Liability and Risk Management in Fetal Monitoring
Malpractice litigation is prevalent in modern clinical practice, and the associated stress affects all health care providers (1,2). Although not all obstetric malpractice cases involve fetal monitoring, electronic fetal monitoring (EFM) is one of the most common procedures in obstetrics (3), making allegations related to EFM a familiar occurrence in obstetric litigation. Some of the most common allegations leveled against obstetric teams related to fetal monitoring include failure to correctly interpret and/or manage fetal heart rate (FHR) tracings, failures related to team communication, and failure of appropriate provider response to nursing notification of FHR findings (4). And while many clinicians continue to believe that most malpractice suits in obstetrics are frivolous, evidence suggests that substandard care can be linked to adverse outcomes. Specifically, in claims related to EFM and fetal hypoxia, substandard care has been reported to be an issue in as many as 60% of cases (5). Several centers have successfully instituted safety approaches to reduce adverse obstetric outcomes and improve teamwork (6,7 and 8), with some interesting similarities among these initiatives. These include communication and teamwork training, standardized approaches to common clinical practices, improvements in situational awareness, and rapid response teams for emergency situations.
This chapter will address common areas of risk for nurses, midwives, and physicians, with suggested practice strategies using a case-based approach. We will review key aspects of risk management related specifically to fetal monitoring, including suggestions for evaluation and management, documentation, and nurse-provider communication. The case example approach will also illuminate two types of defenses to malpractice allegations. Finally, public policy efforts aimed at the establishment of alternatives to the current tort system will be briefly presented in an effort to enhance awareness of these initiatives.
THE MEDICAL LIABILITY PROCESS
Following a poor obstetric outcome, patients will often initially consult an attorney because they are seeking an answer to the question “Why did this happen?” But the legal process in medical malpractice cases is not necessarily designed to provide answers. Claims of medical and nursing malpractice are adjudicated in civil, versus criminal, courts under the area of law known as tort law. This system is therefore adversarial, with attorneys representing each side of the action, or lawsuit. The goal of the plaintiff is to win the case by proving negligence, or malpractice, while the goal of the defense is to prevent the plaintiff from succeeding. For a plaintiff to win a malpractice suit, four elements must be proven:
Duty—that the patient was owed a specific standard of care by the defendant
Breach—that the defendant failed to meet the specific standard of care
Causation (proximate cause)—that there is a direct relationship between the failure to meet the standard of care (“breach of duty”) and the injury to the patient
Injury—that there was an actual harm or injury
Although “injury” is listed as the fourth element, in reality it is the primary element, for without a recognized injury there can be no lawsuit. The tort system provides only one remedy to an injured party and that remedy is a monetary award known as “damages.” The system is therefore driven by “bad outcomes,” with the severity of the outcome directly proportional to the amount of the potential award. Assuming there is a recognized injury, this leaves the plaintiff with three elements to prove in order to win monetary damages. The first element, duty, is easily proven by establishing a relationship between the health care clinician (nurse, midwife, resident, physician, etc.) and the patient. The next element is breach of duty, which must be established by proving a deviation from the standard of care. The third element, causation
or proximate cause, is proven by the plaintiff establishing a causal link between the alleged deviation(s) of the standard of care and the actual injury sustained. Thus, there are fundamentally two basic types of defenses to allegations of malpractice, and one or both may be used depending upon the facts of the case. The first is a defense premised upon the showing that there was no “breach”; that is, the defendant clinician provided care that was within the “standard of care,” commonly defined in most jurisdictions as care that is reasonable and prudent. The second defense relates to the element of “causation.” The basic assertion of a causation defense is that any breach of the standard of care could not be related to the harm or injury sustained by the plaintiff. In cases involving EFM, an understanding of both defenses is crucial. The following case examples will illustrate a variety of issues in obstetric malpractice related to both standard of
care and causation, and will provide suggestions for practices that both reduce the occurrence of preventable error as well as promote the vigorous defense of appropriate care.
or proximate cause, is proven by the plaintiff establishing a causal link between the alleged deviation(s) of the standard of care and the actual injury sustained. Thus, there are fundamentally two basic types of defenses to allegations of malpractice, and one or both may be used depending upon the facts of the case. The first is a defense premised upon the showing that there was no “breach”; that is, the defendant clinician provided care that was within the “standard of care,” commonly defined in most jurisdictions as care that is reasonable and prudent. The second defense relates to the element of “causation.” The basic assertion of a causation defense is that any breach of the standard of care could not be related to the harm or injury sustained by the plaintiff. In cases involving EFM, an understanding of both defenses is crucial. The following case examples will illustrate a variety of issues in obstetric malpractice related to both standard of
care and causation, and will provide suggestions for practices that both reduce the occurrence of preventable error as well as promote the vigorous defense of appropriate care.
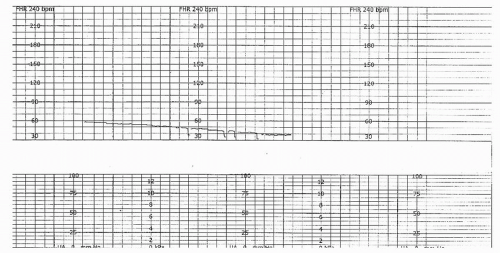
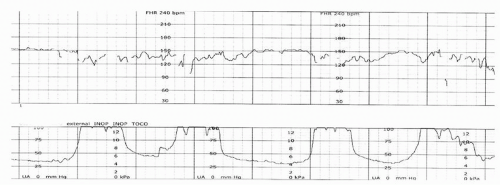
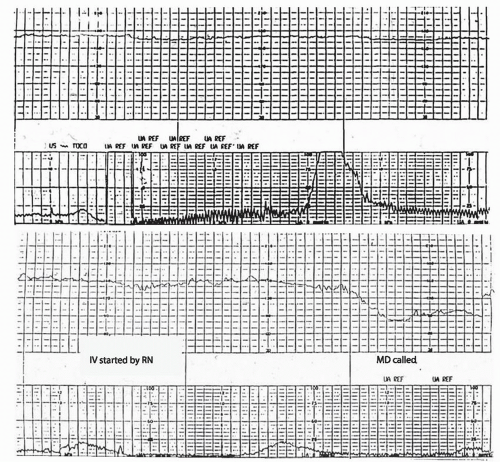 Figure 14.1. Note initial tracing with tachycardia and minimal variability (A), followed by an apparent late deceleration and a prolonged deceleration (B). |
Case Example No. 1
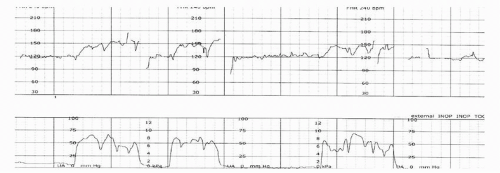
A 39-year-old G3P2002 presented to the hospital for a scheduled nonstress test (NST) at 40 weeks’ gestation due to a complaint of decreased fetal movement in the physician’s office earlier in the day. EFM was applied, and a prolonged deceleration was noted by the nurses (Fig. 14.1A,B), who turned the patient to her side, began an intravenous line, and immediately notified the physician. The physician arrived, viewed the tracing, and documented “NST nonreactive due to patient not eating. Discharge home and repeat NST in AM” (Fig. 14.2A,B). Although the nurses believed
the patient should not be discharged, they did not question the physician’s decision, and the patient was sent home with instructions to rest, increase her fluid intake, and return in the morning. The patient returned and was found to have an intrauterine fetal demise after the nurses were unable to find fetal heart tones (FHTs). Litigation ensued and both the hospital and physician settled for an undisclosed amount.
the patient should not be discharged, they did not question the physician’s decision, and the patient was sent home with instructions to rest, increase her fluid intake, and return in the morning. The patient returned and was found to have an intrauterine fetal demise after the nurses were unable to find fetal heart tones (FHTs). Litigation ensued and both the hospital and physician settled for an undisclosed amount.
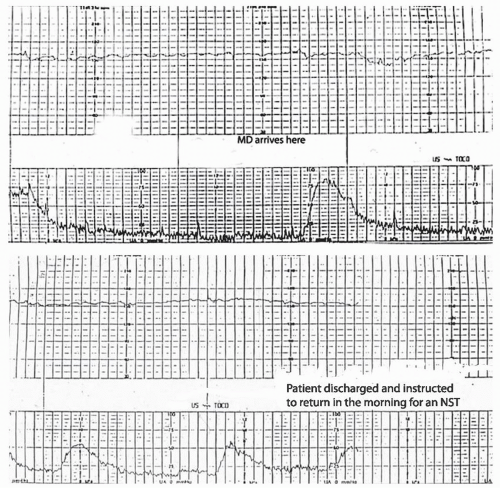 Figure 14.2. Physician arrives and reviews tracing (A); decision to discharge patient with instructions to return for a repeat NST the following morning (B). |
In this case, both the physician and nurses involved deviated from the standard of care by discharging a patient with not only a nonreactive NST but also an FHR tracing demonstrating late and prolonged decelerations. The physician’s apparent belief that the NST was nonreactive because the patient had not eaten was erroneous, and all nonreactive or abnormal antenatal tests require immediate follow-up tests or clinical intervention. Although the nurses disagreed with the physician’s decision, they did not communicate their concern to the physician, nor did they institute the chain of command, or chain of communication, to resolve the issue. When interviewed after the fact, the nurses stated that they were afraid of the physician and “didn’t want to get yelled at.” In 2008, the Joint Commission on Accreditation of Healthcare Organizations (Joint Commission) issued a sentinel event alert addressing the issue of disruptive behavior and its negative impact on patient safety (9). Clinicians must have a mechanism for handling conflict or questioning the plan of care. The modern approach to patient safety recognizes that all team members, regardless of educational background, play pivotal and important roles in patient care. Both physicians and nurses must be able to recognize abnormal FHR changes and provide appropriate followup for antepartum testing. Hospital policies that provide a mechanism for appropriate discussions and input from other team members when questions or concerns arise regarding management plans or FHR tracing interpretation are integral to patient safety. Nurses, midwives, and physicians should receive ongoing communications training and be encouraged to speak up if questions arise, and questions should not be viewed as challenges to authority but rather as fail-safes to prevent unintentional errors. A sample chain of communication model is illustrated in Figure 14.3.
Case Example No. 2
A 23-year-old G1P0000 at term called her physician complaining of labor. The physician sent the patient to the hospital where she was sent to a waiting area for over 2 hours. When placed on the monitor, the nurse could not find FHTs with the external Doppler, though she and another nurse attempted for over 20 minutes. There was no in-house physician to perform artificial rupture of membranes (AROM), although the patient’s exam would have allowed AROM by a qualified clinician. The attending physician was called, and while in route, the patient’s membranes ruptured spontaneously revealing meconium. The nurse then placed a fetal scalp electrode that revealed bradycardia (Fig. 14.4) and the patient was taken to the operating room (OR) for an emergency cesarean delivery. Cord gases revealed metabolic acidemia and the infant required full resuscitation including medications. Following a long course in the neonatal intensive care unit, the infant was discharged and eventually diagnosed with cerebral palsy. Litigation was initiated. The patient testified that she had told the nurse on arrival that she was in labor and had not felt her baby move for several hours. The nurse testified that the patient had not told her of the decreased fetal movement upon arrival, but was unable to explain the extended time in the waiting room prior to evaluation. Plaintiff’s allegations included delay in initial monitoring and delay in obtaining FHR via internal method, with the overall resulting delay in delivery as proximate cause. A confidential settlement was reached for both the hospital and physician.
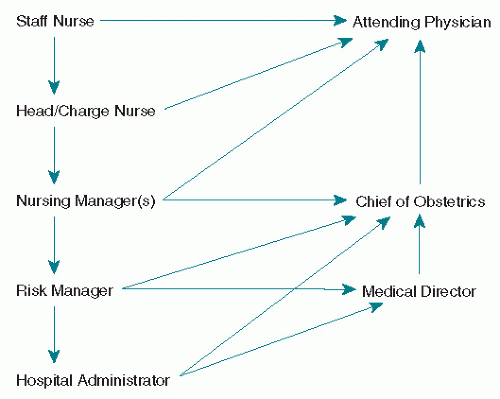 Figure 14.3. Sample chain of communication model. (From Tucker SM, Miller LA, Miller DA. Fetal monitoring: a multidisciplinary approach. 7th ed. Mosby, St. Louis: in press; used with permission) |
Obstetric triage is an area that deserves attention from a risk management perspective. The Guidelines for Perinatal Care state that “a pregnant woman who comes to the labor and delivery area should be evaluated in a timely fashion” (10). Although the term “timely” is not specifically defined, it is unlikely that a delay of 2 hours could be considered reasonable in any patient complaining of labor. And while it is appropriate for nursing staff to initially assess obstetric triage patients, if a nurse is unable to find a FHR in a term patient in a short period of time, an obstetric provider should be notified. This case illustrates the importance of departmental policies for obstetric triage and a systematic approach to dealing with difficulty obtaining FHR data. Many hospitals have implemented the use of an obstetric hospitalist, also known as a laborist, or an in-house call system so that labor and delivery has an obstetrician available for emergencies, and the American College of Obstetricians and Gynecologists (ACOG) has endorsed this approach (11,12). Although it
was published several years after the aforementioned case example, the Association of Women’s Health, Obstetric, and Neonatal Nurses (AWHONN) has a position statement (13) that supports nursing placement of an internal fetal scalp electrode through intact membranes in situations similar to the one described, and hospitals should provide education and training, as well as competence validation, for staff nurses so that they may avoid delay in obtaining FHR data when a physician or midwife is not immediately available. Additionally, nurses can follow AWHONN guidelines for training and competency in limited ultrasound (14), which would also allow documentation of FHR in situations where it may be difficult to find with external Doppler, such as obesity or multiple gestation.
was published several years after the aforementioned case example, the Association of Women’s Health, Obstetric, and Neonatal Nurses (AWHONN) has a position statement (13) that supports nursing placement of an internal fetal scalp electrode through intact membranes in situations similar to the one described, and hospitals should provide education and training, as well as competence validation, for staff nurses so that they may avoid delay in obtaining FHR data when a physician or midwife is not immediately available. Additionally, nurses can follow AWHONN guidelines for training and competency in limited ultrasound (14), which would also allow documentation of FHR in situations where it may be difficult to find with external Doppler, such as obesity or multiple gestation.
Case Example No. 3
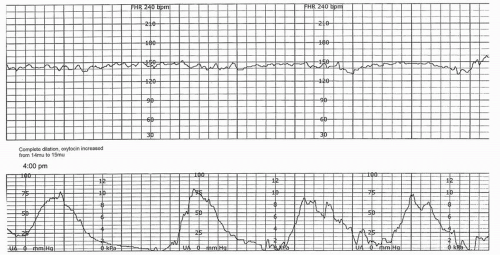
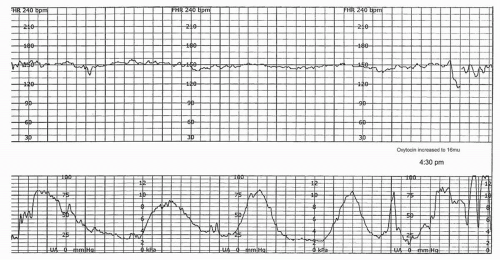
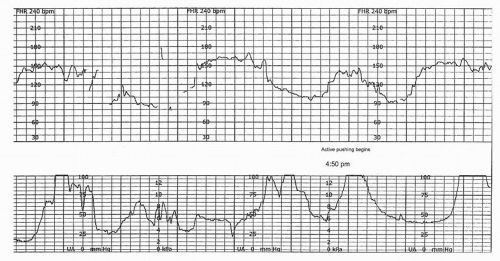
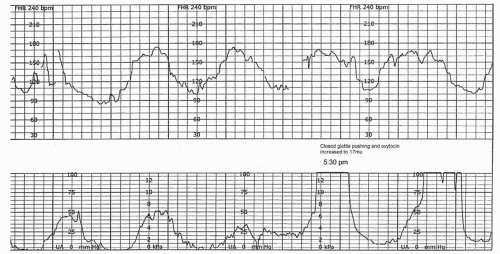
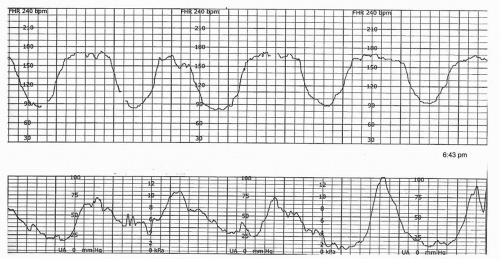
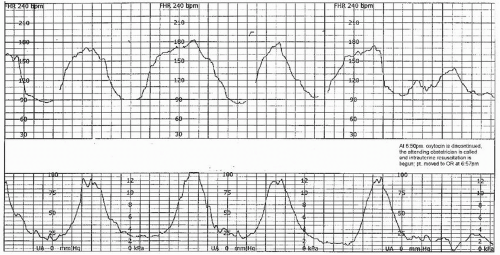
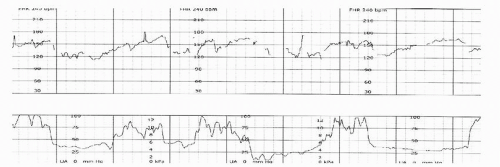
Case example no. 3 involves nursing, midwifery, and obstetric care during the second stage of labor. A 23-year old G1P0000 had an uneventful prenatal course followed by a nurse-midwife who was part of a hospital-owned group practice of physicians and midwives. Labor was augmented with oxytocin due to a protracted active phase following epidural placement. The patient was complete and plus one station at 4:00 pm with a baseline FHR of 145 beats per minute (BPM), moderate variability, no accelerations, and (initially) no decelerations (Fig. 14.5). Although uterine activity appeared adequate and the patient has reached the second stage, the nurse continued to increase the oxytocin, now to 16 mU per minute (Fig. 14.6). The patient begins pushing, and prolonged decelerations soon become evident (Fig. 14.7). The nurse calls the nurse-midwife to the bedside, and the nurse-midwife increases the oxytocin to 17 mU per minute and begins active pushing using the closedglottis technique (Fig. 14.8). The decelerations become recurrent and progressively deeper, accompanied by a rising baseline and loss of moderate variability (Fig. 14.9). The physician is not notified until 6:50 pm, at which time the nurse discontinues Pitocin, instructs the patient to stop pushing, and begins intrauterine resuscitation with position change, IV fluid bolus, and supplemental oxygen (Fig. 14.10). The patient is moved to the OR where an emergency cesarean section is performed under general anesthesia. Delivery occurs at 7:10 pm. Cord gases are obtained, with an arterial cord pH of 6.80 and the base excess reported as “unable to calculate—out of analyzer range.” The initial neonatal diagnosis is hypoxic ischemic encephalopathy (HIE), and the infant is eventually diagnosed with cerebral palsy of the spastic quadriplegic type. Case review revealed all of the essential criteria necessary for establishment of a causative link between intrapartum events and cerebral palsy as discussed in Chapter 3, including metabolic acidemia in arterial cord blood and early onset of severe neonatal encephalopathy. Litigation and a mediation process resulted in a structured settlement.
This case illustrates a number of potential liability areas related to EFM, including basic FHR tracing interpretation, management of oxytocin and uterine activity, and management of the second stage of labor. The nurse and nursemidwife in this case continued to encourage active pushing and continued to increase oxytocin even as the FHR tracing deteriorated. Understanding the mechanisms of different deceleration patterns and the progression from hypoxemia to metabolic acidemia is key to effective clinical practice. Clinicians must recognize that moderate variability and/or FHR accelerations are indicative of the absence of fetal metabolic acidemia at the time of observation (15,16 and 17) and be able to apply this knowledge to tracing evaluation as well as articulate this understanding. The nurse and nurse-midwife in this case failed to recognize the potential for deterioration of fetal acid-base status as the decelerations increased and the variability decreased.
Compounding the problem of tracing interpretation in this case is the continuation of oxytocin. Tachysystole is currently defined as greater than five contractions in a 10-minute window, averaged over 30 minutes, and this definition applies to spontaneous as well as stimulated labors (15,16). The National Institute of Child Health and Human Development (NICHD) workshop panel specifically stated that frequency of contractions (the basis for identification of tachysystole) was only a partial assessment of uterine activity, and the panel noted the importance of other factors, such as duration, strength, and relaxation time, in the clinical evaluation of uterine activity (16). Oxytocin has been designated as a high-alert medication by the Institute for Safe Medication Practice (18). Clinicians must be able to clearly articulate their assessments of uterine activity and, in cases involving the use of oxytocin or other uterine stimulants, their management (and rationale for management) of tachysystole when it does occur. The NICHD panel also recommended further clarification as to the presence or absence of FHR decelerations in association with periods of tachysystole. Clinical recognition of the significance of late, variable, and prolonged decelerations, as well as the absence of clinically significant decelerations, will assist clinicians in their interpretation of uterine activity. Use of a multidisciplinary, standardized protocol that includes a standardized checklist for oxytocin management has been described by Clark et al. (6), resulting in improved outcomes and a significant reduction in claims of obstetric liability.
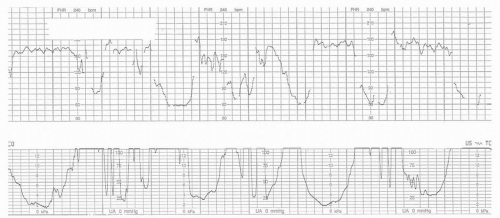 Figure 14.11. Second-stage fetal heart rate pattern with patient pushing on her back and using long Valsalva pushing efforts. |
Second-stage labor management is another issue in this case example. Evidence suggests the use of open-glottis pushing techniques and/or allowing passive descent in the second stage to support fetal oxygenation (19). Improvement of FHR tracings in the second stage may result by simply redirecting or discontinuing pushing efforts, decreasing or discontinuing uterine stimulants if indicated, and maternal position changes and intravenous fluid support. Figure 14.11 illustrates a second-stage pattern where the patient is on her back with legs drawn up and using coached closed-glottis pushing repeatedly during contractions. Figure 14.12 shows the rapid response of the FHR tracing to the following simple nursing interventions: taking a break from pushing, turning the patient to the left side, and providing an intravenous fluid bolus.
Finally, this case again exemplifies the importance of team communication. The physician was not made aware of the FHR tracing until there was no other option than emergent cesarean. Had the nurse and/or nurse-midwife provided ongoing updates related to the deteriorating tracing and the lack of progress, earlier intervention and resuscitation may have resulted in a different outcome.
Case Example No. 4
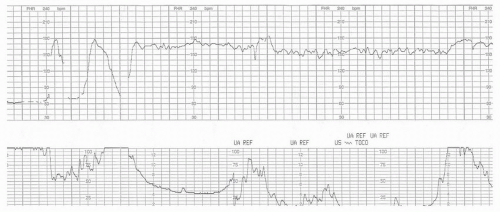
Figures 14.13,14.14,14.15,14.16,14.17,14.18 and 14.19 illustrate another potential problem seen during labor, often in the second stage. This patient had been admitted for an induction of labor due to postdate pregnancy. She progressed to complete and had a somewhat prolonged second stage, but clinicians were unconcerned with the FHR tracing during active pushing, noting that there were “accelerations” during pushing efforts. The infant delivered vaginally, with Apgar scores of 0-0-0 and no response to full resuscitation. Most of the second-stage FHR tracing was actually a recording of maternal heart rate (MHR). The sudden shift in baseline from 150 to 120, along with the disappearance of commonly seen variable decelerations, and the unusual appearance of what appeared to be FHR accelerations but were really accelerations of maternal pulse may be obvious in hindsight but are easily missed in actual practice.
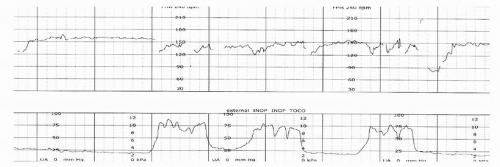 Figure 14.14. Second stage continues, note baseline of 150 with variable decelerations near end of tracing. |
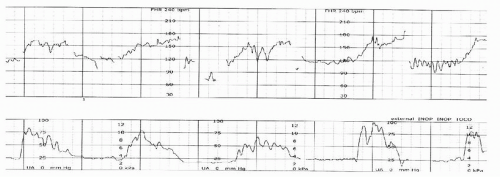 Figure 14.17. Pickup of maternal heart rate continues, last known fetal heart rate was at beginning of second stage. |
In addition to signal ambiguity with MHR, signal coincidence with multiple gestations can also be problematic. Identification and clinical management of both of these issues is detailed in Chapter 4. Regardless of the etiology, clinicians should confirm the validity of the FHR signal every time they make an assessment of the tracing, as shown in the standardized management model described later in this chapter. Documentation of recognition of signal coincidence and/or signal ambiguity, along with corrective actions taken by nursing or medical staff, is a crucial part of record keeping and will assist the clinicians when questions arise regarding validity of the FHR data.
Loss of contiguous tracing and gaps in FHR tracings also occur commonly in the second stage and may be seen frequently in labor during placement of epidural anesthesia (Fig. 14.20). When the patient is repositioned and the FHR tracing is again recording, it is not uncommon to see late or prolonged decelerations due to maternal hypotension (Fig. 14.21). While the majority of these FHR changes are easily resolved by correction of maternal hypotension, clinicians should not hesitate to place an internal fetal electrode if the tracing continues to be questionable. Use of intermittent monitoring during periods of ambulation, during use of alternate measures for pain relief such as the birthing ball or a warm bath/shower, or even simply removing the patient from the monitor to use the bathroom can also lead to allegations regarding adequacy of monitoring. Plaintiffs may attempt to portray these
commonly occurring monitoring lapses as “inadequate monitoring” or even seek experts to speculate that the gaps may hide critical FHR decelerations that clinicians should have attended to with resuscitation. Nursing documentation that shows recognition of the gaps and adjustment of the monitors to obtain an adequate tracing is essential. To avoid problems, reduce risk, and provide care that is both appropriate and defensible, clinicians should have clear guidelines or policies for intermittent monitoring that identify appropriate patient selection, frequency and length of intermittent monitoring, and utilization of auscultation of FHTs per professional guidelines (17,20,21) for periods in which continuous EFM is not being employed.
commonly occurring monitoring lapses as “inadequate monitoring” or even seek experts to speculate that the gaps may hide critical FHR decelerations that clinicians should have attended to with resuscitation. Nursing documentation that shows recognition of the gaps and adjustment of the monitors to obtain an adequate tracing is essential. To avoid problems, reduce risk, and provide care that is both appropriate and defensible, clinicians should have clear guidelines or policies for intermittent monitoring that identify appropriate patient selection, frequency and length of intermittent monitoring, and utilization of auscultation of FHTs per professional guidelines (17,20,21) for periods in which continuous EFM is not being employed.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree