Chapter 24 Electrophysiological Evaluation of Supraventricular Tachycardia
Paroxysmal supraventricular tachycardia (PSVT) is a common condition that affects a wide range of age groups. The clinical syndrome of PSVT and its presentation and management are discussed in detail in Chapter 41. Electrophysiologic study (EPS) of PSVT is routinely performed in clinical laboratories as a component of the diagnostic and therapeutic approach to management of this condition. The clinical presentation of a patient with PSVT includes a variety of tachyarrhythmias, as detailed in Chapter 41 and summarized in Table 24-1. The purpose of EPS is to differentiate the mechanisms of PSVT in an individual patient and help guide appropriate therapy for patient management. These therapeutic approaches can include catheter ablation procedures (see Chapter 93), drug therapy (see Chapters 79 and 80) and, rarely, device therapy (see Chapter 41). For special consideration of drug therapy or ablation in pediatric or pregnant patients, see Chapters 72, 74, and 75, respectively. The focus of this chapter is to delineate the diagnostic information elicited at clinical EPS in two common forms of PSVT—namely, atrioventricular (AV) nodal reentrant tachycardia (AVNRT) and AV reentrant tachycardia (AVRT). EPS of atrial tachycardia (AT) is examined in Chapter 29.
Table 24-1 Paroxysmal Supraventricular Tachycardias with Narrow and Wide QRS Complexes
| SINUS NODE DISORDERS |
| AV NODAL RE-ENTRANT TACHYCARDIAS |
| RE-ENTRANT AND ECTOPIC ATRIAL TACHYCARDIAS |
| PRE-EXCITATION SYNDROME: WOLFF-PARKINSON-WHITE SYNDROME |
| OTHER PRE-EXCITATION SYNDROMES: MAHAIM CONDUCTION |
Atrial tachycardia, AV nodal re-entry, or atrial fibrillation with nodoventricular or nodofascicular bystander conduction |
| AUTOMATIC AV JUNCTIONAL TACHYCARDIAS |
AV, Atrioventricular.
Diagnostic Approach to the Patient with Supraventricular Tachycardia
The initial diagnostic approach to the patient with PSVT, as mentioned in Chapter 41, is documentation of the arrhythmia by electrocardiogram (ECG).
Atrioventricular Re-entrant Tachycardia and Atrioventricular Node Re-entrant Tachycardia
The methods of catheter placement and programmed electrical stimulation are discussed in detail in Chapter 20 and are not revisited here in detail. In brief, multipolar electrode catheters are placed in the right atrium, His bundle region, coronary sinus, and right ventricle. Recordings are obtained from these regions as well as the right and left AV ring for bypass tract mapping or more detailed septal pathway localization. Programmed atrial stimulation is usually performed from the high right atrium, coronary sinus, right ventricular apex, and the atrial or ventricular insertion site of a bypass tract as needed. In some instances, alternate pacing sites can include the left atrium, right ventricular outflow tract, right ventricular septum, or left ventricle. For the study of propagation and induction of tachycardia, the extrastimulus technique is widely used, although burst pacing is an alternative. These techniques are discussed in Chapter 20. Facilitiation of induction may require the administration of pharmacologic agents such as isoproterenol or atropine (see Chapter 72). Other pharmacologic agents such as adenosine may be used for diagnostic purposes to evaluate the presence of accessory pathway conduction or termination of PSVT involving the AV node (see Chapter 72).
Most SVTs are caused by a re-entrant mechanism and may be induced in the laboratory by using programmed electrical stimulation. In A-V junctional tachycardias, electrophysiological study permits induction of tachycardia in more than 90% of patients with AVRT or AVNRT. In patients with AVNRT, premature atrial stimulation can demonstrate dual AV nodal conduction and induce the tachycardia to determine its mechanism. The arrhythmias associated with WPW syndrome include reciprocating or circus movement tachycardias and atrial arrhythmias. In some instances of AVNRT, concomitant pre-excited QRS complexes may exist because of passive conduction over an accessory pathway that may serve as a passive bystander. Tachycardias related to Mahaim fibers have a particular electrocardiographic presentation with LBBB and left-axis deviation. The ECG in sinus rhythm shows the features of WPW syndrome (Figure 24-1). The electrophysiological study often demonstrates decremental conduction over the accessory pathway.
Atrioventricular Nodal Re-Entrant Tachycardia
Dual Atrioventricular Nodal Pathway
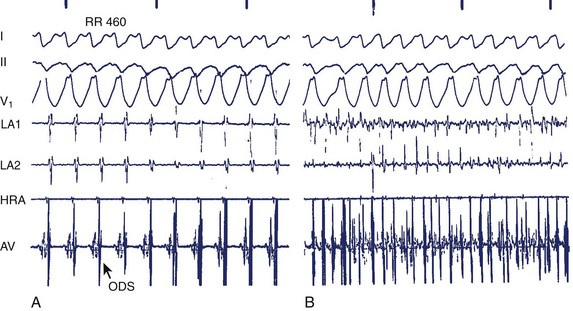
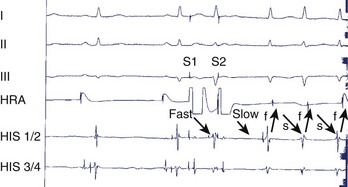
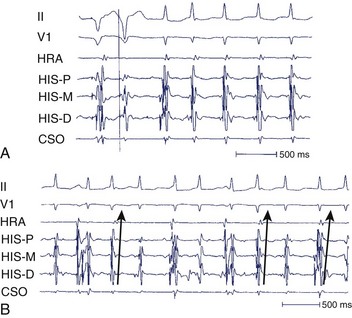
During electrophysiological evaluation, typical AVNRT manifests antegrade conduction via a “slow” pathway and retrograde conduction via a “fast” pathway.1–10 The electrophysiological characteristic is the presence of dual AV nodal pathway physiology demonstrated by a discontinuous AV node functional curve. Discontinuous AV nodal conduction is defined as a sudden increment of 50 ms or greater in the A-H or H-A interval (“jump”), with a decrement in prematurity of the extrastimulus by 10 to 20 ms. In some patients, a jump (>50 ms) of any consecutive A-H intervals during incremental atrial pacing is found, which might be a manifestation of dual AV nodal pathways. Typically, the jump phenomenon is followed by induction of a slow-fast AVNRT (Figure 24-2). During tachycardia in typical slow-fast AVNRT, a long A-H interval with a short V-A interval can be documented (Figure 24-3). When performing endocardial mapping, the earliest atrial activation during tachycardia can be detected at the slow pathway area around the coronary sinus ostium. In contrast, atypical AVNRT has antegrade conduction through a “fast” or “slow” pathway and retrograde conduction through a “slow” pathway.2,3
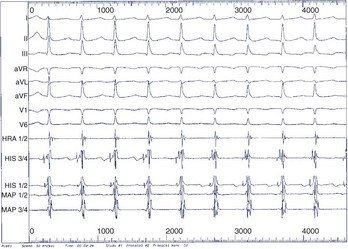
FIGURE 24-3 Typical slow-fast atrioventricular nodal re-entrant tachycardia with a short V-A interval.
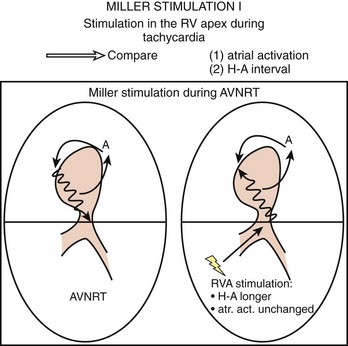
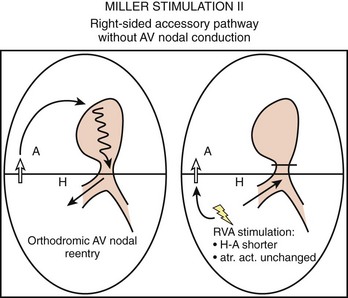
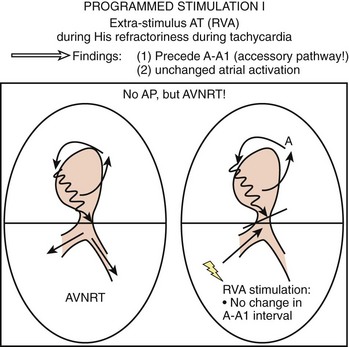
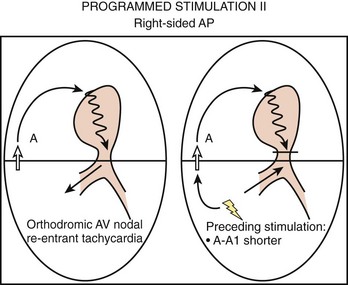
To differentiate AVNRT from AVRT, the following maneuvers can be used4–6:
Two important concepts of dual AV nodal pathways have been further clarified by provocative pharmacologic testing and catheter ablation in patients with AVNRT. One major question has been whether dual AV nodal pathways are fully intranodal and caused by longitudinal dissociation of AV nodal tissue or extranodal, involving separate atrial inputs into the AV node. From clinical studies of slow pathway potentials, LH (low followed by high) frequency potentials are observed during asynchronous activation of muscle bundles above and below the coronary sinus orifice. HL (high followed by low) frequency potentials are caused by asynchronous activation of atrial cells and a band of nodal-type cells that may represent the substrate of the slow pathway.7–10 Thus the slow and fast pathways are likely to be atrionodal approaches or connections rather than discrete intranodal pathways. The results of catheter ablation indicate that the fast and slow pathways have their origins outside the limits of the compact AV node and that the tissues targeted during successful ablation are composed of ordinary working atrial myocardium surrounding the AV node itself.11–14 Furthermore, AV or VA conduction block during AVNRT favors the concept that atrial and ventricular tissues are not involved in the maintenance of this tachycardia (Figures 24-8 and 24-9).15,16
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree