Supraventricular tachycardias (SVTs) are a major cause of morbidity in adults with congenital heart disease (CHD). Few data exist on safety and efficacy of antiarrhythmic drugs in this population. Our aim was to determine the efficacy of antiarrhythmic drugs in adults with CHD and first-onset SVT on maintaining sinus rhythm after conversion. This was a multicenter retrospective study including adults with CHD and first-onset SVT from January 2008 to January 2011. First-onset SVT occurred in 92 of 7,171 patients without previous SVT (mean age 51 ± 16 years, 57% women). SVTs included atrial fibrillation and flutter in >80% of the patients. Most of these patients had septal defects (50%) and left-sided lesions (21%). The acute management of SVTs resulted in sinus rhythm in 83 patients, and 89% of these patients were instituted on oral antiarrhythmics to prevent SVT recurrence. After a mean follow-up of 2.5 ± 1.4 years, only 45% of the patients were free from SVT. Class III antiarrhythmics (85% sotalol and 15% amiodarone) were associated with a significantly lesser risk of SVT recurrence compared with all other antiarrhythmic drugs (hazard ratio 0.5, 95% confidence interval 0.27 to 0.96, p = 0.036). However, adverse effects of medication occurred in 22% of the patients, mainly in patients taking amiodarone. In conclusion, in adults with CHD and first-onset SVTs, class III antiarrhythmics are more efficacious in maintaining sinus rhythm after cardioversion than other antiarrhythmics. Sotalol may be considered as the first-choice therapy as this is associated with fewer adverse effects than amiodarone.
Congenital heart disease (CHD) is the most prevalent form of major birth defects with an incidence of nearly 1%. Owing to diagnostic and therapeutic improvements during the past few decades, the population of adult patients with CHD is growing and aging. However, supraventricular tachycardias (SVT) have been recognized as a major cause of morbidity and have been associated with an increased risk of mortality in this population. The 20-year risk of developing atrial arrhythmias is 7% in a 20-year-old patient with CHD and increases to 38% in a 50-year-old patient with CHD. Atrial arrhythmias are associated with a 2.5-fold greater risk of adverse events with a near 50% increase in mortality. Furthermore, referrals for arrhythmias, most of which are supraventricular, account for 31% to 47% of the hospital admissions in the adult CHD population. Because of the altered anatomy and physiology, arrhythmias in CHD are difficult to treat. Evidence-based guidelines for pharmacologic treatment of atrial arrhythmias are well established in the general adult population; few data exist on its efficacy and safety in the adult CHD population. Therefore, we analyzed the short- and long-term efficacy of different antiarrhythmic drugs in adults with CHD and first-onset SVT.
Methods
This was a multicenter retrospective study including adults with CHD and new-onset SVTs. Patients were identified from the CONCOR database. CONCOR (CONgenital CORvitia) is a nationwide registry of adults with CHD in the Netherlands and aims to facilitate research on outcome and origin of CHD. All adult patients with CHD who developed new-onset SVTs of any type and duration from January 2008 to January 2011 were included in this study. These inclusion dates were chosen as this allowed a follow-up of at least 1 year after a new onset of SVT. Exclusion criteria were permanent atrial fibrillation (AF) or atrial flutter (AFL) and SVTs due to identified noncardiac causes (e.g., anemia, electrolyte imbalance, and hyperthyroidism).
Baseline characteristics included demographics, main cardiac diagnosis, concomitant cardiac conditions, surgical history, medication use, heart failure (HF) symptoms, echocardiographic data within 6 months of first-onset SVT, electrocardiographic (ECG) parameters, and ablations. HF was defined as a syndrome with typical symptoms (e.g., breathlessness, ankle swelling, and fatigue) and signs (e.g., elevated jugular venous pressure, pulmonary crackles, and displaced apex beat) resulting from an abnormality of cardiac structure or function. Echocardiographic data included ventricular function, chamber size, and degree of valvular regurgitation and/or stenosis. Ventricular function was classified as normal (ejection fraction [EF] ≥50%), mildly (EF 40% to 49%), moderately (EF 30% to 39%), and severely (EF <30%) impaired. Ventricular and atrial sizes were qualitatively assessed as normal or enlarged. Valvular dysfunction was graded as absent or mild, moderate, and severe from continuous wave Doppler tracings and Doppler color flow mapping. ECG measurements were rhythm (spontaneous or paced), rate, PR interval, QRS duration, and QT interval. Adverse clinical events were classified as cardiovascular death, thromboembolic events, hospitalization for HF or arrhythmia, and pacemaker insertion.
SVT is any tachycardia that originates in the atria or that uses the atrium or atrioventricular junction and that requires the participation of tissue above the bifurcation of the bundle of His for propagation as a critical component of the tachycardia circle. Arrhythmias were classified according to the American College of Cardiology/American Heart Association/European Society of Cardiology guidelines and included AF, AFL, atrial tachycardia (AT), atrioventricular nodal reentry tachycardia (AVNRT), and unspecified SVT. Arrhythmias were diagnosed by routine electrocardiography. In this study, we only included patients with sustained SVTs who required treatment. In 10% of the patients, spontaneous conversion to sinus rhythm occurred before the treatment was started. Date of the first SVT, the type of SVT, cardiac symptoms during SVT, acute and long-term pharmacologic and interventional management of SVT, and whether the treatment was successful in restoring sinus rhythm were recorded. The acute management of SVTs included vagal maneuvers, electrical cardioversion, intravenous drug therapy, and oral drug therapy. Long-term management of SVTs consisted of new antiarrhythmic drug prescription, pacemaker implantation for bradyarrhythmias, and catheter or surgical ablations. Antiarrhythmic drugs were grouped following the classification by Vaughan Williams.
Data analyses were performed with SPSS software for Windows (version 19.0 for Windows; SPSS Inc., Chicago, Illinois). For all analyses, 2-tailed probability values <0.05 were considered statistically significant. Descriptive statistics for nominal data are expressed in absolute numbers and percentages. After confirming normality, mean values and SDs were calculated for normally distributed continuous variables. When comparing frequencies and means, the chi-square and Student t tests were used, respectively. To identify clinical variables associated with the recurrence of first-onset SVT, we performed univariate Cox regression analysis. Kaplan-Meier estimates were constructed for the time to the first, second, third, and fourth SVT recurrences among various antiarrhythmic drugs and the onset of adverse clinical events. Comparison between groups was performed by log-rank statistics.
Results
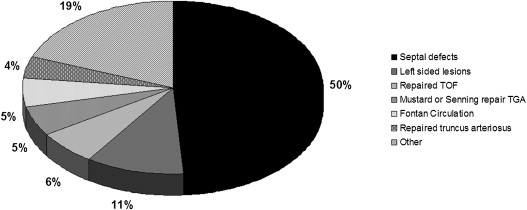
From the 9,537 patients registered in the Concor database at January 2008, 7,171 had no history of SVT. First-onset SVT occurred in 92 of 7,171 patients (43% men) with an annual incidence of 0.4%. The mean duration of follow-up until the development of SVT was 30 ± 9 years. First-onset SVTs included AF (68%), AFL (14%), AVNRT (8%), AT (7%), and unspecified SVT (3%). The underlying cardiac lesion was a septal defect in most patients ( Figure 1 ). Concomitant conditions were present in 57 patients (62%) and are listed in Table 1 . All patients were treated for their cardiac lesion according to the current guidelines. Seventy patients (76%) were symptomatic during their first arrhythmic episode. Arrhythmic symptoms, HF symptoms, and a combination of both were present in 54%, 13%, and 33% of the patients, respectively.
| Characteristic | n (%) |
|---|---|
| Mean age at first-onset SVT in yrs (SD) | 51 ± 16 |
| Men | 48 (52) |
| Surgical repair of CHD | 67 (73) |
| Concomitant conditions | 57 (62) |
| HF | 26 (28) |
| Systemic hypertension | 25 (27) |
| Smoking | 13 (14) |
| Obesity (body mass index ≥30 kg/m 2 ) | 9 (10) |
| Diabetes mellitus | 8 (9) |
| CVA | 6 (7) |
| Myocardial infarction | 2 (2) |
| Medication at baseline | 58 (63) |
| Antiarrhythmics | — |
| β Blocker | 6 (7) |
| Diuretics | 17 (19) |
| ACE inhibitors | 15 (16) |
| Warfarin | 10 (11) |
| Aspirin | 10 (11) |
| Echocardiogram available | 58 (63) |
| At least moderately impaired SVF | 6 (10) |
| At least moderately impaired PVF | 9 (16) |
| At least moderate SAVR | 14 (24) |
| At least moderate PAVR | 19 (33) |
| Dilated left or right atrium | 32 (55) |
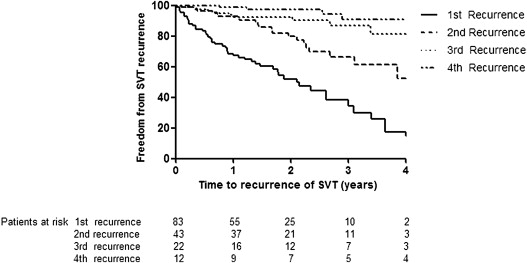
Patients with first-onset SVTs were older than patients without any arrhythmias (51 ± 16 vs 38 ± 14 years, p <0.001). The gender distribution was similar in patients with (43% men) and without SVTs (48% men, p = 0.570). The highest incidence of first-onset SVT was in patients with a truncus arteriosus (15%), univentricular heart (3%), ASD (3%), and transposition of great arteries (1%). In all other diagnoses, the incidence of first-onset SVT was <1%. Figure 2 shows the first and later recurrences of SVT.
The acute management of SVTs consisted of electrical cardioversion (38%), oral antiarrhythmics (38%), and intravenous antiarrhythmic drugs (11%) and resulted in sinus rhythm in 83 (90%) of 92 patients. Table 2 lists a detailed summary of the acute treatment. Spontaneous conversion to sinus rhythm occurred in only 10% of the patients. The patients without sinus rhythm restoration after the acute management were older at the first onset of SVT (69 ± 9 vs 49 ± 15 years, p <0.001), had less frequently repaired cardiac lesions (44% vs 78%, p = 0.026), had more often an impaired systemic ventricular function (33% vs 8%, p = 0.050), and had higher mean creatinine level (108 ± 30 vs 76 ± 18 μmol/L) compared with patients with sinus rhythm recovery.
| Treatment Method | Patients (%) | Success Rate (%) |
|---|---|---|
| Electrical cardioversion | 35 (38) | 31 (89) |
| Vagal maneuvers ∗ | 2 (2) | 0 (0) |
| Intravenous drug therapy | 14 (15) | 14 (100) |
| Adenosine | 3 (21) | 3 |
| Amiodarone | 3 (21) | 3 |
| Sotalol | 2 (14) | 2 |
| Flecainide | 2 (14) | 2 |
| Verapamil | 2 (14) | 2 |
| Metroprolol | 1 (7) | 1 |
| Procainamide | 1 (7) | 1 |
| Oral drug therapy | 34 (37) | 30 (88) |
| Sotalol | 14 (41) | 14 |
| Amiodarone | 2 (6) | 2 |
| Metroprolol | 10 (29) | 6 |
| Verapamil | 4 (12) | 4 |
| Procainamide | 4 (12) | 4 |
| Spontaneous conversion | 9 (10) | 9 (100) |
∗ These patients were treated with intravenous drugs after unsuccessful vagal maneuvers.
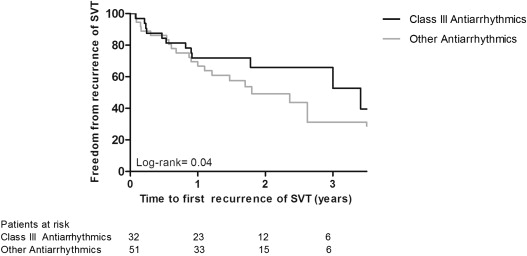
Seventy (84%) of the 83 patients who converted to sinus rhythm after the acute management were instituted on oral antiarrhythmic drugs to maintain sinus rhythm. Various antiarrhythmic drugs of different classes were used in these patients and included class III antiarrhythmics (38% sotalol and 5% amiodarone), class II antiarrhythmics (35%), class I antiarrhythmics (13%), and class IV antiarrhythmics (8%). The drugs and corresponding mean daily dosages are listed in Table 3 . There were only 5 patients who were treated with a combination of antiarrhythmic drugs: 4 with class III or IV antiarrhythmics in combination with a β blocker, 1 patient with class IC in combination with a β blocker. After a mean follow-up of 2.5 ± 1.4 years, only 45% of the patients were free from first SVT recurrence ( Figure 2 ). Class III antiarrhythmics was associated with a significantly less risk of SVT recurrence compared with all other antiarrhythmic drugs (hazard ratio 0.5, 95% confidence interval 0.27 to 0.96, p = 0.036). Notably, the use of class IV antiarrhythmics (verapamil) in 7 patients was associated with a 71% freedom of recurrence (not significant vs all other antiarrhythmics). These drugs were prescribed predominantly for AVNRT or rate control for AF. Figure 3 shows freedom from SVT in patients with and without class III antiarrhythmic drugs during follow-up. The type of SVT was the same during recurrence as the first-onset SVT in 90% of the cases. The type of first-onset SVT did not alter the risk of SVT recurrence during follow-up. There was no difference in recurrence rate of SVT in patients with AF against other types of SVT (p = 0.403). Overall, anticoagulants were prescribed in 63 (68%) of 92 patients.
| Drug | No. of Patients (%) | Mean Dosage (mg/day) |
|---|---|---|
| No antiarrhythmic drugs | 13 (16) | — |
| Class I | ||
| Propafenone | 4 (5) | 563 ± 309 |
| Flecainide | 5 (6) | 120 ± 45 |
| Class II | ||
| Metoprolol | 22 (27) | 69 ± 44 |
| Class III | ||
| Sotalol | 28 (34) | 156 ± 51 |
| Amiodarone | 4 (5) | 350 ± 191 |
| Class IV | ||
| Verapamil | 7 (8) | 166 ± 75 |
During follow-up, 26 SVT ablations were performed in 23 patients. In all patients, ablations were performed only after the first recurrence of SVT. Most of these patients had closed septal defects (52%). The ablation procedures included a concomitant Cox MAZE-III operation in 65%, radiofrequency ablation in 31%, and a mini-MAZE in 4% of the patients. The following arrhythmias were ablated: AF (55%), AFL (23%), AT (12%), and AVNRT (12%). Ablations were classified as successful according to the electrophysiologist directly after the procedure in 18 patients (78%). During a mean follow-up of 1.3 ± 0.9 years after first ablation, 12 (67%) of 18 patients with successful ablation were free from SVT versus 1 (20%) of 5 patients without successful ablation. Three patients had a second ablation during follow-up and were free of recurrences after a mean follow-up of 0.64 ± 0.49 years.
HF at baseline was the only clinical variable associated with recurrences of SVTs during follow-up (hazard ratio 1.9, 95% confidence interval 1.09 to 3.54, p = 0.023). Underlying cardiac defect, ECG measurements, and echocardiographic parameters were not associated with the recurrences of SVTs.
Side effects due to antiarrhythmic drugs occurred in 20 patients (22%). In 85% of these patients, the prescription was changed because of these side effects and included switching to another antiarrhythmic drug (40%), discontinuation of the antiarrhythmic drug (20%), and lowering of the dosage of the antiarrhythmic drug (15%). Table 4 summarizes the side effects of antiarrhythmic drugs in individual patients. Most side effects (75%) occurred in patients with class III antiarrhythmic drugs and were especially driven by the use of amiodarone. Severe side effects occurred in all patients taking amiodarone (mean dosage 350 mg/day) and included thyroid dysfunction (n = 4) and high-grade atrioventricular block (n = 1). Sotalol induced QT prolongation without torsades de pointes in 1 patient.



