Mortality in patients with chronic heart failure (CHF) is high and associated with body mass. However, the best method of assessing nutritional status in patients with CHF is not clear. We sought to demonstrate the prognostic use of a nutritional risk index (NRI) in ambulatory patients with CHF. Consecutive patients attending their first quarterly review appointment in the HF clinic were recruited. All patients had systolic left ventricular (LV) dysfunction. An NRI was calculated as: (1.5 × serum albumin [grams per liter]) + (current body weight/ideal weight). Patients were followed up every 4 months. Of the 538 patients enrolled in the study 75% were men. The patients’ age was 71 ± 10 years (mean ± SD) and total median follow-up in survivors was 68 months (interquartile range 54 to 74). New York Heart Association classes II and III accounted for 60% and 27%, respectively, with 80% having moderate LV impairment or worse. Based on the NRI 23% of patients were at risk of malnutrition. Severely malnourished patients were older. There was no relation between NRI and LV function. The NRI was a univariable predictor of mortality (chi-square 25, p <0.001) and was an independent predictor of outcome in multivariable analysis (chi-square 12, p <0.001). In conclusion, the NRI is useful as a prognostic marker in patients with CHF in an outpatient setting. NRI might be of use as a surrogate marker for nutritional status in trials of dietary supplementation in CHF.
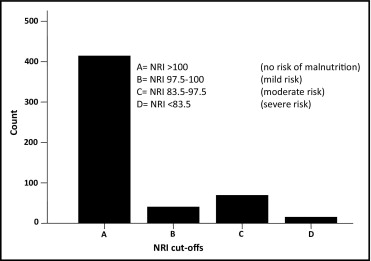
Chronic heart failure (CHF) is commonly associated with weight loss, and once cardiac cachexia develops, the prognosis worsens significantly. Many factors contribute to weight loss in CHF. Although metabolic rate at rest is increased in many patients, their total daily energy expenditure is lower than in matched controls in some reports. Symptoms of breathlessness and fatigue lead to a limitation in the amount of activity performed and result in loss of muscle bulk. There is a shift toward a catabolic state owing to an activation of initially protective neurohormonal pathways. Patients with CHF also have decreased appetites and can develop malabsorption and enteral protein loss. A full assessment of the nutritional status of a subject includes a full medical history, physical examination, blood tests such as serum protein measurements, and an assessment of immunocompetence. A way of simplifying nutritional assessment is to use a clinical score method such as the Subjective Global Assessment. The Subjective Global Assessment, however, has limited success in patients with CHF, particularly in women. The Veterans’ Affairs Total Parenteral Nutrition Cooperative Study Group identified patients at risk of postsurgical complications and developed a nutritional risk index (NRI). It has been used to stratify the risk of developing complications in nonsurgical hospitalized patients. The NRI relies on objective measurements and is calculated as (1.5 × serum albumin [grams per liter]) + (current body weight/usual body weight). An NRI ≥100 indicates no evidence of malnourishment, 97.5 to 100 indicates mild malnourishment, 83.5 to 97.5 indicate moderate malnourishment, and <83.5 indicate severe malnourishment. We sought to assess the prognostic use of NRI in ambulatory patients with CHF.
Methods
We report on a cohort of consecutive patients recruited from a community CHF clinic attending a 4-month review. Patients were recruited retrospectively from June 2002 through September 2008 and were included if they had a diagnosis of CHF secondary to impairment of left ventricular (LV) systolic function. All patients had a full medical history, physical examination, echocardiogram, and routine blood tests at the time of presentation. Serum albumin levels were measured by photometry using a DxC 800 analyzer (Beckman Coulter, High Wycombe, United Kingdom). Echocardiography was performed by an experienced technician using a Vivid 5 scanner (GE, Fairfield, Connecticut) with a 2.5-MHz phased-array transducer. LV ejection fraction was calculated using the Simpson method where possible (65% of all patients), and LV systolic function was estimated in all patients visually on a scale of mild, moderate, and severe impairment. Body weight was recorded on Tanita (Amsterdam, The Netherlands) scales with the patients in their normal clothes and without their shoes.
Patients were followed every 4 months for the first year and annually thereafter unless more frequent follow-up was deemed necessary by the physician. The clinic strategy was to achieve optimal treatment. The status of all the subjects was known up to and including the censor date of November 25, 2009. Although patients were recruited at their initial 4-month appointment, they had not necessarily been titrated up to final medical therapy. We recruited patients at their 4-month visit to minimize the effects of changes in medication instituted at baseline.
The NRI was calculated for all patients as: (1.5 × serum albumin [grams per liter]) + (current body weight/ideal body weight [IBW]). IBW was calculated using the Devine formula for men (IBW [kilograms] = 50 kg +2.3 kg for each inch >5 feet) and the Robinson formula for women (IBW [kilograms] = 48.67 kg +1.65 kg for each inch >5 feet). IBW was used instead of usual body weight because it is less subjective.
Data analysis was performed using SPSS 15.0 (SPSS, Inc., Chicago, Illinois). Discrete variables are presented as frequency count and percentage, and continuous variables are expressed as mean ± SD when normally distributed or as median (interquartile range) if not. Chi-square test, Student’s t test, and Mann–Whitney U test were used to compare proportions and means or medians. Pearson correlation coefficients were calculated between the NRI and other variables.
Cox proportional hazard models and Kaplan–Meier curves were constructed to explore the relation between variables and outcome. Variables were then tested in a backward stepwise multiple Cox regression model to determine independent predictors of death. Variables that were used in the calculation of NRI were not included in multivariable models. NRI was analyzed as a continuous variable. A p value <0.05 was considered statistically significant. Only variables with a p value <0.05 in the univariable model were included in multivariable analysis.
Results
Table 1 presents a summary of the characteristics of the total cohort and those of patients divided into quartiles of NRI. Median follow-up in survivors was 68 months (interquartile range 54 to 74). Cause of HF was ischemic heart disease in 75% of cases. The other 25% was due to hypertension, diabetes, valvular disease, and idiopathy. Patients in the first quartile of NRI were at greatest risk of being malnourished. When comparing quartiles of NRI, those at greatest risk of malnourishment were older, but there was no significant difference in LV function. Fewer of the malnourished patients had diabetes or hypertension. Use of angiotensin-converting enzyme inhibitors and β blockers was similar across quartiles of NRI. As risk of malnourishment increased, fewer patients were on aldosterone antagonists. Aspirin and statin use increased form the first to the fourth quartile.
| Total Cohort (n = 538) | NRI (quartiles) | p Value | ||||
|---|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | |||
| (n = 137) | (n = 133) | (n = 135) | (n = 133) | |||
| Variable | ||||||
| Age (years) | 71 ± 9.9 | 75 ± 9.0 | 72 ± 9.6 | 71 ± 9.7 | 68 ± 11 | <0.001 |
| Men | 76% | 75% | 82% | 73% | 73% | 0.33 |
| Nutritional risk index | 109 ± 11.4 | 94 ± 6.7 | 105 ± 2.1 | 112 ± 2.2 | 124 ± 7.3 | |
| Body mass index (kg/m 2 ) | 28 ± 5.4 | 23 ± 2.8 | 26 ± 2.5 | 28 ± 2.5 | 34 ± 5.1 | <0.001 |
| New York Heart Association class | 0.22 | |||||
| I | 10% | 11% | 15% | 9% | 9% | |
| II | 60% | 65% | 57% | 63% | 53% | |
| III | 28% | 23% | 26% | 26% | 35% | |
| IV | 2% | 1% | 2% | 2% | 3% | |
| Left ventricular dysfunction | 0.68 | |||||
| Mild | 20% | 18% | 19% | 22% | 22% | |
| Moderate | 56% | 53% | 60% | 55% | 57% | |
| Severe | 24% | 29% | 21% | 23% | 21% | |
| Ischemic heart disease | 75% | 70% | 77% | 75% | 77% | 0.1 |
| Diabetes | 26% | 17% | 20% | 29% | 39% | <0.001 |
| Hypertension | 43% | 37% | 30% | 47% | 57% | 0.001 |
| Sinus rhythm | 74% | 70% | 77% | 72% | 78% | 0.59 |
| Medications | ||||||
| Aldosterone antagonist | 26% | 15% | 24% | 32% | 31% | 0.01 |
| Aspirin | 42% | 42% | 33% | 40% | 53% | 0.02 |
| Statin | 49% | 38% | 52% | 50% | 58% | 0.04 |
| Warfarin | 28% | 27% | 33% | 31% | 21% | 0.11 |
| Loop diuretic | 77% | 72% | 81% | 80% | 76% | 0.39 |
| Digoxin | 16% | 16% | 18% | 18% | 13% | 0.43 |
| Thiazide | 1.7% | 1.4% | 1.5% | 1.4% | 2.2% | 0.63 |
| Amiodarone | 9.7% | 8.9% | 11% | 12% | 6.7% | 0.69 |
| Angiotensin-converting enzyme inhibitor or angiotensin receptor blocker | 84.4 | 79.8 | 87.4 | 88.8 | 81.5 | 0.44 |
| β Blocker | 78% | 75% | 80% | 78% | 77% | 0.78 |
| Laboratory variables | ||||||
| White blood cell count (×10 9 /L) | 7.3 ± 2.4 | 7.1 ± 2.0 | 7.3 ± 2.3 | 7.2 ± 2.7 | 7.7 ± 2.3 | 0.03 |
| Hemoglobin (g/dl) | 13.1 ± 1.6 | 12.7 ± 1.4 | 13.1 ± 1.6 | 13.2 ± 1.3 | 13.5 ± 1.9 | 0.01 |
| Platelets (×10 9 ) | 223 ± 64 | 230 ± 68 | 213 ± 64 | 216 ± 55 | 234 ± 63 | 0.22 |
| Sodium (mmol/L) | 139 ± 3.0 | 139 ± 3.3 | 139 ± 3.0 | 140 ± 2.9 | 140 ± 3.0 | 0.02 |
| Potassium (mmol/L) | 4.5 ± 0.5 | 4.5 ± 0.5 | 4.5 ± 0.5 | 4.5 ± 0.5 | 4.5 ± 0.5 | 0.69 |
| Creatinine (μmol/L) | 129 ± 52 | 135 ± 54 | 128 ± 53 | 132 ± 52 | 123 ± 48 | 0.25 |
| Urea (mmol/L) | 9.3 ± 5.2 | 9.9 ± 5.2 | 8.8 ± 5.1 | 9.7 ± 5.1 | 8.6 ± 5.4 | 0.30 |
| Albumin (g/L) | 38 ± 3.3 | 35 ± 3.4 | 38 ± 2.5 | 39 ± 2.5 | 39 ± 3.2 | <0.001 |
Using the NRI investigators’ data to define risk level cutoffs for malnutrition, 23% of our cohort was malnourished and 2.8% had severe malnourishment. Figure 1 shows the distribution of patients by risk of malnutrition. Table 2 presents a comparison of subject characteristics between those at risk of malnutrition and those not at risk.
| At Risk of Malnutrition (NRI <100) | Not at Risk of Malnutrition (NRI ≥100) | p Value | |
|---|---|---|---|
| (n = 124) | (n = 414) | ||
| Variables | |||
| Age (years) | 75 ± 8 | 71 ± 10 | <0.001 |
| Men | 75% | 76% | 0.80 |
| Body mass index (kg/m 2 ) | 23 ± 3 | 29 ± 5 | <0.001 |
| New York Heart Association class | 0.82 | ||
| I | 12% | 11% | |
| II | 61% | 59% | |
| III | 25% | 28% | |
| IV | 2% | 2% | |
| Left ventricular dysfunction | 0.09 | ||
| Mild | 17% | 21% | |
| Moderate | 53% | 57% | |
| Severe | 30% | 22% | |
| Ischemic heart disease | 68% | 77% | 0.08 |
| Diabetes | 18% | 28% | 0.03 |
| Hypertension | 41% | 43% | 0.71 |
| Sinus rhythm | 74% | 80% | 0.18 |
| Medication | |||
| Aldosterone antagonist | 12% | 29% | <0.001 |
| Aspirin | 40% | 42% | 0.75 |
| Statin | 38% | 52% | 0.01 |
| Warfarin | 28% | 28% | 0.96 |
| Loop diuretic | 68% | 80% | 0.01 |
| Digoxin | 17% | 16% | 0.87 |
| Thiazide | 1.7% | 1.8% | 0.94 |
| Amiodarone | 9.6% | 9.6% | 0.99 |
| Angiotensin-converting enzyme inhibitor or angiotensin receptor blocker | 79% | 86% | 0.08 |
| β Blocker | 75% | 78% | 0.40 |
| Laboratory variables | |||
| White blood cell count (×10 9 /L) | 7.2 ± 2.1 | 7.3 ± 2.4 | 0.68 |
| Hemoglobin (g/dl) | 12.7 ± 1.5 | 13.2 ± 1.6 | 0.01 |
| Platelets (×10 9 ) | 234 ± 74 | 220 ± 61 | 0.06 |
| Sodium (mmol/L) | 139 ± 3 | 139 ± 3 | 0.02 |
| Potassium (mmol/L) | 4.5 ± 0.5 | 4.5 ± 0.5 | 0.53 |
| Creatinine (μmol/L) | 132 ± 57 | 129 ± 51 | 0.51 |
| Urea (mmol/L) | 9.7 ± 5.4 | 9.14 ± 5.1 | 0.28 |
A correlation matrix for variables in relation to NRI is presented in Table 3 . Variables most strongly correlated with NRI were body mass index (BMI), hemoglobin, and age. The older the subject and the lower the hemoglobin, the more likely subjects were to be malnourished. Lower NRI scores were also associated with lower sodium levels. There was no significant relation between NRI and creatinine or urea. There was no relation between NRI and level of LV dysfunction. A plot of NRI against severity of LV function is shown in Figure 2 .
| Variable | NRI Correlation Coefficient | p Value |
|---|---|---|
| Body mass index (kg/m 2 ) | 0.87 | <0.001 |
| Hemoglobin (g/dl) | 0.19 | <0.001 |
| Age (years) | −0.24 | <0.001 |
| White blood cell count (×10 9 ) | 0.11 | 0.03 |
| Sodium (mmol/L) | 0.08 | 0.07 |
| Platelets (×10 9 ) | 0.06 | 0.23 |
| Urea (mmol/L) | −0.48 | 0.26 |
| Potassium (mmol/L) | −0.03 | 0.49 |
| Creatinine (μmol/L) | −0.21 | 0.63 |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


