Fig. 3.1
A 69-year-old male patient who underwent left upper lobectomy with systematic nodal dissection in 2010. Pathologic diagnosis: squamous lung carcinoma, pT2aN0M0. During follow-up, CT detected an enlarged (15 mm) subaortic lymph node (a). PET-CT showed an abnormal uptake in the same station (b). A second extended cervical mediastinoscopy was performed. Biopsy of the enlarged node confirmed recurrent squamous carcinoma in the subaortic lymph node station. (c) Shows the 5 mm biopsy forceps biopsying the subaortic space. (d) Final appearance of the biopsy site after checking the haemostasis
ECM is performed through the same cervical incision used for mediastinoscopy. The innominate artery is palpated on its superior surface, directing the finger towards its origin from the aorta. The innominate artery and the aorta are examined digitally to rule out large atheromatous plaques. It is not recommended to proceed further if digital palpation or CT suggests excessive plaque formation [13]. Once this has been ascertained and following the technique described by Ginsberg et al. [12], the fascia between these two vessels is torn with the finger, and the finger can be advanced easily over the aortic arch (Fig. 3.2a) [19]. Lopez et al. [14] have described a modification of this technique in which the retrosternal space is dissected between the anterior surface of the innominate vein and the posterior surface of the sternum.
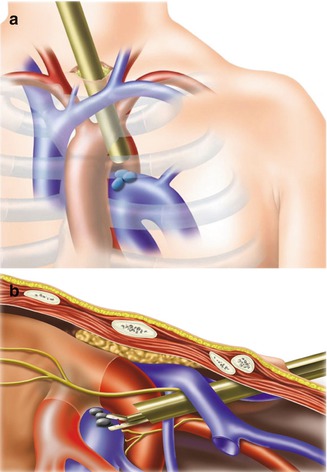
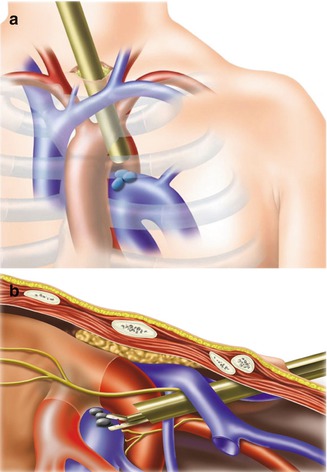
Fig. 3.2
Scheme of anatomic landmarks of ECM in the coronal (a) and sagittal (b) planes (Reproduced from Leyn and Lerut [19] with permission from the editor)
After this digital dissection to create a tunnel, over or under the left innominate vein, the mediastinoscope is advanced over the aortic arch between the innominate artery and the left carotid artery and over the hemiazygos accessory vein (Figs. 3.2 and 3.3) [20]. Lymph nodes can be found among fatty tissue (Fig. 3.2b). By moving the mediastinoscope medially, the para-aortic nodes also can be explored, although differentiating between subaortic (station 5) and para-aortic nodes (station 6) is difficult because mobilization of the mediastinoscope is limited by the bony structures of the chest wall. Before biopsying nodes in this location, it is recommended to puncture any structure of dubious nature to avoid bleeding [13, 20].
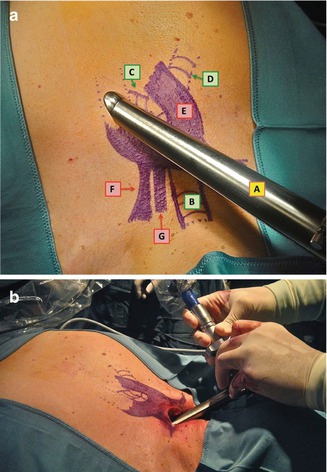
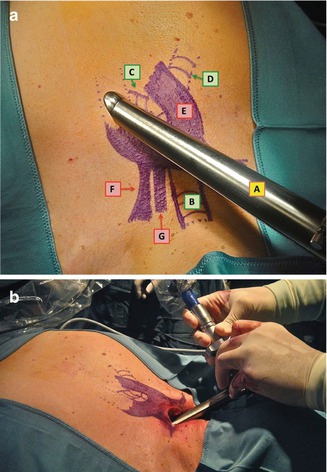
Fig. 3.3
(a) Scheme of the relationship of the mediastinoscope with the main airway, aortic arch and supra-aortic vessels; A, mediastinoscope; B, trachea; C, left main bronchus; D, right main bronchus; E, aortic arch; F, left subclavian artery; G, left carotid artery (Reproduced from Call et al. [20] with permission from the editor). (b) Insertion of the mediastinoscope. The mediastinoscope is inserted obliquely, and it is advanced over the aortic arch between the innominate artery and the left carotid artery to reach the subaortic space (Reproduced from Call et al. [20] with permission from the editor)
One limitation of ECM is that it does not allow the surgeon to palpate the subaortic space properly. If palpation is needed to differentiate between mere contact and tumour invasion in this area, then parasternal mediastinotomy is recommended [20].
3.5.3 Diagnosis of Anterior Mediastinal Masses
After performing the same incision used for standard mediastinoscopy, a 3–5 cm collar incision close to the sternal notch, the retrosternal space is dissected digitally between the anterior surface of the left innominate vein and the posterior surface of the sternum, separating the fascia lying between both structures. This technique allows exploring the aortic arch at the origin of the innominate artery. The presence of preaortic masses is ascertained, first, by finger palpation and, next, by the mediastinoscope, which is introduced through the dissected plane. The suspicious lesion at this location and all neighbouring areas are sampled using the biopsy forceps [8].
However, in presence of invasive neoplasms of the anterior mediastinum, especially when the neighbouring structures are invaded, this approach is rarely performed. In these special cases, anterior mediastinotomy is generally considered safer and more effective [21].
3.6 Results
There are few publications reporting the results of extended cervical mediastinoscopy for staging bronchogenic carcinoma of the left lung. Sensitivity ranges from 0.69 to 0.89; negative predictive value, from 0.89 to 0.97; and, diagnostic accuracy, from 0.91 to 0.98 [12, 14, 15, 22–25]. Although these reported experiences have different selection criteria and prevalences, a consistently high negative predictive value is reported in all of them (Table 3.1). Focusing on the sensitivity of this procedure, when ECM is performed selectively according to the results of CT and PET, the sensitivity increases. This could probably be explained by the higher prevalence of N2-N3 disease in patients with enlarged lymph nodes or abnormal uptake in PET [15].
Table 3.1
Staging values of ECM in the staging of bronchogenic carcinoma of the left lung according to the selection criteria used by each author
Author and reference | Year | Type of ECM | N | S | NPV | Diagnostic accuracy |
|---|---|---|---|---|---|---|
Ginsberg et al. [12] | 1987 | Routine | 100 | 0.69 | 0.89 | 0.91 |
López et al. [14] | 1994 | Selective (CT) | 46 | 0.83 | 0.97 | 0.98 |
Freixinet et al. [22] | 2000 | Selective (CT) | 106 | 0.81 | 0.91 | 0.95 |
Metin et al. [23] | 2011 | Selective (CT and PET) | 55 | 0.69 | 0.89 | 0.91 |
Obiols et al. [24] | 2012 | Routine | 89 | 0.44 | 0.94 | 0.94 |
Selective (CT and PET) | 132 | 0.76 | 0.95 | 0.95 | ||
Witte et al. [25]
Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|