Obesity is associated with increased risk for cardiovascular (CV) disease (CVD) and CV mortality. Bariatric surgery has been shown to resolve or improve CVD risk factors, to varying degrees. The objective of this systematic review was to determine the impact of bariatric surgery on CV risk factors and mortality. A systematic review of the published research was performed to evaluate evidence regarding CV outcomes in morbidly obese bariatric patients. Two major databases (PubMed and the Cochrane Library) were searched. The review included all original reports reporting outcomes after bariatric surgery, published in English, from January 1950 to July 2010. In total, 637 studies were identified from the initial screen. After applying inclusion and exclusion criteria, 52 studies involving 16,867 patients were included (mean age 42 years, 78% women). The baseline prevalence of hypertension, diabetes, and dyslipidemia was 49%, 28%, and 46%, respectively. Mean follow-up was 34 months (range 3 to 155), and the average excess weight loss was 52% (range 16% to 87%). Most studies reported significant decreases postoperatively in the prevalence of CV risk factors, including hypertension, diabetes, and dyslipidemia. Mean systolic pressure reduced from to 139 to 124 mm Hg and diastolic pressure from 87 to 77 mm Hg. C-reactive protein decreased, endothelial function improved, and a 40% relative risk reduction for 10-year coronary heart disease risk was observed, as determined by the Framingham risk score. In conclusion, this review highlights the benefits of bariatric surgery in reducing or eliminating risk factors for CVD. It provides further evidence to support surgical treatment of obesity to achieve CVD risk reduction.
Reducing cardiovascular (CV) disease (CVD) risk is a primary public health imperative given the substantial morbidity and mortality associated with the disease. The most effective nonpharmacologic means of achieving such risk reduction is weight loss. Even a moderate 5% to 10% weight loss through diet and lifestyle interventions has been shown to decrease the risk for conversion from impaired glucose tolerance to overt diabetes and can maintain blood pressure reductions over prolonged periods of follow-up. More dramatic weight loss after bariatric surgery has been associated with even greater benefits, such as reduced CV mortality and total mortality in obese patients, particularly those with diabetes. These effects on mortality are due largely to the remarkable consequences of surgical intervention on individual co-morbid conditions such as diabetes, hypertension, and hyperlipidemia. Functional and electrical cardiac investigations also document positive changes in cardiac parameters (structural and electromechanical) after weight reduction. The purpose of this systematic review was to evaluate the current evidence regarding CVD risk reduction after bariatric surgery. We examined the short- and long-term effects of all bariatric interventions on the foremost modifiable traditional risk factors for CVD (hypertension, diabetes mellitus, and hyperlipidemia). We also examined the effects of surgically induced weight loss on objective measures of cardiac function, disease, or risk, by evaluating studies that reported the results of echocardiography, electrocardiography, arterial reactivity testing, C-reactive protein (CRP) levels, and Framingham risk scores pre- and postoperatively.
Methods
The present review was conducted according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses statement. We conducted a comprehensive review of all studies published in English containing data on CV outcomes, risk factors, and risk reduction in obese patients after any form of bariatric surgery. We performed an electronic search in 2 databases (PubMed and the Cochrane Library) for relevant interventional or observational studies published from January 1, 1950, to July 1, 2010. The search string used was as follows: bariatric surgery (Medical Subject Headings [MeSH]) OR obesity/surgery (MeSH) OR gastric bypass (MeSH) OR gastroplasty (MeSH) OR biliopancreatic diversion (MeSH) OR jejunoileal bypass (MeSH) OR gastric banding OR duodenal switch AND cardiovascular diseases (MeSH) AND outcome assessment (health care) (MeSH) OR outcomes. In addition to the primary electronic search, we reviewed the “related citations” linked to each citation in PubMed and manually reviewed the bibliographies of selected reports and reviews published in the past 5 years.
Only reports published in English were included for review. Inclusion criteria were as follows; prospective and retrospective series reporting on outcomes related to CVD, CV risk, objective measures of cardiac function, or cardiac disease biomarkers after bariatric surgery in an obese population. Studies were included if they reported clinical outcome (control of hypertension, hyperlipidemia, and diabetes), laboratory-based measures of cardiac disease and risk (echocardiography, electrocardiography, and CRP), or risk estimates of cardiac disease (Framingham risk score) postoperatively. Case reports or small case series involving <50 patients, review articles, and studies reporting on surgical techniques or weight loss only as a primary outcome were excluded. Multiple publications involving the same series of patients (or duplicate patient populations) were identified and grouped together; only the most recent or parent study was included in this review to avoid double counting of patients. In cases in which we were uncertain about duplicate patient groups (the same group or institution reporting outcomes for a similar period, without clear indications that the smaller report was a substudy or interim results), a consensus was reached among the investigators regarding its inclusion or exclusion.
Data extraction from selected studies was based on protocol-defined criteria. Statistical analyses were performed only on the extracted data from the selected studies. Basic descriptive statistics (simple counts and means) were used to summarize the patient and study characteristics, reported weight loss, and CV risk factor data. Average unweighted values were calculated for the weight loss, CV risk factor, and mortality data across all studies and for the different operative procedures. Outcomes collected for CV risk reduction included resolution or reduction of hypertension, dyslipidemia, and diabetes; decrease in CRP level; decrease in Framingham risk score; or other improvements in markers of cardiac disease or function. Other efficacy outcomes collected included percentage excess weight loss (%EWL). Where %EWL was not specifically stated, but weight loss was reported in terms of body mass index (BMI) reduction, %EWL was calculated as (BMI at baseline − BMI postoperatively)/(BMI at baseline − 25) × 100, on the basis of the assumption that “ideal weight” after bariatric surgery was equivalent to achieving a BMI of 25 kg/m 2 . These outcomes were assessed at the longest time point for which data were available on ≥50% of the initial patient population. In studies with control groups, the change in values between baseline and follow-up indicators of CV risk was obtained for the surgical cohort only. For studies that reported results by gender, age, or race, we calculated the overall results using the proportional mix of genders (or other variables) and individual scores. CVD risk reduction indicators were expressed as the percentage of patients who had resolution or reduction of hypertension, dyslipidemia, and diabetes as determined by clinical or laboratory measurements (blood pressure readings, serum lipid profiles, and fasting blood glucose and glycosylated hemoglobin measures, respectively) or changes in medication requirements for each co-morbidity postoperatively. Mean patient characteristics were synthesized by calculating raw weighted means; the denominator used to obtain results varied according to the individual characteristics reported. Comparisons of the different bariatric procedures with respect to improvements in CV outcomes postoperatively were performed using the chi-square test and/or 1-way analysis of variance, as appropriate, for the pooled data across all studies.
Results
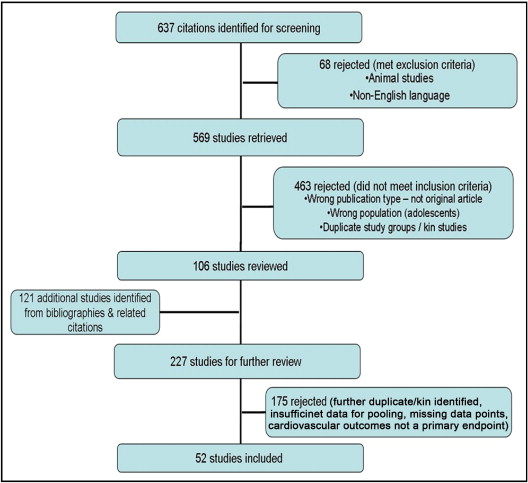
After the initial screening of titles and abstracts (n = 637), 68 were excluded, and 569 studies were reviewed to determine whether they met the inclusion criteria. Of these, 463 were excluded at this stage of the review because they were not original reports of adult bariatric populations, involved duplicate patient groups, or were substudies of larger series. On review of the remaining 106 publications in full, a further 121 studies were identified from bibliographies and related citations that were deemed suitable for inclusion. Of these 227 primary studies, only 52 contained sufficient detail to merit inclusion in the extractable and analyzable data set ( Figure 1 ) .
The data set consisted of 52 original studies involving 16,867 patients who had undergone primary bariatric procedures. Of these 52 studies, most from United States (n = 25) and Europe (n = 16), with the remaining 11 from Taiwan (n = 4), Australia (n = 2), New Zealand (n = 1), Canada (n = 1), South America (n = 1), and Israel (n = 2). Data from 2 studies published by the Swedish Obese Subjects Study Scientific Group were included and merged to ensure that the patient cohort was counted only once. Regarding study design, there were 2 randomized prospective trials, 3 nonrandomized prospective trials, 1 comparative prospective study, 4 comparative retrospective studies, 2 observational case-control studies, 20 uncontrolled prospective case series, and 20 retrospective case series. Each of the extracted studies included >1of the outcomes of interest. Of the 52 studies, 43 addressed the impact of bariatric surgery on traditional CV risk factors, including hypertension, diabetes, and dyslipidemia, and 9 studies examined the effects of surgically induced weight loss on novel CV risk factors (CRP, albuminuria, and proinflammatory markers), risk scores, and CV-related biochemical or functional investigations ( Table 1 ).
| First Author | Year | Country | n | Follow-Up (Months) | Mean Age (Years) | Women | Baseline BMI (kg/m 2 ) | Study Procedures |
|---|---|---|---|---|---|---|---|---|
| Traditional CV risk factor studies | ||||||||
| Adami | 2005 | Italy | 461 | 36 | 41.5 | 59% | 49 | BPD |
| Ahmed | 2009 | United States | 100 | 12 | 42 | 89% | 49 | RYGB |
| Ahroni | 2005 | United States | 195 | 12 | 43.8 | 83% | 49 | LGB |
| Alexandrides | 2007 | Greece | 137 | 26 | 41.4 | 77% | 46 | RYGB and BPD |
| Anderson | 2007 | United States | 50 | 12 | 43 | 74% | 56 | RYGB |
| Bacci | 2002 | Italy | 50 | 12 | 42 | 94% | 55 | LGB |
| Batsis | 2007 | United States | 197 | 40 | 44 | 8% | 51 | RYGB |
| Bowne | 2006 | United States | 106 | 40 | 42 | 80% | 44 | LGB and RYGB |
| Brancatisano | 2008 | Australia | 838 | 36 | 44 | 8% | 50 | LGB |
| Cottam | 2006 | United States | 362 | 36 | 43 | 85% | 56 | LGB and RYGB |
| Cowan | 1998 | United States | 82 | 12 | 38 | 74% | 44 | RYGB |
| Fernstrom | 2006 | United States | 347 | 18 | 40 | 77% | 42 | RYGB and VBG |
| Frigg | 2004 | Switzerland | 295 | 48 | 41 | 79% | 47 | LGB |
| Goergen | 2007 | Luxemburg | 110 | 24 | 41 | 76% | 47 | RYGB and VBG |
| Khalaileh | 2008 | Israel | 50 | 12 | 37 | 66% | 54 | RYGB |
| Larrad-Jimenez | 2007 | Spain | 343 | 120 | 41 | 80% | 45 | BPD |
| Lee | 2004 | Taiwan | 645 | 12 | 30 | 6% | 45 | RYGB and VBG |
| Maher | 2008 | United States | 450 | 12 | 42 | 80% | 47 | RYGB |
| Mattar | 2005 | United States | 70 | 15 | 47 | 69% | 56 | RYGB, LGB, and SG |
| Müller | 2008 | Switzerland | 50 | 48 | 38 | 80% | 43 | RYGB |
| Obeid | 2005 | United States | 925 | 3 | 45 | 87% | 45 | RYGB |
| O’Brien | 2002 | Australia | 709 | 12 | 41 | 85% | 47 | LGB |
| Papasavas | 2002 | United States | 116 | 6 | 42 | 87% | 52 | RYGB |
| Paran | 2007 | Israel | 115 | 85 | 39 | 76% | 43 | VBG |
| Peluso | 2007 | United States | 400 | 24 | 45 | 84% | 39 | RYGB |
| Pinheiro | 2008 | Brazil | 105 | 48 | 54 | 71% | 50 | RYGB |
| Ponce | 2004 | United States | 402 | 24 | 42 | 83% | 46 | LGB |
| Pontiroli | 2009 | Italy | 101 | 65 | 45 | 83% | 51 | LGB and BPD |
| Prachand | 2010 | United States | 350 | 36 | 40 | 83% | 45 | RYGB and BPD with DS |
| Puzziferri | 2006 | United States | 155 | 36 | 48 | 92% | 49 | RYGB |
| Sampalis | 2006 | Canada | 1,035 | 30 | 45 | 66% | 47 | RYGB and VBG |
| Scopinaro | 1998 | Italy | 1,356 | 155 | 37 | 68% | 48 | BPD |
| Sears | 2008 | United States | 75 | 12 | NA | NA | 54 | RYGB |
| Singhal | 2008 | United Kingdom | 122 | 12 | 45 | 75% | 46 | LGB |
| Sjöström , ⁎ | 2007 2004 | Sweden | 2,010 | 131 | 47 | 71% | 48 | LGB, RYGB and VBG |
| Spivak | 2004 | United States | 271 | 6 | 25 | 87% | 58 | LGB |
| Steffen | 2009 | Switzerland | 388 | 84 | 43 | 77% | 48 | LGB and RYGB |
| Sugerman | 2003 | United States | 1,025 | 144 | 39 | 78% | NA | RYGB |
| Valera-Mora | 2005 | Italy | 107 | 24 | 37 | 79% | 47 | BPD |
| Vila | 2009 | Spain | 115 | 24 | 45 | NA | 52 | BPD |
| White | 2005 | New Zealand | 342 | 48 | 43 | 76% | 53 | RYGB (and Silastic ring) |
| Yan | 2008 | United States | 59 | 60 | 49 | NA | 52 | RYGB |
| Novel CV risk factor/score | ||||||||
| Agrawal | 2009 | United States | 62 | 15 | 46 | 82% | 47 | RYGB |
| Arterburn | 2009 | United States | 92 | 12 | 46 | 78% | 45 | RYGB |
| Chen | 2009 | Taiwan | 640 | 12 | 31 | 69% | 43 | LGB and “mini-bypass” |
| Habib | 2009 | United States | 50 | 12 | 44 | 76% | 53 | RYGB |
| Hsuan | 2010 | Taiwan | 66 | 3 | 31 | 65% | 52 | RYGB and SG |
| Kligman | 2007 | United States | 97 | 12 | 43 | 89% | 49 | RYGB |
| Lin | 2007 | Taiwan | 69 | 6 | 34 | 71% | 52 | VBG |
| Serra | 2006 | Spain | 70 | 12 | 42 | 59% | 46 | RYGB |
| Torquati | 2007 | United States | 500 | 12 | 45 | 81% | 48 | RYGB |
| Total | 16,867 | 34 | 42 | 78% | 48 |
⁎ Data taken from 2 publications by the same group on the same cohort of obese surgical patients.
In total, 16,867 patients were investigated in the 52 studies. At baseline, the mean age of the patients was 42 years (range of mean ages 25 to 54), 78% of the population were women, and the mean BMI was 49 kg/m 2 (range of mean BMIs reported 39 to 58). The baseline prevalence of those obesity-related co-morbidities, which increase the risk for CVD, is listed in Table 2 . Malabsorptive or bypass procedures were most commonly performed, with Roux-en-Y gastric bypass (RYGB) and biliopancreatic diversion (BPD) accounting for 62.0% of cases ( Figure 2 ) . The mean follow-up duration was 34 months (range 3 to 155), with 23% of studies reporting medium- to long-term results of >48 months. Weight loss after bariatric surgery (all types) was quantified and reported in all but 1 study, and the overall mean %EWL was 52% (range 16% to 87%). Examining weight loss according to the various procedures performed revealed that malabsorptive procedures such as RYGB and BPD resulted in greater weight loss (65% and 69%, respectively) than restrictive procedures ( Figure 3 ). Laparoscopic gastric banding resulted in the lowest %EWL overall (42%).
| Co-Morbidity | Baseline | Percentage Resolution or Reduction ⁎ |
|---|---|---|
| Hypertension | 49% | 68% |
| Diabetes mellitus | 28% | 75% |
| Dyslipidemia | 46% | 71% |

Most studies reported significant decreases postoperatively in the prevalence of obesity-related co-morbidities that present a risk for CVD; on average, hypertension remitted or resolved in 68%, diabetes in 75%, and dyslipidemia in 71% ( Table 2 ). These improvements occurred as early as 3 months (when investigators looked at short-term effects, or serially over a longer duration of follow-up) and persisted throughout the duration of follow-up (up to 155 months). Examining the change in co-morbidity status postoperatively according to the different bariatric procedures performed showed that BPD and vertical banded gastroplasty resulted in greater remission or reduction rates of all 3 co-morbidities compared to RYGB and laparoscopic gastric banding. Overall, laparoscopic gastric banding resulted in the lowest rates of remission or reduction of diabetes (71%) and hypertension (58%), although the differences between procedures were marginal ( Figure 3 ). Blood pressure measurements pre- and postoperatively were documented in 42% of studies. Mean systolic pressure reduced from to 139 to 124 mm Hg and mean diastolic pressure from 87 to 77 mm Hg ( Table 3 ). Lipid profiles were also reported pre- and postoperatively in 42% of studies and had altered significantly after surgical intervention. Mean total cholesterol, low-density lipoprotein cholesterol, and triglyceride levels decreased, while high-density lipoprotein increased ( Table 3 ). Postoperative changes in fasting blood glucose and glycosylated hemoglobin were reported in 27% and 11.5% of studies, respectively. Average fasting glucose level decreased from 119 to 92 mg/dl, and glycosylated hemoglobin decreased by 1.5%, which would be considered a clinically significant reduction.
| Variable | Baseline | Postoperatively ‡ |
|---|---|---|
| Fasting blood glucose (mg/dl) | 126 | 92 |
| Glycosylated hemoglobin (%) | 7.5 | 6.0 |
| Systolic blood pressure (mm Hg) | 139 | 124 |
| Diastolic blood pressure (mm Hg) | 87 | 77 |
| Total cholesterol (mg/dl) | 205 | 169 |
| LDL (mg/dl) | 118 | 94 |
| HDL (mg/dl) | 49 | 52 |
| Triglycerides (mg/dl) | 169 | 103 |
| CRP (mg/L) ⁎ | 4.5 | 1.7 |
| Flow-mediated diameter of brachial artery (% change) † | 6% | 16% |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


