Chapter 2 Principles of Cellular Architecture and Physiology with Applications in Electrophysiology
Specialized Excitable Cells Tightly Regulate Cardiac Depolarization
The highly coordinated and efficient propagation of electrical activity through the heart is maintained by the combined activities of a diverse set of specialized excitable cardiac cells, each with its own structural, electrical, and molecular signature. The cardiac sinoatrial (SA) node, a small group of spontaneously active cells in the right atria, is the primary initiation site of cardiac electrical activity because of its relatively positive threshold potential.1 Once generated by the sinus node, the cardiac action potential propagates through the atria to the atrioventricular (AV) node (the maximum diastolic potential of the AV node is only slightly more negative than that of the SA node), a second small but critical group of specialized cells that display slow conduction properties preventing inappropriate depolarization of the ventricles. In fact, the slow conduction of the AV node is a critical safeguard against the development of ventricular arrhythmias from pathologic atrial pacing defects (i.e., atrial flutter/fibrillation). After the AV node, the cardiac action potential propagates through the cardiac conduction system comprising the AV bundle (bundle of His), the left and right bundle branches, and the cardiac Purkinje system. Interestingly, this conduction system, particularly the cardiac Purkinje fibers, has evolved to rapidly propagate cardiac electrical activity at up to 2 to 4 m/s for the nearly instantaneous spread of depolarization through the sub-endocardium of the left and right ventricles.2 In comparison with the rapid conduction pathways of the Purkinje system, left ventricular tissue conduction velocity is significantly slower (0.3 to 1 m/s).2 Importantly, Purkinje fibers communicate with the ventricular mass at well-defined discrete loci (Purkinje-muscle junctions).
Form Fits Function: The Ventricular Cardiomyocyte and Excitation-Contraction Coupling
As is discussed in detail in Chapter 3, the electrical activity of cardiac cells (the action potential) is primarily modulated by the coordinated movement of sodium (Na+), calcium (Ca2+), and potassium (K+) across the external plasma membrane (sarcolemma) and the internal sarcoplasmic reticulum (SR) membrane. The specialized function of each cardiac cell type is the result of the evolution of specific molecular and structural components that regulate ion flux across the membrane and dictate specific cell properties.3 In this section, the primary structural and molecular components of different cardiac cells is discussed in relation to cell type–specific action potentials. Because of its central role in cardiac excitability, the ventricular cardiomyocyte will be used as the central point of comparison for other excitable cardiac cell types.
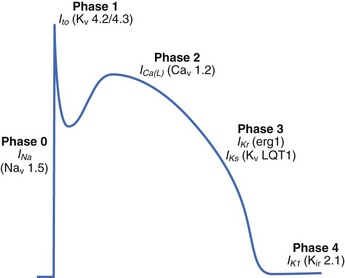
The ventricular action potential is notable for its hyperpolarized resting membrane potential, rapid upstroke, and prolonged plateau (Figure 2-1). The resting membrane potential of the ventricular cardiomyocyte (held at ~–90 mV, roughly 30 mV more negative than the human sinus node) is the most negative of all excitable cell types (hence the final cell type to depolarize), primarily because of a large inwardly rectifying K+ current, IK1, prominently expressed in these cells.4 The rapid upstroke, because of the presence of rapidly activating voltage-gated Na+ channels, allows for rapid propagation of the electrical signal through the ventricles, which is required for synchronized muscle contraction. Finally, the extended plateau allows sufficient time for Ca to enter the cell and signal contraction.3
Once the excitation reaches the ventricles through the cardiac conduction system (see above), the electrical signal passes from cell to cell as a flux of ions through specialized intercellular ion channels called gap junctions (discussed in detail below). This flow of ions into the cell from neighboring activated cells depolarizes the membrane potential. If the membrane reaches a threshold potential (~–60 mV), a large population of voltage-gated Na+ channels (primarily Nav1.5, encoded by SCN5A) is activated, which results in a large inward influx of Na+ across the membrane into the myocyte. Na+ channels are functionally well suited to this task as they undergo rapid activation (activation time constant <0.5 ms) in response to membrane depolarization. Importantly, these channels also experience rapid voltage-dependent inactivation, which prevents reactivation until the membrane has returned to rest. The inward flux of Na+ ions carried by voltage-gated Na+ channels produces the initial rapid spike of the ventricular action potential (phase 0; see Figure 2-1).3 Depolarization of the cardiac membrane by rapidly activating voltage-gated Na+ channels activates higher threshold, more slowly activating voltage-gated Ca2+ channels (primarily CACNA1C-encoded Cav1.2 in the ventricle; see Figure 2-1).2 Ca2+ influx through voltage-gated Ca2+ channels serves two major purposes: (1) maintaining the action potential plateau (important for controlling heart rhythm), and (2) triggering Ca2+ release from internal stores for the purpose of triggering the mechanical contraction of the heart (excitation-contraction coupling).2 During excitation-contraction (EC) coupling, a small inward Ca2+ current across the plasma membrane is sensed by functional SR ryanodine receptor (RyR2 in the ventricle, encoded by RYR2) clusters, which subsequently release large quantities of Ca2+ from the internal SR stores into the cytosol, giving rise to a dramatic increase (order of magnitude) in intracellular Ca2+ (the Ca2+ transient).2 In this process, termed Ca2+-induced Ca2+ release, a small increase in local Ca2+ via Cav1.2 produces a relatively large release of SR Ca2+ (high gain function).
While voltage-gated Na+ and Ca2+ channels are responsible for myocyte depolarization and contraction, a host of plasma membrane–associated K+ channels regulate ventricular cardiomyocyte repolarization during phases 1, 2, and 3, as well as the rest potential.4 Specifically, the characteristic repolarization “notch” of phase 1 is modulated by the outward flux of K+ carried by the transient outward K+ current, Ito (primarily Kv4.2/Kv4.3 channels; see Figure 2-1). The duration of the action potential plateau (phase 2) is determined by a delicate balance between the inward Ca2+ current and the outward delayed rectifier K+ currents IKr and IKs (erg1/MiRP1 and KvLQT1/MinK channels encoded by KCNH2/KCNE2 and KCNQ1/KCNE1, respectively; see Figure 2-1).4 As the action potential proceeds, the Ca2+ current decreases because of deactivation as well as inactivation, and the K+ currents IKr and IKs increase, ultimately tilting the balance in favor of the late repolarization phase (phase 3; see Figure 2-1).4 The cell eventually returns to a resting potential maintained primarily by the time-independent inward rectifier current IK1 (see Figure 2-1). Other currents such as IKATP, while not central to the healthy control action potential, may have key roles in disease. Finally, the Na+-K+ adenotriphosphatase (ATPase) (which uses ATP to remove 3 Na+ from the cell and bring in 2 K+) is a key feature for generating and maintaining the myocyte electrochemical gradient.
Cell Membrane Architecture Defines Myocyte Local Electrical Activity
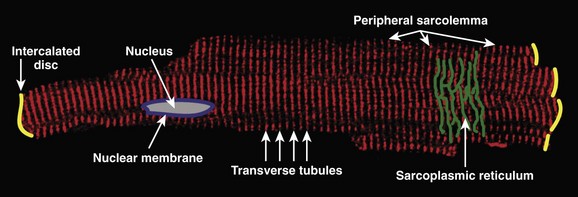
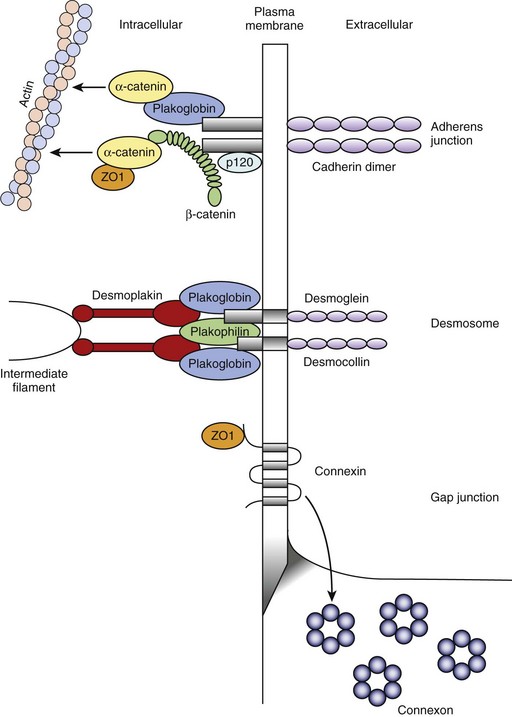
The ventricular cardiomyocyte plasma membrane, or sarcolemma, is divided into multiple and unique membrane structures (Figure 2-2). In addition to the external sarcolemma (resident proteins include the Na+-Ca2+ exchanger (NCX1) and plasma membrane Ca2+-ATPase [PMCA1]), the ventricular cardiomyocyte contains a large array of regularly spaced (~1.8 μm) plasma membrane invaginations, termed transverse tubules, or T-tubules. This membrane system, instrumental in myocyte EC coupling, evolved to facilitate coordinated EC coupling in the relatively large ventricular cardiomyocyte (system not present in smaller atrial and sinoatrial node cells). T-tubule–resident proteins include the L-type Ca2+ channel Cav1.2, the Na+-Ca2+ exchanger, and Na+-K+-ATPase.2 Finally, a highly specialized domain is present where the ventricular cardiomyocyte plasma membrane lies in close apposition to the plasma membrane of a neighboring cell. This complex membrane system, termed the intercalated disc, is required for myocyte cell-cell adhesion as well as intercellular action potential propagation and comprises three subdomains: (1) the gap junction, (2) the adherens junction, and (3) the desmosome (Figure 2-3).2 The gap junction comprises hundreds of hemi-channels (connexons) that span the lipid bilayer and allow electrical and metabolic coupling when docked with hemi-channels from a neighboring cell. At least four different connexin proteins (functional units of the connexon) with distinct biophysical properties are expressed throughout the heart. Gap junctions in ventricular tissue consist primarily of connexin43, which forms large conductance channels to allow rapid conduction. In contrast, gap junctions in the sinus node contain mostly connexin45, which forms lower conductance channels ideal for slow but safe conduction. The adherens junction is maintained by the function of a cadherin-catenin complex that provides a stabilizing link from the intercalated disc to the actin cytoskeleton (see Figure 2-3). Finally, the desmosome also supports cell adhesion through a complex, including plakoglobin (γ-catenin, also found in the adherens junction), desmoplakin, and plakophilin, that interacts with intermediate filaments (see Figure 2-3). Interestingly, defects in desmosomal proteins have been linked to cardiomyopathies and arrhythmias, including arrhythmogenic right ventricular cardiomyopathy (ARVC). In fact, loss of plakoglobin immunostaining in human heart biopsies has been recently developed into a diagnostic marker for Naxos disease, a cardiocutaneous syndrome characterized by wooly hair, palmoplantar keratoderma, and severe cardiomyopathy.5
In addition to the external plasma membrane, the cardiac myocyte (as well as many other excitable cells, including neurons and skeletal muscle) contains SR, the specialized endoplasmic reticulum that has key roles in the regulation of intracellular Ca2+.2 The cardiac SR is an extensive network of tubules linking key signaling networks, including the plasma membrane, nuclear envelope, nucleus, and mitochondria, to mediate a host of diverse functions. The pre-eminent role of the cardiac SR is to regulate myocyte EC coupling. Specifically, the vertebrate SR sequesters a large pool of releasable Ca2+ (1 mM inside SR vs. 100 nM in cytosol2) that serves as the primary source of Ca2+ for troponin-C (TnC) activation and muscle contraction (discussed in detail below).2 The majority of this Ca2+ is internally buffered by the Ca2+-binding protein calsequestrin, which forms a critical RyR2 regulatory complex with triadin and junctin. However, Ca2+ entry into the cell during the action potential plateau through voltage-gated Ca2+ channels activates SR ryanodine receptor Ca2+ channels. These RyR2 channels then rapidly release sequestered SR Ca2+ into the cytosol (see below) to signal contraction. During diastole, SR Ca2+-ATPase (SERCA2) and its regulatory protein phospholamban play central roles in the reuptake of released Ca2+ from the myocyte cytosol into the SR. Interestingly, inappropriate regulation of SR Ca2+ because of defects in either Ca2+ buffering (i.e., human calsequestrin-2 gene mutations) or Ca2+ release (human RyR2 gene mutations) has been linked with potentially fatal human arrhythmia (catecholaminergic polymorphic ventricular tachyarrhythmia). SR membrane–resident proteins also include inositol 1,4,5 trisphosphate (InsP3) receptors that have been linked to cardiac hypertrophy and arrhythmia.6
During the ventricular action potential, the rise in cytosolic Ca2+ via the SR membrane–associated RyR2 is rapidly translated into mechanical activity between the thick myosin filaments and the thin actin filaments through the regulatory functions of the troponin-tropomyosin complex.2 This complex consists of four subunits. Tropomyosin is a double-stranded α-helical molecule, which, under basal conditions (low Ca2+), covers myosin-binding sites along a span of seven actin monomers.2 Troponin T (TnT; tropomyosin-binding subunit) connects tropomyosin to the two remaining subunits TnC (Ca2+-binding) and troponin I (TnI; inhibitory subunit). The cardiac isoform of TnC has two high-affinity binding sites for Ca2+ or Mg2+ in the C-terminal domain and a low-affinity regulatory binding site that is Ca2+ specific in the N-terminal domain. During diastole, the C-terminal domain of TnI interacts with actin. During systole, Ca2+ binds to a low-affinity binding site in the TnC N-terminal domain, causing an increased affinity between this domain and the TnI N-terminal domain. As a result, the TnI-actin interaction is destabilized, which ultimately leads to a conformational change in the troponin-tropomyosin complex.2 Specifically, this complex is shifted and exposes myosin binding sites on actin, leading to “cross-bridge” formation between actin and myosin, force production, and cellular shortening.2 On removal of Ca2+ from the cytosol (primarily by the activities of SERCA2A and the plasma membrane Na+-Ca2+ exchanger), these molecular events are rapidly reversed, which results in cellular relaxation.2 Specifically, as cytosolic Ca2+ levels decrease, Ca2+ is removed from the TnC low-affinity binding site, causing TnI to dissociate from TnC and then reassociate with actin, effectively re-establishing the steric hindrance imposed by the troponin-tropomyosin complex.
As discussed in detail below, the dynamic range of cardiac excitation-mechanical coupling is, in part, regulated by phosphoregulation of key ion channels and transporters, which modulate intracellular Ca2+ in addition to altering the Ca2+ sensitivity of contractile proteins. For example, protein kinase A (PKA) phosphorylation of phospholamban at serine 16 relieves inhibition of phospholamban on SERCA2, thereby increasing SR Ca2+ uptake and promoting muscle relaxation.7 In addition to phosphorylating membrane proteins, PKA also phosphorylates contractile proteins to decrease their Ca2+ sensitivity, thereby promoting muscle relaxation. These modifications allow for increased cycle frequency elicited by exercise. For example, the N-terminal domain of cardiac TnI is phosphorylated by cyclic adenosine monophosphate (cAMP)-dependent PKA phosphorylation at serines 22 and 23. Phosphorylation of these residues desensitizes TnI to Ca2+-bound TnC and reduces the Ca2+ affinity of the Ca2+-specific regulatory site on TnC.8 Thus, these findings clearly illustrate the highly collaborative roles of structural, electrical, mechanical, and signaling proteins in the modulation of myocyte EC coupling and cardiac function.
Recent findings demonstrate key cellular roles for nuclear and mitochondrial membranes in the regulation of myocyte transcriptional pathways and in metabolism. The nuclear envelope is a complex structure comprising outer and inner nuclear membranes. The outer nuclear membrane is continuous with the SR, and the inner membrane contains a number of critical membrane proteins involved in nuclear assembly and gene transcription, such as lamins, which create a structural lattice for nuclear envelope integrity, and emerins, which bind directly to actin filaments. Mutations in lamin A/C and emerin have been linked to Emery-Dreifuss muscular dystrophy, a degenerative muscle disease featuring cardiac conduction defects. Human mutations in the nuclear lamina protein emerin (EMD), which are relevant to cardiac arrhythmia, have also been linked to familial atrial fibrillation and sinus node disease.9 Specifically, identified probands display a complex arrhythmia phenotype, including irregular, chaotic atrial rhythm and first-degree atrioventricular block.9 One proband displayed premature atrial complexes with rate variability (30 to 100 beats/min), and sinus arrest with junctional escape rhythm.9 Interestingly, the identified EMD mutation is hypothesized to affect the interaction between the emerin LEM domain and intranuclear binding proteins.9 Moreover, analysis of emerin localization in EMD mutation carriers revealed defects in nuclear emerin localization.9 These findings clearly demonstrate the unexpected link between cardiac atypical cellular architecture, in this case the nuclear lamina, and normal cellular excitability. In addition to having clear roles in orchestrating cellular structure and intermediate filament organization, the nuclear membrane also contains an autonomous system for Ca2+ signaling. InsP3 receptors located on both the inner and outer nuclear membranes allow Ca2+ release from the nuclear membrane lumen into the nucleoplasm and cytosol, respectively.10 In fact, work by Bers and colleagues demonstrated that Ca2+ in the nuclear membrane is tightly regulated by SR Ca2+, and this Ca2+ is central to cardiac excitation-transcription signaling via InsP3 receptor-dependent signaling.11
Cardiac mitochondria play an important role not only in energy production but also in Ca2+ homeostasis and apoptosis. Mitochondria occupy a large percentage of the cell volume (about 30%) and are concentrated near myofilaments, T-tubules, and the SR.12 Mitochondria comprise inner and outer membranes surrounding the mitochondrial matrix, where oxidative phosphorylation drives ATP production. A large potential gradient (ΔΨm about –180 mV) across the inner mitochondrial membrane, together with a proton gradient (ΔpH), is necessary for the conversion of adenosine diphosphate (ADP) to ATP. Respiration is regulated by many factors, including ADP and Ca2+, which activate key enzymes in the tricarboxylic acid (TCA) cycle. Highly selective Ca2+ uniporters expressed in the inner mitochondrial membrane use the electrical gradient across the inner mitochondrial membrane to move Ca2+ from the myoplasm into the mitochondria. The proximity of mitochondria to the Ca2+ channels at T-tubules and to the Ca2+ release sites on the SR create a local Ca2+ domain that provides mitochondria with access to an important resource for respiration and enables mitochondria to serve as an important buffer of intracellular Ca2+. Interestingly, disruption of the normal mitochondrial arrangement within the cell has been linked to mitochondrial dysfunction, apoptosis, and arrhythmias in a murine model of desmin-related cardiomyopathy. The mitochondrial Na+-Ca2+ exchanger helps maintain mitochondrial Ca2+ homeostasis, and the Na+-H+ exchanger and the Na+-K+-ATPase use the proton gradient and ATP, respectively, for maintaining mitochondrial Na+ homeostasis. Ion homeostasis in the myoplasm and in the mitochondrial matrix are coupled such that dysregulation of homeostasis in the myoplasm may alter mitochondrial energetics. Thus, myoplasmic Na+ accumulation in the setting of heart failure may accelerate Ca2+ removal from the mitochondrial matrix via the Na+-Ca2+ exchanger, leading to decreased mitochondrial Ca2+, decreased NADH production via the TCA cycle, and decreased ATP production.13 Conversely, myoplasmic Ca2+ overload (e.g., during myocardial ischemia) may lead to the accumulation of mitochondrial Ca2+ and the opening of the mitochondrial permeability transition pore, a large nonspecific conductance in the inner mitochondrial membrane that discharges the mitochondrial membrane potential, which leads to cell death.13
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree