV ( Fig. 25-1 and Video 25-1 ![]() ). RV size may be rapidly assessed via the appearance of the cardiac apex in the ME four-chamber view. Typically, the LV forms the cardiac apex. With RV enlargement, however, the RV may share the cardiac apex. With severe enlargement, the RV may completely occupy the cardiac apex in that echocardiographic view.
). RV size may be rapidly assessed via the appearance of the cardiac apex in the ME four-chamber view. Typically, the LV forms the cardiac apex. With RV enlargement, however, the RV may share the cardiac apex. With severe enlargement, the RV may completely occupy the cardiac apex in that echocardiographic view.
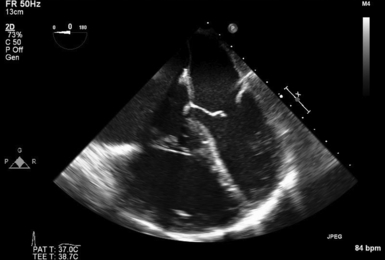
Figure 25-1 Midesophageal four-chamber view of patient with chronic thromboembolic pulmonary hypertension (CTEPH) and resulting severe right ventricular (RV) enlargement. Note that cross-sectional area of RV exceeds cross-sectional area of left ventricle. (See Video 25-1 ![]() .)
.)
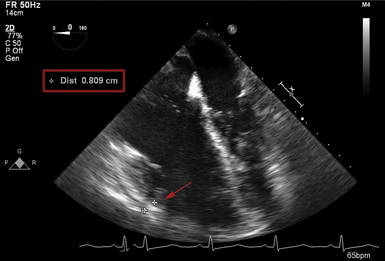
Quantitatively, the RV is difficult to assess owing to its asymmetric shape, and its size is frequently underestimated. Although specific normal RV dimensions have not been established for transesophageal echocardiography (TEE), the American Society of Echocardiography (ASE) has suggested a transthoracic apical four-chamber measurement of the RV basal dimension (within the basal third of the RV) with an upper reference limit of 4.2 cm ( Fig. 25-2). 24 For longitudinal measurements, the suggested upper reference limit is 8.6 cm.
Right Ventricular Hypertrophy
In response to chronically elevated RV afterload, the RV myocardium hypertrophies. This may be demonstrated on echocardiography as RV free wall thickness greater than 5 mm at end-diastole ( Fig. 25-3). Long-standing severe chronic PH may result in RV hypertrophy exceeding 10 mm. This measurement may be obtained in the ME four-chamber view, the ME RV inflow-outflow view, or the TG mid-papillary view, often aided by the use of M-mode echocardiography. Hypertrophy of the RV includes the encircling bands, yielding an often easily identified hypertrophied moderator band near the RV apex ( Fig. 25-4 and Video 25-2 ![]() ).
).