DYSPNEA
DYSPNEA
The American Thoracic Society defines dyspnea as a “subjective experience of breathing discomfort that consists of qualitatively distinct sensations that vary in intensity. The experience derives from interactions among multiple physiological, psychological, social, and environmental factors and may induce secondary physiological and behavioral responses.” Dyspnea, a symptom, must be distinguished from the signs of increased work of breathing.
MECHANISMS OF DYSPNEA
Respiratory sensations are the consequence of interactions between the efferent, or outgoing, motor output from the brain to the ventilatory muscles (feed-forward) and the afferent, or incoming, sensory input from receptors throughout the body (feedback), as well as the integrative processing of this information that we infer must be occurring in the brain (Fig. 5-1). In contrast to painful sensations, which can often be attributed to the stimulation of a single nerve ending, dyspnea sensations are more commonly viewed as holistic, more akin to hunger or thirst. A given disease state may lead to dyspnea by one or more mechanisms, some of which may be operative under some circumstances, e.g., exercise, but not others, e.g., a change in position.
FIGURE 5-1
Hypothetical model for integration of sensory inputs in the production of dyspnea. Afferent information from the receptors throughout the respiratory system projects directly to the sensory cortex to contribute to primary qualitative sensory experiences and provide feedback on the action of the ventilatory pump. Afferents also project to the areas of the brain responsible for control of ventilation. The motor cortex, responding to input from the control centers, sends neural messages to the ventilatory muscles and a corollary discharge to the sensory cortex (feed-forward with respect to the instructions sent to the muscles). If the feed-forward and feedback messages do not match, an error signal is generated and the intensity of dyspnea increases. (Adapted from MA Gillette, RM Schwartzstein: Mechanisms of dyspnea, in Supportive Care in Respiratory Disease, SH Ahmedzai and MF Muer [eds]. Oxford, UK, Oxford University Press, 2005.)
Motor efferents
Disorders of the ventilatory pump, most commonly increase airway resistance or stiffness (decreased compliance) of the respiratory system, are associated with increased work of breathing or a sense of an increased effort to breathe. When the muscles are weak or fatigued, greater effort is required, even though the mechanics of the system are normal. The increased neural output from the motor cortex is sensed via a corollary discharge, a neural signal that is sent to the sensory cortex at the same time that motor output is directed to the ventilatory muscles.
Sensory afferents
Chemoreceptors in the carotid bodies and medulla are activated by hypoxemia, acute hypercapnia, and acidemia. Stimulation of these receptors, as well as others that lead to an increase in ventilation, produce a sensation of air hunger. Mechanoreceptors in the lungs, when stimulated by bronchospasm, lead to a sensation of chest tightness. J-receptors, sensitive to interstitial edema, and pulmonary vascular receptors, activated by acute changes in pulmonary artery pressure, appear to contribute to air hunger. Hyperinflation is associated with the sensation of increased work of breathing and an inability to get a deep breath or of an unsatisfying breath. Metaboreceptors, located in skeletal muscle, are believed to be activated by changes in the local biochemical milieu of the tissue active during exercise and, when stimulated, contribute to the breathing discomfort.
Integration: Efferent-reafferent mismatch
A discrepancy or mismatch between the feed-forward message to the ventilatory muscles and the feedback from receptors that monitor the response of the ventilatory pump increases the intensity of dyspnea. This is particularly important when there is a mechanical derangement of the ventilatory pump, such as in asthma or chronic obstructive pulmonary disease (COPD).
Anxiety
Acute anxiety may increase the severity of dyspnea either by altering the interpretation of sensory data or by leading to patterns of breathing that heighten physiologic abnormalities in the respiratory system. In patients with expiratory flow limitation, for example, the increased respiratory rate that accompanies acute anxiety leads to hyperinflation, increased work and effort of breathing, and a sense of an unsatisfying breath.
ASSESSING DYSPNEA
Quality of sensation
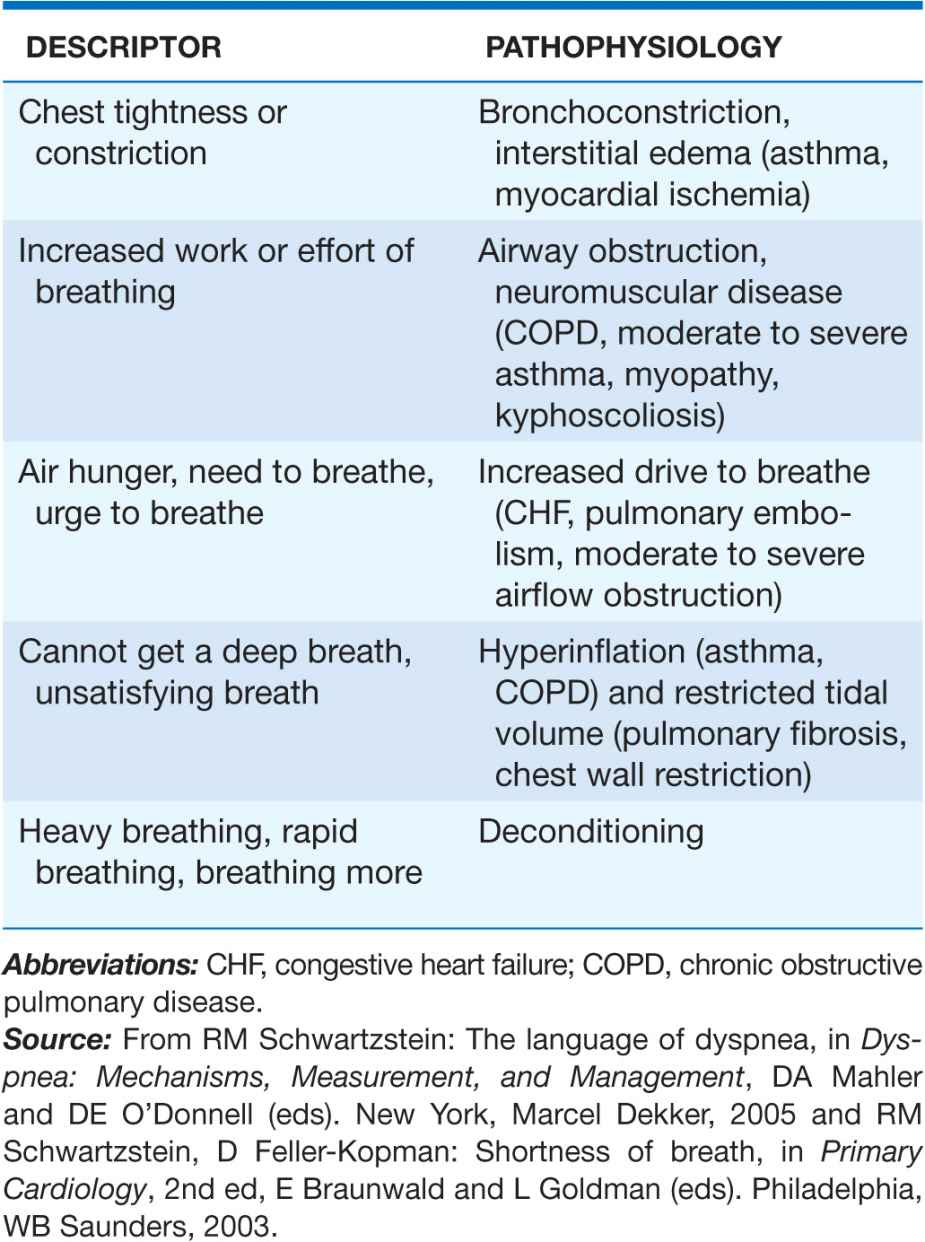
As with pain, dyspnea assessment begins with a determination of the quality of the discomfort (Table 5-1). Dyspnea questionnaires, or lists of phrases commonly used by patients, assist those who have difficulty describing their breathing sensations.
TABLE 5-1
ASSOCIATION OF QUALITATIVE DESCRIPTORS AND PATHOPHYSIOLOGIC MECHANISMS OF SHORTNESS OF BREATH
Sensory intensity
A modified Borg scale or visual analogue scale can be utilized to measure dyspnea at rest, immediately following exercise, or on recall of a reproducible physical task, e.g., climbing the stairs at home. An alternative approach is to inquire about the activities a patient can do, i.e., to gain a sense of the patient’s disability. The Baseline Dyspnea Index and the Chronic Respiratory Disease Questionnaire are commonly used tools for this purpose.
Affective dimension
For a sensation to be reported as a symptom, it must be perceived as unpleasant and interpreted as abnormal. Laboratory studies have demonstrated that air hunger evokes a stronger affective response than does increased effort or work of breathing. Some therapies for dyspnea, such as pulmonary rehabilitation, may reduce breathing discomfort, in part, by altering this dimension.
DIFFERENTIAL DIAGNOSIS
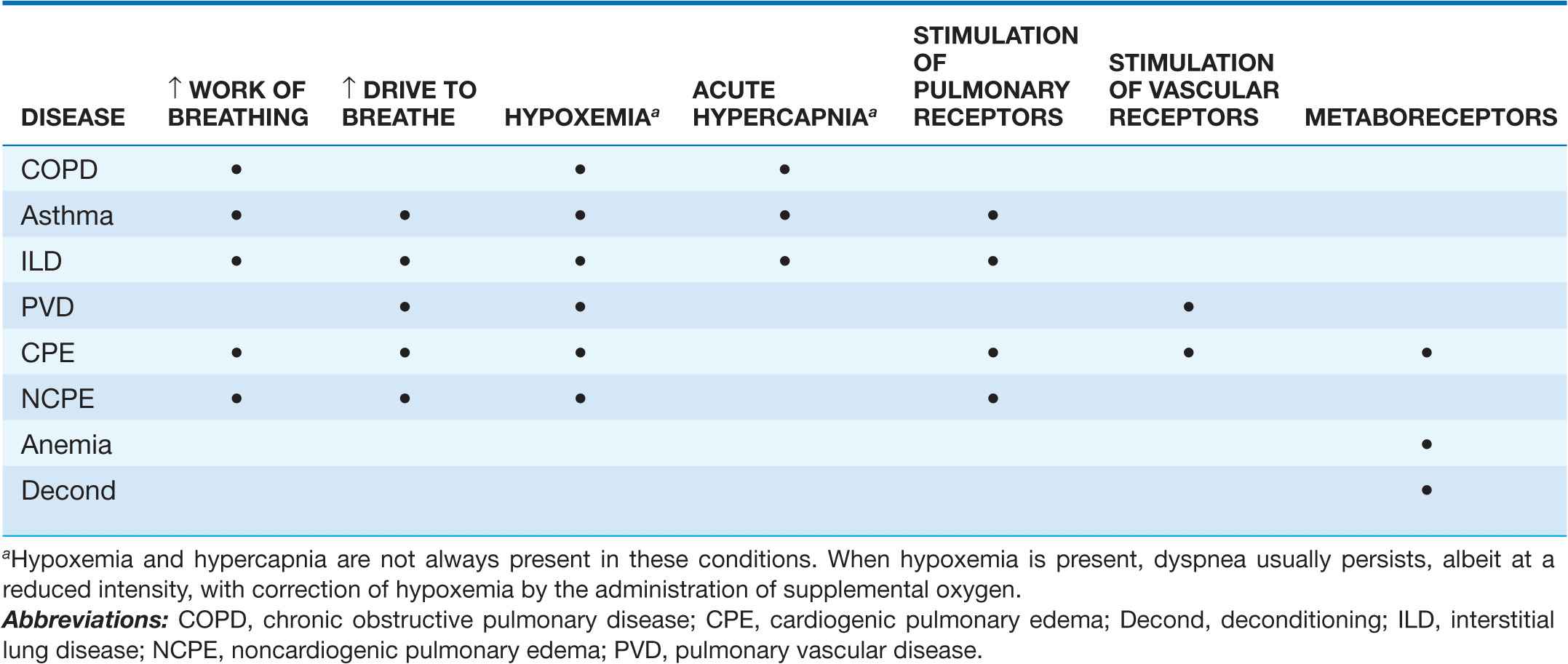
Dyspnea is the consequence of deviations from normal function in the cardiopulmonary systems. These deviations produce breathlessness as a consequence of increased drive to breathe; increased effort or work of breathing; and/or stimulation of receptors in the heart, lungs, or vascular system. Most diseases of the respiratory system are associated with alterations in the mechanical properties of the lungs and/or chest wall, frequently as a consequence of disease of the airways or lung parenchyma. In contrast, disorders of the cardiovascular system more commonly lead to dyspnea by causing gas exchange abnormalities or stimulating pulmonary and/or vascular receptors (Table 5-2).
TABLE 5-2
MECHANISMS OF DYSPNEA IN COMMON DISEASES
Respiratory system dyspnea
 Diseases of the airways
Diseases of the airways
Asthma and COPD, the most common obstructive lung diseases, are characterized by expiratory airflow obstruction, which typically leads to dynamic hyperinflation of the lungs and chest wall. Patients with moderate to severe disease have increased resistive and elastic loads (a term that relates to the stiffness of the system) on the ventilatory muscles and increased work of breathing. Patients with acute bronchoconstriction also complain of a sense of tightness, which can exist even when lung function is still within the normal range. These patients commonly hyperventilate. Both the chest tightness and hyperventilation are probably due to stimulation of pulmonary receptors. Both asthma and COPD may lead to hypoxemia and hypercapnia from ventilation-perfusion (![]() /Q) mismatch (and diffusion limitation during exercise with emphysema); hypoxemia is much more common than hypercapnia as a consequence of the different ways in which oxygen and carbon dioxide bind to hemoglobin.
/Q) mismatch (and diffusion limitation during exercise with emphysema); hypoxemia is much more common than hypercapnia as a consequence of the different ways in which oxygen and carbon dioxide bind to hemoglobin.
 Diseases of the chest wall
Diseases of the chest wall
Conditions that stiffen the chest wall, such as kyphoscoliosis, or that weaken ventilatory muscles, such as myasthenia gravis or the Guillain-Barré syndrome, are also associated with an increased effort to breathe. Large pleural effusions may contribute to dyspnea, both by increasing the work of breathing and by stimulating pulmonary receptors if there is associated atelectasis.
 Diseases of the lung parenchyma
Diseases of the lung parenchyma
Interstitial lung diseases, which may arise from infections, occupational exposures, or autoimmune disorders, are associated with increased stiffness (decreased compliance) of the lungs and increased work of breathing. In addition, ![]() /Q mismatch, and destruction and/or thickening of the alveolar-capillary interface may lead to hypoxemia and an increased drive to breathe. Stimulation of pulmonary receptors may further enhance the hyperventilation characteristic of mild to moderate interstitial disease.
/Q mismatch, and destruction and/or thickening of the alveolar-capillary interface may lead to hypoxemia and an increased drive to breathe. Stimulation of pulmonary receptors may further enhance the hyperventilation characteristic of mild to moderate interstitial disease.
Cardiovascular system dyspnea
 Diseases of the left heart
Diseases of the left heart
Diseases of the myocardium resulting from coronary artery disease and nonischemic cardiomyopathies result in a greater left-ventricular end-diastolic volume and an elevation of the left-ventricular end-diastolic, as well as pulmonary capillary pressures. These elevated pressures lead to interstitial edema and stimulation of pulmonary receptors, thereby causing dyspnea; hypoxemia due to ![]() /Q mismatch may also contribute to breathlessness. Diastolic dysfunction, characterized by a very stiff left ventricle, may lead to severe dyspnea with relatively mild degrees of physical activity, particularly if it is associated with mitral regurgitation.
/Q mismatch may also contribute to breathlessness. Diastolic dysfunction, characterized by a very stiff left ventricle, may lead to severe dyspnea with relatively mild degrees of physical activity, particularly if it is associated with mitral regurgitation.
 Diseases of the pulmonary vasculature
Diseases of the pulmonary vasculature
Pulmonary thromboembolic disease and primary diseases of the pulmonary circulation (primary pulmonary hypertension, pulmonary vasculitis) cause dyspnea via increased pulmonary-artery pressure and stimulation of pulmonary receptors. Hyperventilation is common, and hypoxemia may be present. However, in most cases, use of supplemental oxygen has minimal effect on the severity of dyspnea and hyperventilation.
 Diseases of the pericardium
Diseases of the pericardium
Constrictive pericarditis and cardiac tamponade are both associated with increased intracardiac and pulmonary vascular pressures, which are the likely cause of dyspnea in these conditions. To the extent that cardiac output is limited, at rest or with exercise, stimulation of metaboreceptors and chemoreceptors (if lactic acidosis develops) contribute as well.
Dyspnea with normal respiratory and cardiovascular systems
Mild to moderate anemia is associated with breathing discomfort during exercise. This is thought to be related to stimulation of metaboreceptors; oxygen saturation is normal in patients with anemia. The breathlessness associated with obesity is probably due to multiple mechanisms, including high cardiac output and impaired ventilatory pump function (decreased compliance of the chest wall). Cardiovascular deconditioning (poor fitness) is characterized by the early development of anaerobic metabolism and the stimulation of chemoreceptors and metaboreceptors.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree