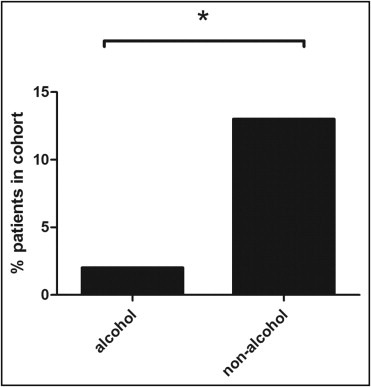
There are conflicting data as to the prevalence of coronary artery disease (CAD) in patients with end-stage liver disease (ESLD) being assessed for liver transplantation (LT). The aims of this study were to compare the prevalence of CAD in patients with alcohol-related versus non-alcohol-related ESLD and to assess the diagnostic utility of dobutamine stress echocardiography (DSE) in predicting angiographically important CAD. Consecutive patients with ESLD being assessed for LT (n = 420, mean age 56 ± 8 years) were identified and divided into groups of those with alcohol-related ESLD (n = 125) and non-alcohol-related ESLD (n = 295). Demographic characteristics, CAD risk factors, results of DSE, and coronary angiographic characteristics were recorded. There were no significant differences in age or CAD risk factors between groups. The incidence of severe CAD (>70% diameter stenosis) was 2% in the alcohol-related ESLD group and 13% in the non-alcohol-related ESLD group (p <0.005). In the 2 groups, the presence of ≥1 CAD risk factor was associated with significant CAD (p <0.05 for all). Absence of cardiac risk factors was highly predictive in ruling out angiographically significant disease (negative predictive value 100% for alcohol-related ESLD and 97% for non-alcohol-related ESLD). DSE was performed in 205 patients. In the 2 groups, DSE had poor predictive value for diagnosing significant CAD but was useful in ruling out patients without significant disease (negative predictive value 89% for alcohol-related ESLD and 80% for non-alcohol-related ESLD). In conclusion, there was a significantly lower prevalence of severe CAD in patients with alcohol-related ESLD. These findings suggest that invasive coronary angiography may not be necessary in this subgroup, particularly in the absence of CAD risk factors and negative results on DSE.
The prevalence of coronary artery disease (CAD) in patients with end-stage liver disease (ESLD) is unclear. Early postmortem studies reported a low incidence of myocardial infarction, while later studies, which assessed CAD using clinical, stress echocardiographic, coronary calcification, and/or coronary angiographic parameters in patients with ESLD being considered for liver transplantation (LT), reported rates varying from 2.5% to 38%. Moreover, it is not known whether the cause of ESLD influences the likelihood of severe CAD. In particular, the relation between excess alcohol consumption and CAD is controversial, with some postmortem and coronary angiographic data suggesting that excess alcohol consumption may be protective and others studies using clinical surrogates of CAD demonstrating that patients with alcohol-related ESLD are more likely to have significant CAD. In the first year after LT, CAD is the major cause of morbidity and mortality, accounting for up to 70% of major adverse clinical events, and over the longer term remains the leading cause of non-graft-related death in this population. It is therefore imperative that appropriate cardiac screening before LT be undertaken, and at many institutions, all patients being considered for LT undergo invasive coronary angiography (CA). We hypothesized that patients with alcohol-related ESLD would have a lower prevalence of significant CAD compared to patients with non-alcohol-related ESLD. The aim of this study was to assess the CAD risk profile and coronary angiographic characteristics of patients being assessed for LT. We also aimed to determine the diagnostic utility of dobutamine stress echocardiography (DSE) in predicting angiographically significant CAD.
Methods
We identified 420 consecutive patients with ESLD who were referred for cardiac catheterization as part of their pre-LT evaluation from January 2000 to March 2010. Patients were classified according to the cause of ESLD, obtained from chart review. Patients were classified as having alcohol-related ESLD if they had histories of consumption of >80 g of ethanol per day over many years. Patients with viral-related ESLD were classified on the basis of abnormal serologic results. Patients who were classified as having both alcohol-related and viral-related ESLD were considered part of the alcohol-related group. Demographic information and risk factors were collected retrospectively by chart review. Coronary risk factors included hypertension (defined as either systolic blood pressure at evaluation >140 mm Hg and/or diastolic blood pressure >90 mm Hg and/or the use of antihypertensive medication), diabetes mellitus (defined as taking insulin or a hypoglycemic agent), current or previous smoker, hyperlipidemia (defined as a total cholesterol >240 mg/dl and/or taking a lipid-modifying agent), and family history of early coronary heart disease.
Angiographic analysis was performed by an interventional cardiologist blinded to patients’ data. CAD was classified as normal (no angiographically apparent CAD), mild (<30% stenosis in all major epicardial coronary arteries), moderate (30% to 70% stenosis in all major epicardial coronary artery), or severe (>70% stenosis in all major epicardial coronary arteries). Further angiographic analysis was performed by assigning a Gensini score to each patient.
DSE was performed on 204 of the 420 patients, as part of their pre-LT assessment protocol. The decision to proceed with DSE was at the discretion of the referring physician and was performed according to a previously described protocol. The results of DSE were obtained retrospectively from chart review and classified as normal (no induced wall motion abnormality) or abnormal (induced wall motion abnormality) with stress.
Statistical analysis was performed using GraphPad Prism 5 (GraphPad Software, San Diego, California). Student’s t test was used to compare continuous variables. The chi-square test for proportions was used to detect differences between groups of categorical variables and to detect trends between the number of cardiac risk factors and the presence or severity of CAD. The chi-square test for trend was used to detect differences between alcohol-related ESLD and non-alcohol-related ESLD groups across a range of CAD severity. Variables were entered into a multivariate logistic analysis to determine the effect of alcohol status as an independent predictor of angiographically determined CAD. A p value <0.05 was considered significant.
Results
Four hundred twenty consecutive patients being evaluated for LT at our institution were included in this study. Baseline patient characteristics are listed in Table 1 . Most patients were middle-aged men. The causes of ESLD were predominantly viral (42%), alcohol related (19%), and cryptogenic (17%). In all patients, there was a high prevalence of CAD risk factors and a high prevalence of CAD, with 29% of all patients having angiographically apparent disease ( Table 1 ).
| Variable | Value |
|---|---|
| Age (years) | 56 ± 8 |
| Men/women | 279/141 |
| Cause of ESLD | |
| Alcohol | 81 (19%) |
| Viral | 175 (42%) |
| Alcohol and viral | 44 (10%) |
| Cryptogenic | 73 (17%) |
| Nonalcoholic steatohepatitis | 24 (6%) |
| Other | 23 (6%) |
| Atherosclerotic risk factors | |
| Hypertension ⁎ | 161 (38%) |
| Diabetes mellitus † | 120 (29%) |
| Current or previous smoker | 150 (36%) |
| Hypercholesterolemia ‡ | 112 (27%) |
| Family history of premature CAD | 65 (15%) |
| Severity of CAD § | |
| Normal | 297 (71%) |
| Minor | 48 (11%) |
| Moderate | 35 (8%) |
| Severe | 40 (10%) |
⁎ Systolic blood pressure >140 mm Hg or diastolic blood pressure >90 mm Hg and/or the use of antihypertensive medication.
† Taking insulin or a hypoglycemic agent.
‡ Total cholesterol >240 mg/dl and/or taking a lipid-modifying agent.
§ Minor, moderate, and severe CAD defined as <30% stenosis, 30% to 70% stenosis, and >70% stenosis, respectively, in any major epicardial coronary artery.
When patients with alcohol-related ESLD were compared to those with non-alcohol-related ESLD, a significantly higher proportion of patients in the non-alcohol-related group had angiographically defined severe coronary disease (2% in the alcohol-related group vs 13% in the non-alcohol-related group, p <0.01; Figure 1 ) and a statistically significant trend toward more severe CAD ( Table 2 ) . Also, patients with alcohol-related ESLD had significantly lower Gensini scores (mean 1.5 ± 0.6) compared to those with non-alcohol-related ESLD (mean 4.2 ± 0.8) (p <0.05). These groups were otherwise comparable with respect to age and the type and number of CAD risk factors, although there was a preponderance of men in the alcohol and alcohol-viral subgroups ( Table 2 ). When all variables were entered into a multivariate logistic analysis, hyperlipidemia (β = 0.29, p <0.001), alcohol status (β = −0.20, p <0.001), age (β = 0.12, p <0.05), hypertension (β = 0.11, p <0.05), and diabetes (β = 0.10, p <0.05) were found to be significant independent predictors of CAD.
| Variable | Alcohol-Related ESLD | Non-Alcohol-Related ESLD | p Value |
|---|---|---|---|
| Age (years) | 56 ± 7 | 56 ± 8 | 0.44 |
| Men/women | 98/27 | 175/120 | <0.01 |
| Coronary risk factors | |||
| Hypertension ⁎ | 55/125 (44%) | 106/295 (36%) | 0.12 |
| Diabetes mellitus † | 31/125 (25%) | 89/295 (30%) | 0.52 |
| Current or previous smoker | 48/125 (38%) | 102/295 (35%) | 0.45 |
| Hypercholesterolemia ‡ | 34/125 (27%) | 78/295 (26%) | 0.87 |
| Family history of premature CAD | 23/125 (18%) | 42/295 (14%) | 0.28 |
| >1 CAD risk factor | 61/125 (49%) | 155/295 (52%) | 0.48 |
| Severity of CAD § | |||
| Normal | 101/125 (81%) | 196/295 (66%) ∥ | |
| Minor | 14/125 (11%) | 34/295 (12%) ∥ | |
| Moderate | 7/125 (6%) | 28/295 (9%) ∥ | |
| Severe | 3/125 (2%) | 37/295 (13%) ∥ | |
| Gensini score | 1.5 ± 0.6 | 4.2 ± 0.8 | <0.05 |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


