Chapter 21 Pacemakers and Implantable Cardioverter-Defibrillators Essentials for Clinicians
Please go to expertconsult.com for supplemental chapter material.
Pacemakers: Definitions and Types
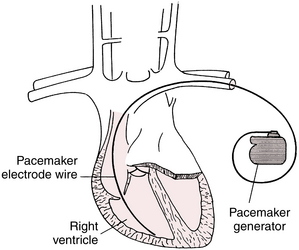
A pacemaker consists of two major components: (1) a pulse generator (battery and microcomputer) and (2) one or more electrodes (also called leads). The electrodes can be attached to the skin (in the case of emergency transcutaneous pacing), but more often are attached directly to the inside of the heart (Fig. 21-1).
Permanent pacemakers have both the generator and electrode(s), also called leads, implanted inside the body (see Fig. 21-1). Electronic pacemakers are used for three major purposes:
• They can supplant impaired atrial impulse formation in severe sinus node dysfunction.
• They can supplant impaired AV conduction in heart block syndromes, thereby restoring normal AV timing (synchrony∗).
• They can compensate for left bundle branch block (LBBB) conduction abnormalities, especially with heart failure, by providing synchronization∗ of right and left ventricular contraction. This use is called resynchronization therapy or biventricular pacing.
All contemporary pacemakers are capable of sensing intrinsic electrical activity of the heart and are externally programmable (adjustable) using special computer devices provided by the manufacturers. Pacemakers are usually set to operate in an on-demand mode, providing electronic pacing support only when the patient’s own electrical system fails to generate impulses in a timely fashion. Modern pacemaker batteries last on average between about 8 and 12 years, depending on usage.
Single- and Dual-Chamber Pacemakers
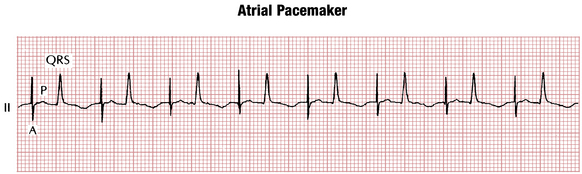
Single-lead (or single-chamber) pacemakers (see Fig. 21-1), as their name indicates, are used to stimulate only one chamber (right atrium or right ventricle). Atrial single-lead pacemakers (with the lead positioned in the right atrium) can be used to treat isolated sinus node dysfunction with normal AV conduction (Fig. 21-2). In the United States, single-lead atrial pacemakers are rarely used. Even patients with isolated sinus node dysfunction usually receive dual-chamber devices because AV conduction abnormalities often develop later as the patient ages.
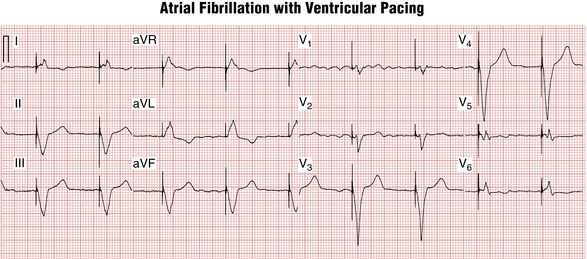
Ventricular single-lead pacemakers (with the lead positioned in the right ventricle) are primarily used to generate the heartbeat in patients with chronic atrial fibrillation with an excessively slow ventricular response. The atrial fibrillation precludes effective atrial stimulation so that there is no reason to insert an atrial lead (Fig. 21-3).
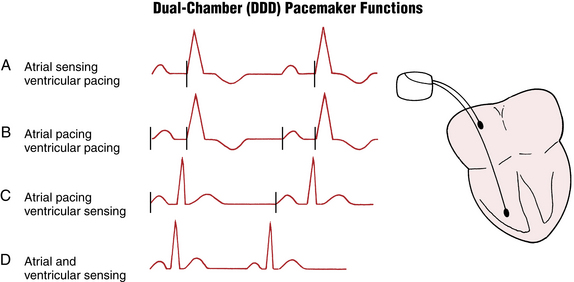
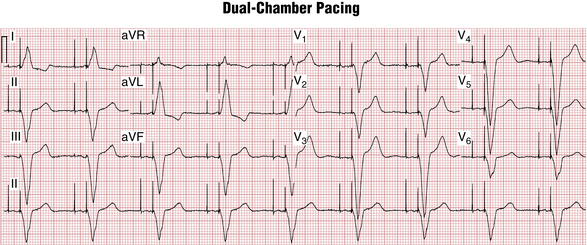
In dual-chamber pacemakers, electrodes are inserted into both the right atrium and right ventricle (Figs. 21-4 and 21-5). The circuitry is designed to allow for a physiologic delay (normal synchrony) between atrial and ventricular stimulation. This AV delay (interval between the atrial and ventricular pacemaker spikes) is analogous to the PR interval under physiologic conditions.
ECG Morphology of Paced Beats
A paced P wave demonstrates a pacing spike followed by a P wave (see Fig. 21-2).
A paced QRS beat also starts with a pacing spike, followed by a wide QRS complex (see Figs. 21-3 and 21-6). The wide QRS is due to the fact that activation of the ventricles starts at the tip of the lead and spreads to the other ventricle through slowly conducting myocardium, similar to what occurs with ventricular premature beats (VPBs) or ventricular escape beats. The QRS morphology depends on the lead (electrode) position. The most commonly used ventricular electrode site is the right ventricular apex. Pacing at this location produces a wide QRS (usually resembling an LBBB pattern; see Chapter 7) with a leftward axis (QRS deflections are predominantly negative in leads II, III, and aVF and positive in leads I and aVL).
As with VPBs, the T waves in paced beats normally are discordant—directed opposite to the main QRS direction (see Figs. 21-3 and 21-5). Concordant T wave (i.e., pointing in the same direction as the paced QRS) during ventricular pacing may indicate acute myocardial ischemia (see following discussion).
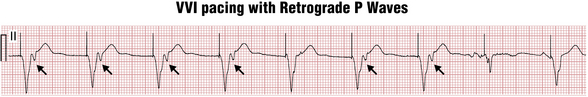
Ventricular paced beats, similar to VPBs, can also sometimes conduct in a retrograde manner to the atria, producing near simultaneous atrial and ventricular depolarization and contraction (Fig. 21-6). When this occurs repeatedly, atrial contraction against the closed AV valves produces recurrent, sudden increases in jugular (and pulmonary) vein pressures, which may be seen as “cannon” A waves in the neck examination. Of note for clinicians, these abrupt pressure changes, in turn, may activate a vagal reflex and cause severe symptoms (palpitations, pulsation in the neck, dizziness, and blood pressure drop), often referred to as the pacemaker syndrome. Therefore, patients in sinus rhythm with AV block are usually implanted with dual-chamber pacemakers so that ventricular pacing will occur after atrial pacing, maintaining physiologic AV timing (synchrony).
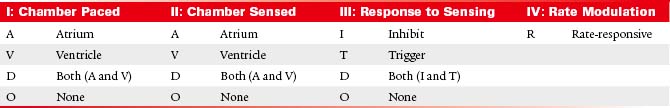
Electronic Pacemaker Programming: Shorthand Code
Historically, pacemaker programming has been described by a standard three- or four-letter code, usually followed by a number indicating the lower rate limit. Although many new pacing enhancements have been introduced since the inception of this code, it is still widely used (Table 21-1).
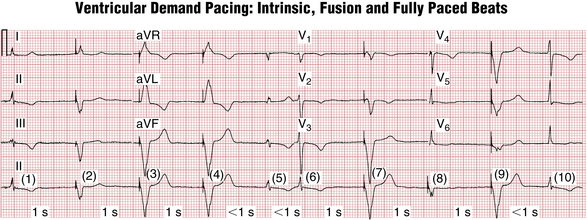
Single-Chamber Pacemaker Programming
As noted, modern pacemakers are programmed in the on-demand mode providing pacing support only when needed. In the case of a single-chamber pacemaker this function is accomplished by specifying the lower rate limit (for example 60 beats/min). The pacemaker constantly monitors the patient’s heart rate in the implanted chamber on a beat to beat basis. Any time the rate drops below the lower rate limit (in the case of 60/min, the critical pause after a spontaneous QRS complex will be >1 sec), the pacemaker will deliver a pacing stimulus (Fig. 21-7). This corresponds to the code: VVI 60.