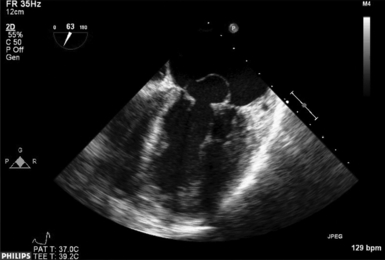
20 Infective endocarditis (IE) is an infection of the endothelium of the heart or blood vessels. Heart valves are particularly susceptible, but IE can occur on any endothelial lined surface, including the papillary muscles, walls of the atria or ventricles, pulmonary artery, or endothelialized surfaces of prosthetic valves or implanted devices such as catheters, pacemakers, and automatic implantable cardioverter-defibrillators (AICDs).1,2 Structural heart disease is the most common predisposing risk factor for IE, which includes acquired valvular disease, congenital abnormalities, prosthetic heart valves, and indwelling devices. Echocardiography is the imaging technology of choice for the diagnosis of IE and recognition of its potential complications.3–5 Once IE is confirmed by blood cultures and echocardiography, appropriate treatment with bactericidal antibiotics and surgery (if indicated) can reduce the morbidity and mortality of IE. Unrecognized and untreated, IE is invariably fatal. 6 Perioperative echocardiography must be performed in IE to help the surgeon in the assessment and management of these patients. 7 The American Heart Association (AHA) estimates the incidence of IE in the United States to be 10,000 to 15,000 new cases annually. 8 The pathophysiologic mechanism of IE is blood flowing from a zone of relatively high pressure to one of lower pressure. If the Reynolds number is surpassed, turbulent flow will be generated and cause endothelial damage, forming a susceptible nidus for implantation and subsequent infection with an adhering organism during bacteremia or fungemia. As part of the native immune response, adherence factors such as fibrin, platelets, and inflammatory cells are drawn to the infective surface, creating a heterogeneous irregular meshwork called vegetation. Vegetations are typically located on the low-pressure side of high-velocity turbulence, on the atrial side of mitral or tricuspid regurgitation, on the ventricular side of aortic or pulmonic regurgitation, on the ventricular side of mitral stenosis, or on the aortic side of aortic stenosis ( Figs. 20-1 and 20-2; Figure 20-2 Three-dimensional en face view of same valve seen Figure 20-1 and Video 20-1 The definitive diagnosis of endocarditis by echocardiography is detection of a vegetation diagnosed with either transthoracic or transesophageal echocardiography (TTE, TEE). This is identified as an irregularly shaped echogenicity mass that may be sessile or pedunculated, mobile or immobile, fibrinous or multilobar and usually has a distinct separation and echogenicity (tissue density) from the underlying valve or endocardial tissue. Infection may involve the valve leaflet or its support apparatus. Any endocardial surface that is attached or adherent to an indwelling cardiac device can also become the site for formation of a vegetation ( Video 20-3 The echocardiogram can also diagnose complications of IE including abscess formation, ruptured chordae or papillary muscle, leaflet or sinus of Valsalva perforation, prosthetic valve dehiscence, development of fistulous tracts, and suppurative pericarditis ( Fig. 20-3 and Video 20-4 The Duke criteria for diagnosis of IE, originally published in 1994 and modified in 2000, includes endocardial involvement as documented by positive TTE or TEE as one of the two major criteria in the diagnosis of endocarditis, the other being positive blood cultures ( Box 20-1).3,11,12 Minor criteria include a broader range of clinical findings: predisposing cardiac conditions, elevated temperature/fever, vascular phenomena, immunologic phenomena, and certain microbiological findings. The criteria also define three diagnostic categories: (1) “definite” by pathologic or clinical criteria, (2) “possible,” and (3) “rejected.” 3 The category “possible IE” is defined as having at least one major criterion and one minor criterion or three minor criteria. 11 The Duke criteria have also been validated in the intravenous drug user (IVDU) population, in whom right-sided endocarditis, especially involving the tricuspid valve, occurs much more frequently than in the non-IVDU population (Video 20-5 Because the clinical presentation of IE can be equivocal and blood cultures may be negative in up to 30% of cases, echocardiography plays a significant role in the definitive diagnosis. Blood culture–negative endocarditis is often due to empirical antibiotic treatment before blood culture sampling or to fungal or fastidious organisms. Among 759 patients with blood culture–negative endocarditis, a causative microorganism was later identified in 62.7% (including Streptococcus, Q fever, and Bartonella infections) and a noninfective etiology in 2.5% (particularly neoplastic or autoimmune disease). 14 With advances in technology, vegetations as small as 1 to 2 mm may be detected on native valves by TTE. However, in 20% to 40% of adult patients, TTE may be inadequate for evaluating suspected endocarditis. 6 Two-dimensional (2D) TTE has a sensitivity for detection of endocarditis of 29% to 65% and a specificity of 90% and is consequently used as an initial screening test in patients with low clinical suspicion of IE. 15 Prosthetic or indwelling devices may be difficult to fully evaluate by TTE owing to acoustic shadowing. TEE has a higher sensitivity (85% to 98%) and a specificity of better than 90% for IE detection because it uses higher transmit frequencies (7 MHz compared to TTE’s 2-4 MHz) and its retrocardiac position is closer to the heart and does not require penetration through the chest wall and lungs, as does TTE. The negative predictive value of TEE is nearly 100% for patients with native valves, but vegetations may be missed with prosthetic valves owing to acoustic shadowing. In a recent study of 511 patients, TTE detected only 45% of vegetations seen by TEE. 15 As a result, TEE should be the initial screening test for all patients with prosthetic valves, suspected technically difficult transthoracic echocardiograms, or indwelling cardiac devices. According to the 2011 appropriate use criteria of echocardiography guidelines, TTE received a score of 9 (the highest score possible) for initial evaluation of suspected endocarditis with positive blood cultures or a new murmur as well as reevaluation of IE at high risk of progressive complications or a change in clinical status or cardiac exam. 16 TEE also carries an appropriate use score of 9 to diagnose IE with a moderate to high test probability (Staphylococcus bacteremia, fungemia, prosthetic heart valve, or intracardiac device). Patients with indwelling hemodialysis catheters, pacemakers, or AICDs can develop endocardial erosions and mural thrombi within the right atrium, tricuspid valve, or right ventricle, which then can become superinfected, producing endocarditis. 17 Additionally, mural endocarditis can occur on the right ventricular side of the interventricular septum or on the contralateral wall of a VSD jet. These structures have to be interrogated carefully when performing a TEE because they may be difficult to image by TTE.
Endocarditis
![]() Videos 20-1 and 20-2). Similarly, if there is a ventricular septal defect (VSD) with left-to-right shunting, the vegetation will be on the low-pressure side, or in this specific scenario, the right ventricular side of the defect. An atrial septal defect (ASD) usually has low pressure on either side of the defect and subsequently does not create a turbulent jet, resulting in a much lower likelihood of developing endocarditis.
Videos 20-1 and 20-2). Similarly, if there is a ventricular septal defect (VSD) with left-to-right shunting, the vegetation will be on the low-pressure side, or in this specific scenario, the right ventricular side of the defect. An atrial septal defect (ASD) usually has low pressure on either side of the defect and subsequently does not create a turbulent jet, resulting in a much lower likelihood of developing endocarditis.
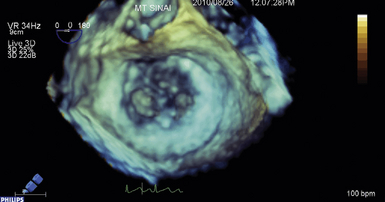
![]() . Vegetations seen in both commissures and at A2.
. Vegetations seen in both commissures and at A2.
![]() ).
).
![]() ). The differential diagnosis of a vegetation includes Libman-Sacks lesions, which are nonbacterial thrombotic lesions found in inflammatory disorders such as systemic lupus erythematosus in up to 18% of patients.9,10 These broad-based lesions may appear on the basilar portion of the valve leaflets (not necessarily associated with jet lesions) and are usually sessile. Marantic endocarditis can also occur in patients with advanced neoplasms such as melanoma and may be difficult to differentiate from endocarditis in a patient with malignancy and fever. Lambl excrescences are small, fibrinous, filiform lesions usually seen on aortic valve leaflet coaptation points as a result of mechanical trauma. They can also appear on the mitral valve (MV).
). The differential diagnosis of a vegetation includes Libman-Sacks lesions, which are nonbacterial thrombotic lesions found in inflammatory disorders such as systemic lupus erythematosus in up to 18% of patients.9,10 These broad-based lesions may appear on the basilar portion of the valve leaflets (not necessarily associated with jet lesions) and are usually sessile. Marantic endocarditis can also occur in patients with advanced neoplasms such as melanoma and may be difficult to differentiate from endocarditis in a patient with malignancy and fever. Lambl excrescences are small, fibrinous, filiform lesions usually seen on aortic valve leaflet coaptation points as a result of mechanical trauma. They can also appear on the mitral valve (MV).
![]() Duke Criteria
Duke Criteria
![]() ). 13 IVDUs with definite diagnosis of IE more commonly have vascular phenomena (arterial embolism, septic pulmonary infarction, mycotic aneurysm, intracranial hemorrhage, or Janeway lesions) and multiple opacities on chest radiography than those with possible endocarditis.
). 13 IVDUs with definite diagnosis of IE more commonly have vascular phenomena (arterial embolism, septic pulmonary infarction, mycotic aneurysm, intracranial hemorrhage, or Janeway lesions) and multiple opacities on chest radiography than those with possible endocarditis.
![]() Transthoracic and Transesophageal Echocardiography
Transthoracic and Transesophageal Echocardiography
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Thoracic Key
Fastest Thoracic Insight Engine