Procedural outcomes for transcatheter aortic valve implantation (TAVI) are well described. However, limited information exists regarding patient screening and selection. Thus, the purpose of the study was to review consecutive patients referred for TAVI from an inclusive-defined population. The Mazankowski Alberta Heart Institute TAVI program has maintained a prospective database on all referred patients. Patients are reviewed in outpatient clinic attended by a nurse, cardiologist, cardiac surgeon, and administrative assistant. After workup is complete, a TAVI Heart Team conference occurs to accept or reject each patient. Since November 2009, 276 patients (145 men and 131 women) have been referred with a steady increase in the number of referrals annually. Mean age was 82.2 years (men 81.6 and women 82.8), with 13% aged <70 years. Mean EuroSCORE was 13.8 and mean STS score was 5.7. Of the referred patients, 34% received TAVI, 17% were rejected, 12% underwent open AVR, 10% refused TAVI, and 27% are currently being assessed or followed. There were no differences in the mean EuroSCORE (13.4 vs 14.3; p = 0.64) or STS scores (5.2 vs 6.4; p = 0.13) of those accepted for TAVI versus those who were not. In conclusion, a team-based approach to assess this complex patient population is essential to ensure efficient and comprehensive evaluation, in turn determining appropriate care allocation. With expansion of clinical experience and the evidence supporting TAVI, the Heart Teams defined to assess this patient population will be burdened with increased clinical commitment and require appropriate support.
The indications for aortic valve replacement (AVR) have been well established and, overall, this procedure can be performed with a very low (2.6%) risk of mortality. However, there are certain patients for whom surgical AVR is associated with high or prohibitive risk of morbidity and mortality. The introduction of transcatheter aortic valve implantation (TAVI) has provided an important treatment option for these high-risk patients. The Placement of AoRTic TraNscathetER Valve trial cohorts A and B have demonstrated that TAVI plays a key role in the management of patients with aortic stenosis who are considered to be at high or prohibitive surgical risk. With the publication of the aforementioned trials, and large registries in Europe, new challenges have arisen: namely, determining who is most appropriately managed with surgical AVR, with TAVI, and who is not a candidate for either intervention. Although procedural outcomes are well described, limited information exists regarding patient screening and selection. Thus, the purpose of the study was to review the characteristics and outcomes of consecutive patients referred for TAVI within a defined health-care region where all referrals are processed through a single TAVI program.
Methods
The Mazankowski Alberta Heart Institute is a quaternary care hospital that serves a population of 1.7 million people. It is the only cardiac surgery site in this defined health-care region. The Mazankowski Alberta Heart Institute TAVI program acts as a regional program and serves all tertiary care hospitals and cardiology groups within this region. Accordingly, all patients with aortic stenosis considered eligible for AVR are referred to this institution. Since the formal introduction of the Mazankowski Alberta Heart Institute TAVI program in November 2009, we have prospectively maintained a consecutive patient database.
Patients are reviewed in weekly outpatient clinic attended by a registered nurse, cardiologist, cardiac surgeon, and administrative assistant. During the initial visit, all patients received a transthoracic echocardiography, reviewed by a dedicated echocardiographer associated with the program (MS), to confirm severe aortic stenosis, annulus dimension, aortic valve calcification and anatomy, and ventricular function. A second surgical opinion is also critical for all potential candidates. Extensive amount of time is spent assessing overall functional status, current quality of life, and frailty to determine the appropriateness of TAVI. These assessments are aided by the use of the Minnesota Living with Heart Failure Questionnaire and the EQ-5D quality of life scale.
If on completion of the clinical assessment the patient appears to be an appropriate candidate for TAVI, additional investigations including cardiac catheterization are performed to assess coronary, aortic root, and iliofemoral anatomy. Computed tomographic scans are arranged if supplementary data are required. Once all data are collected, a TAVI Heart Team conference occurs to determine final candidacy. This team consists of both cardiologists and cardiac surgeons.
Continuous data are expressed as mean ± SD or as median when data are skewed and comparisons are made using Student t test. Categorical data are expressed as frequencies and percentages, with comparisons between categorical variables made using chi-square tests or Fisher’s exact test where appropriate. All analyses were performed using SPSS (version 20, IBM Software, Armonk, New York).
Results
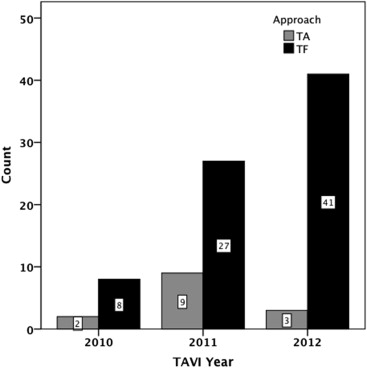
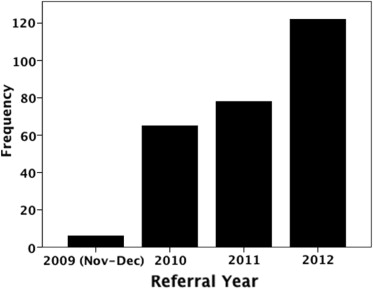
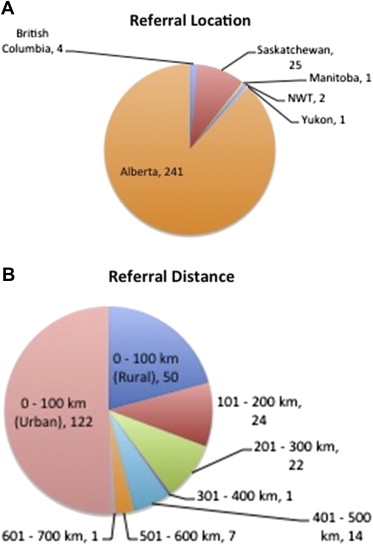
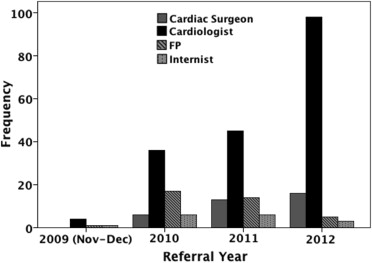
In total, 276 patients (145 men and 131 women) have been referred with a steady increase in the number of referrals in each year ( Figure 1 ). The mean age of those referred was 82.2 years (men 81.6 and women 82.8), with 13% aged <70 years, 20.7% aged 71 to 80 years, 51.1% aged 81 to 90 years, and 15.6% aged 91 to 100 years. Most referrals came from the province of Alberta (n = 241), with the remainder coming from adjacent provinces ( Figure 2 ). Travel distance for assessment is substantial with 37.2% of patients traveling >100 km and 28.1% patients traveling >200 km ( Figure 2 ). Most referrals came from cardiologists (n = 183), with the remainder coming from cardiac surgeons (n = 35), internists (n = 16), and family practitioners (n = 37). During the duration of the program’s 3 complete years, the referrals from cardiac surgeons have increased slightly (9.2% vs 13.1%). However, referrals from internists (9.2% vs 2.5%) and family physicians (26.2% vs 4.1%) decreased substantially once our referral process was refined to require review of potential candidates by a cardiologist (55.4% vs 80.3%) in advance of referral to the TAVI clinic ( Figure 3 ).
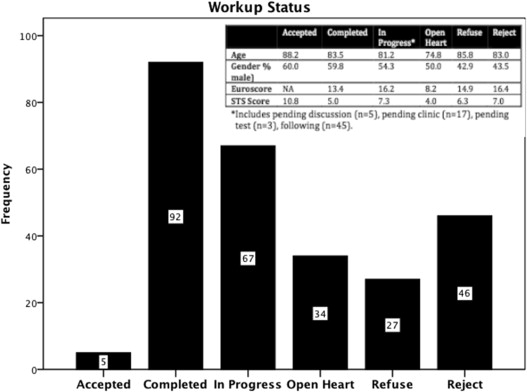
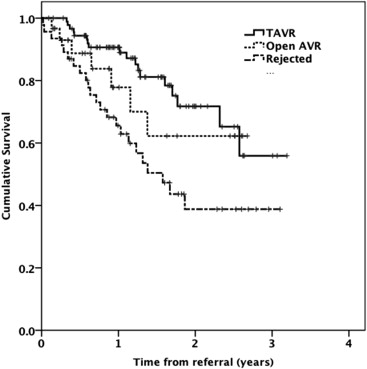
The outcomes of the screening program and the EuroSCORE and STS score data are summarized in Figure 4 . Overall, 92 patients have received TAVI, with the remainder in various states of workup or have had decisions made about their therapy. Mean EuroSCORE was 13.8 and mean STS score was 5.7. There were no significant differences in the mean EuroSCORE (13.4 vs 14.3; p = 0.64) or STS scores (5.2 vs 6.4; p = 0.13) of those accepted for TAVI versus those who were not, respectively. When specifically comparing those who underwent TAVI versus those who underwent surgical AVR, there were greater differences in EuroSCORE (13.4 vs 8.2; p = 0.08) and STS score (5.0 vs 4.0; p = 0.26), but these still did not meet statistical significance. Of those who were rejected, 50.0% have died, whereas only 19.7% of those who have received TAVI have died ( Figure 5 ). Mean number of days from time of referral to TAVI was 135. This was longer for the transfemoral (139 days) versus the transapical group (115 days; p = 0.54).
There has been a steady increase in the number of procedures performed annually, with 92 cases to date and with a decreasing proportion of cases being performed transapically ( Figure 6 ). There was 1 death within 7 days because of myocardial infarction and 4 additional deaths during the first 30 days after procedure, giving an overall 30-day mortality of 5.4%. There was no difference in 30-day mortality in the transfemoral (5.1%) versus transapical group (7.1%; p = 0.57). Mortality within 30 days was not significantly different between male and female patients (1.8% vs 10.8%; p = 0.15). Only 6 patients (6.5%) required a permanent pacemaker.