Minimally Invasive Treatment of Atrial Fibrillation
Gorav Ailawadi
INTRODUCTION
Atrial fibrillation (AF) develops in nearly 5% of patients in their lifetime and is the most common arrhythmia. An estimated 5 million Americans suffer from AF, and this number is expected to triple by 2050. AF is associated with an increased risk of stroke, thromboembolism, and death. Moreover, AF is an underdiagnosed cause for tachycardia-induced cardiomyopathy. AF is responsible for nearly 26 billion dollars annually. For these clinical and economic reasons, there is great interest in developing effective treatments for AF.
Medical therapy is the first-line therapy for patients with AF but has been shown to have poor success at rhythm restoration. The advent of surgical and ultimately catheterbased ablation technologies has revolutionized approach for this devastating disease.
AF is now classified by the terms paroxysmal, persistent, and long-standing persistent according to the ACC/AHA guidelines. Paroxysmal is characterized by recurrent episodes that last <7 days or convert to sinus without cardioversion. Persistent AF refers to AF that lasts more than 7 days, while long-standing persistent AF is AF lasting more than 1 year. The terms intermittent, chronic, and permanent AF are no longer in use.
The Cox-Maze III procedure (so-called “Cut and Sew Maze”) became the gold standard for the cure of AF. Although this procedure has excellent long-term results, it was limited in its adoption due to patient morbidity and complexity for the surgeon. Within the last several years, a number of alternate energy sources were developed to create lesion sets to treat AF, which is a variant of the Cox-Maze III, often termed Cox-Maze IV.
PATHOPHYSIOLOGY OF ATRIAL FIBRILLATION
AF is characterized by macro reentrant electrical circuits in both atria. Each patient’s electrical circuitry is unique; thus, mapping AF in any given patient can be laborious and challenging. Endocardial mapping has demonstrated that the pulmonary veins and posterior left atrium are the critical anatomic targets for ablation in patients with isolated AF as well as those with concomitant valvular heart disease. Specifically, in patients with paroxysmal AF, the source for reentrant circuit appears to be from the pulmonary veins while in patients with persistent AF, regular and repetitive activation can be identified in the posterior left atrium, the pulmonary veins, and/or the left atrial appendage (LAA). Although routine intraoperative mapping is currently not feasible for guiding intraoperative AF ablation, an anatomic approach based on our understanding of pathophysiology and on empiric results is reasonable. In fact, such an anatomic (rather than map-guided) approach is rapidly becoming the standard for catheter-based ablation of AF. The Cox-Maze III and IV use predetermined lesions/incisions in anatomic locations to interrupt these circuits. Surgical intervention typically includes excision/ligation of the LAA, which may reduce the risk of recurrent AF, thromboembolism, and stroke.
THE COX-MAZE PROCEDURES
Cox-Maze IV
With recent advances in surgical tools for ablation, there are a number of less invasive approaches to recreate variations of the Cox-Maze III lesion set. The number of cases referred for surgical ablation pales in comparison to those treated via catheter. However, there are several potential advantages to surgical ablation including creation of transmural lesions, direct or endoscopic visualization eliminating the possibility of pulmonary vein stenosis as well as collateral damage to adjacent structures like the esophagus, and the ability to excise or exclude the LAA. Limitations include the inability to replicate the complete Cox-Maze lesion set without opening the heart or performing a concomitant catheter ablation for ablation along the coronary sinus (CS) and cavotricuspid isthmus, as well as poor ability to map for gaps or atrial flutter.
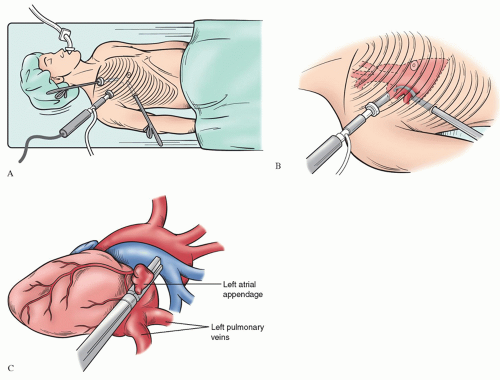
We perform bilateral completely thoracoscopic epicardial ablation followed by endocardial catheter ablation. The patient is placed in supine position with doublelumen endotracheal tube intubation. Three ports are placed in the right chest. Under single-lung ventilation, the right pericardium is opened parallel to the phrenic nerve. The oblique and transverse sinuses are opened bluntly and the right pulmonary veins are encircled using a special dissector. The right veins are ablated using a bipolar radiofrequency (RF) clamp with 3 to 5 successful ablations high on the left atrium. Electrical isolation is confirmed by sensing and pacing the pulmonary veins. The atrial roof and floor lines/connecting lesions are created using a unipolar RF lesions sources from the right side to the left side using thoracoscopic guidance. Unipolar RF can also create a lesion from the superior vena cava (SVC) to the inferior vena cava (IVC) laterally along the right atrium. An SVC encircling lesion is made above the sinus node using bipolar RF. On the left side, the ligament of Marshall is divided after opening the pericardium posterior to the phrenic nerve. The left veins are encircled and ablated using the bipolar RF clamp. The connecting lesions are completed and the LAA is excised with an endoscopic stapler or excluded using commercially available devices (Fig. 66.1). The surgical procedure takes roughly 3 to 4 hours. Patients then undergo catheter procedure at the same setting or at a later date with mitral isthmus/CS ablation and cavotricuspid ablation. The surgical lesions are tested for gaps as well. Our results are fairly consistent with over 85% freedom from AF at 18-month follow-up of antiarrhythmics as tested with 7-day Holter monitor.
There are a number of other less invasive methods to recreate some version of the Cox-Maze III lesion set in patients with lone AF. Another common approach is through a port access approach (right mini thoracotomy) using cardiopulmonary bypass via the femoral vessels. The heart is arrested similar to a minimally invasive approach to the mitral valve. Using cryoablation and RF, the lesion set can be replicated after opening the left atrium. If right atrial lesion sets are planned, femoral venous cannula must be in as far as the SVC and the perfusion must be prepared to get air in the venous line. The LAA is oversewn from the inside. With this approach, centers are reported over 80% success in patients with failed catheter ablation.
Cox-Maze III
The traditional Cox-Maze III procedure infrequently performed today is through a median sternotomy. Cardiopulmonary bypass is established using bicaval and ascending aortic cannulation. Coronary artery bypass grafting distal anastomoses are completed prior to the Cox-Maze III procedure, whereas mitral valve surgery is performed after reconstruction of the left atrium. The heart is arrested using antegrade cardioplegia with or without retrograde cardioplegia.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree