Coronary Angiography
Coronary angiography remains the gold standard in defining coronary anatomy and graft patency. It is an invasive procedure and is associated with procedural risks including stroke, native vessel dissection, acute myocardial infarction (MI), ventricular arrhythmias, and puncture site morbidities such as hematomas and pseudoaneurysm formation. In addition, its deficiency in three-dimensional definition has led to the investigation of other noninvasive imaging techniques to define the overall coronary pathoanatomy. Initial attempts to utilize electron beam tomography and helical scan computed tomography (CT) were not encouraging due to motion artifacts, the need for prolonged breath holding, and image distortion due to metallic clips. Newer imaging techniques such as multidetector computed tomography (MDCT) have begun to revolutionize the diagnostic field.
Multidetector Computed Tomography
MDCT allows for fast data acquisition in a single breath hold of 25 to 30 seconds with varying slice thickness collimation, and Gantry rotation speeds following intravenous administration of 80 to 100 ml of nonionic contrast agent and a predetermined delay period to allow the contrast to reach the arterial circulation. Preprocedure beta-blockade allows for a heart rate of <60 beats per minute since faster hearts along with atrial fibrillation and
ectopic beats impair the quality of images obtained. Image reconstruction and manipulation is facilitated by electrocardiographic gated reconstruction algorithms.
Evaluation of Native Coronary Anatomy
Martuscelli and coworkers investigated the accuracy of MDCT in detection of significant (>50%) stenosis using a scanner equipped for 16 × 0.625 mm collimation and compared it with coronary angiography in 64 patients with suspected CAD. Eighty-four percent of the angiographic segments were evaluable. Severe calcification, cardiac motion artifacts, poor opacification, and blending of the segments with veins hindered the evaluation of the remaining segments. In the segments that were evaluable, namely, vessels >1.5 mm in diameter, MDCT had a sensitivity, specificity, positive predictive value, and negative predictive value of 89%, 98%, 90%, and 98%, respectively. MDCT had a 100% specificity and sensitivity in detecting total occlusion. Overall, MDCT detected 78% of stenoses detected by angiography. Cury et al. demonstrated an excellent correlation between 16-slice MDCT and angiography in quantifying the degree of stenosis. However, MDCT tended to overestimate the stenosis. The evaluation of the coronary anatomy and the results were significantly better than those obtained with the 4-slice MDCT. With the advent of 64-slice MDCT, Rubinshtein et al. analyzed its efficacy in the emergency room in evaluating patients with chest pain. They observed that emergency room MDCT had a high positive predictive value for diagnosis of acute coronary syndrome and a negative study predicted a low rate of major adverse cardiovascular event. In this study, only 4.6% of the coronary segments were of low image quality testifying to improvements in MDCT technology and also aided by the low calcium burden. These diagnostic tests have also been helpful in planning for minimally invasive revascularization procedures. During the procedures of minimally invasive direct coronary artery bypass (MIDCAB) or totally endoscopic coronary artery bypass (TECAB), the visualization of the target vessels is often limited and it is critical to identify the target vessel correctly and bypass it at the correct site. A common source of error is the bypassing of a large diagonal instead of the left anterior descending (LAD) artery during minimally invasive surgery. In addition, the target vessels could be buried under epicardial fat, covered by a myocardial bridge, run an intramural course, or heavily calcified. Newer generation MDCT scanners have been shown to identify these variations in coronary anatomy better than coronary angiography. These findings can dictate the type of surgery offered to the patients. Coronary calcification is obscured by the dye used in angiography. In an open procedure, such areas can be palpated and anastomosis can be performed in the noncalcified segments of the coronary vessels. However, tactile feedback is absent in the minimally invasive procedures. Regions of coronary vessels burdened by calcification as evidenced by MDCT can be avoided for anastomosis.
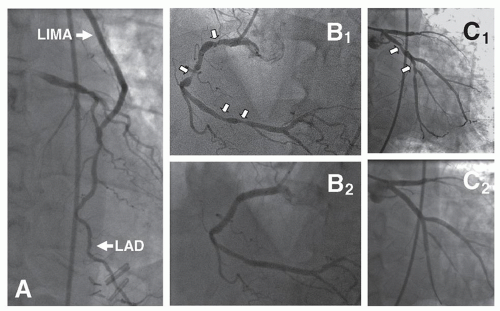
Evaluation of Graft Patency
Reoperative cardiac surgery is associated with increased morbidity and mortality and the potential to inadvertently injure the bypass grafts. MDCT allows for the accurate three-dimensional visualization of the course of the left internal mammary artery (LIMA) graft in relation to the midline, location of other conduits, and the degree of adherence of the right ventricle to the posterior table of the sternum. Unusual location of the grafts and their proximal anastomoses pose difficulties in evaluation by conventional angiography, especially in the absence of radio-opaque markers for the proximal anastomoses. Faster data acquisition allows a manageable breath hold for the patient allowing for visualization of the most proximal portions of the internal mammary artery grafts not seen in the early generation scanners. Martuscelli et al. analyzed 285 conduits in 96 patients with 16-slice MDCT and compared the results with those obtained by conventional angiography. The sensitivity of MDCT in diagnosing significant stenosis was 96%. Evaluation of graft patency and occlusion improved with the advent of 64-slice MDCT. The accuracy of 64-slice multislice CT for graft occlusion and stenosis is given in
Table 51.1. A recent analysis suggests that the sensitivity and specificity for graft occlusion approach 100% across the studies, with only two cases of missed occlusions in bypass grafts, which were not visualized on MDCT. There are currently no reports of false-positive occlusion. When diagnosing bypass graft stenosis, sensitivity ranged from 75% to 100%. Missed stenoses at distal anastomoses due partly to calcified wall plaque and membranous-like stenoses accounted for falsenegative results. The specificity for diagnosis of stenosis of bypass grafts ranges from 89.3% to 100%. Poor opacification combined with small vessel size, vessel kinking, and surgical clip artifact account for false-positive results. The results from these eight studies of 1,169 coronary artery bypass grafts are similar to those obtained by coronary angiography. Several studies have reported that grafts not visualized on coronary angiography were visualized on MDCT, thus, providing important additional clinical information.
However, assessment of native coronary arteries is impaired in the presence of atherosclerosis, calcification, and small diameter vessels. In addition, MDCT does not provide the flow characteristics of either the grafts or the distal run off. Arrhythmias, metallic clips on the side branches of the grafts, and higher heart rates continue to hinder adequate evaluation of the bypass grafts. Improved temporal and spatial resolution of the 64-slice CT scanner overcomes the artifacts caused by metal clips. Evaluation of in-stent stenosis by MDCT is difficult. Coronary stents are usually 2.5 to 4 mm in diameter. Blooming artifacts are produced by the metal in both the bare metal and drug-eluting stents. Cardiac motion compounds the problem. Partial volume effects lead to decreased visibility of the stent lumen, underestimates the luminal diameter, and overestimates
the outer diameter. Inside the lumen of the stent, there is an increase in the attenuation that can be minimized by utilizing submillimeter collimation and a sharp reconstruction kernel. With improving technological areas, the larger diameter stents in the left main coronary artery and the proximal coronary vasculature can be analyzed for evidence of decreased luminal diameter due to intimal hyperplasia. The native coronary vasculature in the immediate vicinity of the stent is difficult to evaluate for stenosis due to beaming artifacts. In addition, beam hardening produces dark areas adjacent to the clips stimulating stenosis especially at the anastomotic points.
MDCT can be effectively used as a one-stop test to evaluate the different causes of chest pain following CABG. Dual source and 256-slice scanning allow for fast data acquisition, may further simplify the test, improve diagnostic accuracy, and eliminate the current limitations imposed by rapid hearts rates. MR coronary angiography is being evaluated to analyze its potential as a noninvasive diagnostic tool. The summary statement released by the American Heart Association in collaboration with other councils has recommended that neither coronary artery CTA nor MRA should be used to screen for CAD in patients who have no signs or symptoms of CAD (Class III, level of evidence C). The potential benefit of noninvasive coronary angiography is likely to be greatest and is reasonable for symptomatic patients who are at intermediate risk for CAD after initial risk stratification including patients with equivocal stress-test results (Class IIa, level of evidence B). Concerns regarding radiation dose limit the use of coronary CTA in hig-hrisk patients who have a very low pretest likelihood of coronary stenoses; they are likely to require intervention and invasive catheter angiography for definitive evaluation; thus, CTA is not recommended for those individuals (Class III, level of evidence C). Pronounced coronary calcification may negatively impact interpretability and accuracy of coronary CTA and thus, the usefulness of CTA is uncertain in these individuals (Class IIb, level of evidence B).”