Fig. 65.2 Mechanism of atrial fibrillation (AF). Some AF originates from electrophysiologically active foci in pulmonary veins – isolating these by radiofrequency burns from the rest of the atrium can prevent AF. Some AF is due to re-entry within the atria – these patients may respond to the percutaneous MAZE procedure.
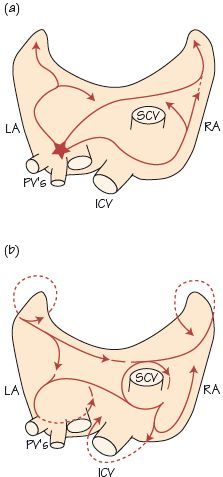
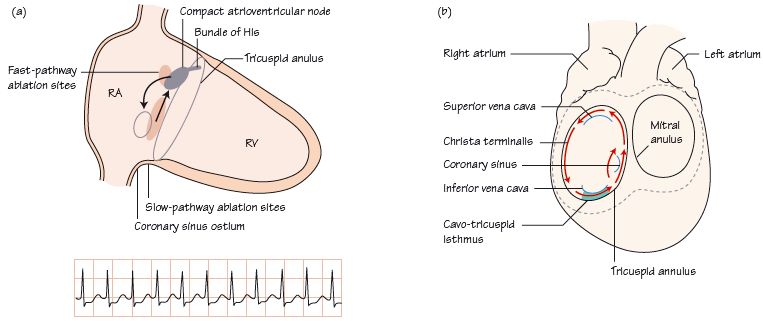
Fig. 65.3 (a) Sites for ablating atrioventricular nodal re-entrant tachycardia (AVNRT). (b) Mechanism of atrial flutter – a ‘burn’ across the cavo-tricuspid isthmus prevents the flutter circuit.
Specialist electrophysiological (EP) investigations have a small but important role in evaluating arrhythmias. They are expensive and are restricted to a few specialized centres; despite their lack of availability it is crucial to refer patients who may benefit.
Standard EP setup
Electrophysiological studies take place in the catheterization laboratory, with the patient draped, sedated, lying on the X-ray table. Catheters are introduced via the right femoral (subclavian) vein, and placed in the: (i) high right atrium; (ii) alongside the atrioventricular (AV) node/bundle of His; (iii) right ventricle (RV) apex (sometimes RV outflow tract); (iv) coronary sinus. A roving catheter may also be used. Electricity detected by these catheters passes to an ECG machine, which records the signals and prints out high speed/gain paper traces. Electrophysiological catheters detect electricity from multiple sites in and around their tip. The aim is to introduce sufficient catheters to accurately determine when different parts of the heart are activated, both in normal sinus rhythm and during an arrhythmia. Many abnormal pathways that sustain arrhythmias generate electricity during sinus rhythm and can be mapped.
Studies to evaluate supraventricular tachyarrhythmias
- Atrioventricular nodal re-entrant tachycardia (AVNRT), due to additional pathway(s) in/around the AV node, can be demonstrated at EP study (Fig. 65.3

Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


