N-terminal prohormone brain natriuretic peptide (NT-proBNP) is known to be valuable as a prognostic marker for the management of heart failure. This study aimed to assess the serial changes of serum NT-proBNP levels as a prognostic factor for outcomes of pediatric dilated cardiomyopathy (DC). A retrospective study reviewed echocardiographic measurements and serum NT-proBNP levels obtained at the time of diagnosis, 3 and 6 months after diagnosis, and at the last follow-up in 68 children with DC. They were classified into 3 groups according to the last follow-up of the left ventricular (LV) function: group I (n = 37) with LV fractional shortening (FS) ≥25%, group II (n = 15) with 10% ≤ LVFS < 25%, and group III (n = 16) with LVFS <10% or cardiac death. The median age at diagnosis was 30 months and median duration of follow-up was 45 months (range 8 to 108 months). The origin of DC varied. Serial serum NT-proBNP levels showed statistically significant differences among the 3 groups. Although initial levels of serum NT-proBNP at diagnosis were not different from each other, group III maintained a higher NT-proBNP level throughout the duration of the follow-up. On multivariate Cox analysis, only the NT-proBNP level at 3 months was a significant predictor of an adverse outcome (hazard ratio 2.012, p = 0.028). The percent changes of NT-proBNP from diagnosis were not significant. Patients with DC with a serum NT-proBNP level ≥681 pg/ml at 3 months after diagnosis showed an increased risk of severe LV dysfunction or cardiac death (p <0.001, area under the curve = 0.846). In conclusion, the level of NT-proBNP in serum at 3 months after diagnosis could predict an adverse outcome in pediatric DC and could be used as a guide for long-term treatment plans.
We wondered whether the serum N-terminal prohormone brain natriuretic peptide (NT-proBNP) level at any point after diagnosis or whether its change over time can predict adverse outcomes in children with dilated cardiomyopathy (DC). To address this, the present study sought to (1) assess serial serum NT-proBNP levels and echocardiographic variables and their correlation in children with DC, (2) investigate whether serial serum NT-proBNP levels or percent change in levels of serum NT-proBNP can predict adverse outcomes in the patient group, and (3) obtain a cut-off value for the most valuable prognostic marker with which adverse outcomes were predicted.
Methods
We retrospectively reviewed the records of pediatric patients <19 years of age who were diagnosed with DC from March 2004, when their serum NT-proBNP levels became available, to December 2011, at the Samsung Medical Center. DC was diagnosed based on 2006 definitions and classification of cardiomyopathies by the American Heart Association. Sixty-eight patients were enrolled in this study according to the inclusion criteria: (1) pediatric DC patients aged <19 years, (2) availability of complete data for serial measurements of NT-proBNP, and (3) a follow-up duration >6 months. We excluded patients who had congestive heart failure with renal insufficiency causing inappropriate elevation of serum NT-proBNP levels. The origin of DC in these enrolled patients was various and included idiopathic disease, myocarditis, tachycardia, familial disease, mitochondrial disease, and anthracycline-induced cardiomyopathy. The patients were all managed for heart failure according to a management protocol over at least 6 months. All patients received individually optimized medication of diuretics, β blockers, angiotensin-converting enzyme inhibitors, and digoxin at our center. Study end points were cardiac death or last outpatient follow-up.
The study was approved by the Samsung Medical Center Institutional Review Board.
NT-proBNP was measured in serum using an immunochemiluminescence immunoassay method (Elecsys 2010; Roche Diagnostics, Indianapolis, Indiana). The assay uses polyclonal antibodies for human NT-proBNP and has a measurement range of 5 to 35,000 pg/ml. All measurements were performed in the laboratory at the Samsung Medical Center. Serum NT-proBNP levels at diagnosis of DC, 3 and 6 months after diagnosis, and at the last follow-up were obtained and reviewed. The percent change in each serum level from NT-proBNP at diagnosis was calculated as [(NT-proBNP (3 months, 6 months, and final follow-up)−NT-proBNP at diagnosis) × 100]/NT-proBNP at diagnosis.
Echocardiography was performed using a Sequoia 512 apparatus (Acuson, Mountain View, California). In the echocardiographic data, we investigated left ventricular (LV) diastolic dimension, LV systolic dimension, LV ejection fraction (EF), and LV fractional shortening (FS) at diagnosis, 3 and 6 months from diagnosis, and at the last follow-up. M-mode tracing for LV diastolic dimension, LV systolic dimension, LVEF, and LVFS was measured in the parasternal long-axis view. Body surface area–normalized z scores for LV systolic dimension and LV diastolic dimension were then calculated. Although extrapolation of EF from linear LV minor-axis diameters can be inaccurate because of the geometric assumptions, all patients in this study showed acceptable ventricular geometry supporting the linear relation between LVFS and LVEF based on volumetric measurements by Simpson method. Because of incomplete data of LVEF, LVFS was used instead of LVEF.
This study was classified into 3 groups according to the outcomes at the last follow-up: LVFS ≥25% (group I), 10% ≤ LVFS <25% (group II), and LVFS <10% or cardiac death (group III).
We defined that adverse outcomes were severe systolic ventricular dysfunction of LVFS <10% or cardiac death. Cardiac death was defined as when cardiac pump function is not able to maintain vital organ perfusion resulting in mortality or heart transplantation or sudden arrhythmic death.
Continuous variables are expressed as the median (range) value. The 3 groups were compared using a 1-way analysis of variance or Kruskal-Wallis test. The serum NT-proBNP comparisons were first computed using raw values and then verified with log-transformed values (log NT-proBNP). Pearson test was used to determine correlation between serum NT-proBNP levels and echocardiographic variables. The serial change of the serum NT-proBNP level was analyzed using a repeated measures analysis of variance. The correlation between the levels of the peptide or percent change of the level and the adverse outcome was analyzed by Cox proportional hazard regression. Receiver operating characteristic curves were generated to show the optimal value of the predictor of adverse outcomes. Time-to-occurrence adverse outcomes were used for creation of a Kaplan-Meier curve. p <0.05 was considered to indicate statistical significance.
Results
Baseline characteristics of the patients are listed in Table 1 . Age at diagnosis among the 3 groups was significantly different (p = 0.005). Group III patients were older than those in the other groups at diagnosis. Eight (11%) of 68 patients showed cardiac death (4 deaths and 4 heart transplantations). There were no cases of sudden arrhythmic death. Adverse outcomes included 8 severe LV systolic dysfunctions, 4 deaths, and 4 heart transplantations. The origins of patients with DC were idiopathic disease, myocarditis, tachycardia, familial disease, mitochondrial disease, and anthracycline-induced cardiomyopathy. There were no significant differences of origin among the 3 groups.
| Variable | LVFS ≥25% (n = 37) | 10% ≤ LVFS < 25% (n = 15) | LVFS <10% or Cardiac Death (n = 16) | p |
|---|---|---|---|---|
| Male (%) | 14 (38) | 9 (60) | 10 (63) | 0.155 |
| Age (mo) | 85 (15 to 264) ∗ | 105 (14 to 264) ∗ | 169 (19 to 240) ∗ | 0.105 |
| Age at diagnosis (mo) | 11 (1 to 204) ∗ | 62 (1 to 192) ∗ | 136 (2 to 204) ∗ | 0.005 |
| Cause of DC, n (%) | 0.843 | |||
| Idiopathic | 24 (65) | 11 (73) | 12 (75) | |
| Myocarditis | 6 (16) | 0 | 1 (6) | |
| Tachycardia | 3 (8) | 1 (7) | 1 (6) | |
| Familial | 1 (3) | 0 | 0 | |
| Mitochondrial | 2 (5) | 2 (13) | 1 (6) | |
| Anthracycline-induced | 1 (3) | 1 (7) | 1 (6) | |
| Length of follow-up (mo) | 52 (12 to 108) ∗ | 34 (12 to 96) ∗ | 29 (8 to 96) ∗ | 0.035 |
| Cardiac death | 0 | 0 | 8 (50) | <0.001 |
| Died | 4 | |||
| Heart transplantation | 4 |
A detailed comparison of serum NT-proBNP levels and echocardiographic variables among the groups is listed in Table 2 . The initial serum NT-proBNP level and log NT-proBNP did not differ among the 3 groups. Group I patients had a lower level of serum NT-proBNP and log NT-proBNP than patients from the other 2 groups at 3 and 6 months and final follow-up. The decrease in serum NT-proBNP level after diagnosis in group I patients was significantly larger than that in the other 2 groups at 3 and 6 months and final follow-up.
| Variable | LVFS ≥25% (n = 37) | 10% ≤ LVFS < 25% (n = 15) | LVFS <10% or Cardiac Death (n = 16) | p |
|---|---|---|---|---|
| NT-proBNP (pg/ml) | ||||
| At diagnosis | 8,016 (48 to 35,000) | 12,927 (644 to 35,000) | 9,379 (1,195 to 35,000) | 0.616 |
| At 3 mo | 312 (50 to 3,637) | 2,197 (82 to 22,677) | 4,274 (692 to 35,000) | <0.001 |
| At 6 mo | 208 (28 to 1,571) | 1,526 (108 to 19,220) | 2,059 (86 to 35,000) | <0.001 |
| At final | 70 (18 to 1,086) | 259 (49 to 35,000) | 2,068 (76 to 35,000) | 0.001 |
| log NT-proBNP | ||||
| At diagnosis | 8.98 (3.89 to 10.46) | 9.46 (6.47 to 10.46) | 9.14 (7.09 to 10.46) | 0.919 |
| At 3 mo | 5.74 (3.91 to 8.20) | 7.69 (4.41 to 10.03) | 8.36 (6.54 to 10.46) | <0.001 |
| At 6 mo | 5.33 (3.33 to 7.36) | 7.30 (4.68 to 9.86) | 7.49 (4.45 to 10.46) | <0.001 |
| At final | 4.24 (2.89 to 6.99) | 5.55 (3.91 to 10.46) | 7.61 (4.33 to 10.46) | <0.001 |
| Percent change of NT-proBNP | ||||
| By 3 mo | −96 (−99 to 141) | −76 (−99 to 30) | −43 (−95 to 91) | 0.012 |
| By 6 mo | −98 (−99 to 45) | −84 (−98 to −9) | −53 (−99 to 228) | 0.001 |
| By final | −99 (−99 to 18) | −96 (−99 to 97) | −58 (−98 to 44) | 0.001 |
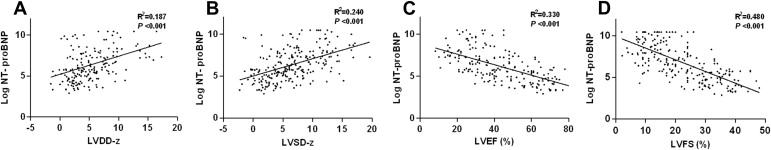
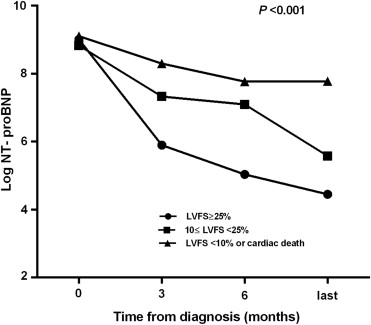
Group I patients had smaller LV diastolic diameters, as determined by echocardiography and relative to body surface area z score (LV diastolic dimension-z), and smaller LV systolic diameters relative to body surface area z score (LV systolic dimension-z) than the patients in the other 2 groups at initial diagnosis, 3 and 6 months, and final follow-up. Group I patients had a greater level of LVFS than the patients in the other 2 groups at initial diagnosis and 3 and 6 months after diagnosis ( Table 3 ). Log NT-proBNP levels at any point were correlated with LV diastolic dimension-z, LV systolic dimension-z, and were negatively correlated with LVEF and LVFS ( Figure 1 ). Serial log NT-proBNP levels decreased significantly through each follow-up point (within-subject effects; Figure 2 ). The 3 groups displayed different patterns of change of log NT-proBNP levels (between-subject effects).
| Variable | LVFS ≥25% (n = 37) | 10% ≤ LVFS < 25% (n = 15) | LVFS <10% or Cardiac Death (n = 16) | p |
|---|---|---|---|---|
| LVDD-z | ||||
| At diagnosis | 4.8 (1.3 to 12.3) | 4.8 (2.5 to 10.8) | 7.9 (−0.9 to 14.2) | 0.026 |
| At 3 mo | 3.6 (−0.7 to 9.7) | 5.5 (1.0 to 8.9) | 7.7 (1.2 to 14.5) | 0.005 |
| At 6 mo | 2.4 (−1.5 to 11.2) | 5.5 (2.2 to 13.2) | 9.1 (0.2 to 16.4) | <0.001 |
| At final | 2.9 (−1.2 to 8.0) | 4.9 (1.9 to 14.6) | 7.8 (−1.1 to 17.3) | <0.001 |
| LVSD-z | ||||
| At diagnosis | 7.6 (2.5 to 13.1) | 7.7 (4.0 to 16.5) | 11.4 (1.5 to 16.2) | 0.011 |
| At 3 mo | 4.4 (−0.3 to 10.1) | 7.1 (0.6 to 12.1) | 9.7 (−1.2 to 16.8) | 0.001 |
| At 6 mo | 2.6 (−1.8 to 9.3) | 6.6 (3.1 to 17.1) | 11.7 (0.1 to 16.5) | <0.001 |
| At final | 2.2 (−2.2 to 8.1) | 5.5 (1.6 to 19.6) | 11.4 (−1.6 to 16.8) | <0.001 |
| LVFS (%) | ||||
| At diagnosis | 13.1 (2.0 to 24.0) | 15.5 (7.0 to 26.0) | 10.8 (3.8 to 16.9) | 0.043 |
| At 3 mo | 26.0 (7.6 to 42.0) | 22.0 (13.0 to 37.0) | 12.4 (6.5 to 32.0) | 0.006 |
| At 6 mo | 32.5 (11.0 to 45.0) | 22.5 (13.0 to 30.0) | 15.1 (4.1 to 20.0) | <0.001 |
| At final | 35.0 (26.0 to 48.0) | 22.0 (17 to 24.0) | 9.0 (5.6 to 9.8) | <0.001 |
The results of univariate and multivariate Cox analyses to predict adverse outcomes are listed in Table 4 . In the univariate analysis, gender, cause of DC, log NT-proBNP at diagnosis, and percent change at 3 months after diagnosis were not significant for predicting adverse outcomes. Age at diagnosis, log NT-proBNP at 3 and 6 months after diagnosis, and the percent change of the 6-month serum NT-proBNP value after diagnosis were significant predictors of adverse outcomes. We included the following variables in the multivariate analysis: age at diagnosis, log NT-proBNP at 3 and 6 months after diagnosis, and the percent changes in the 3- and 6-month serum NT-proBNP values from those at diagnosis. Multivariate analysis revealed that log NT-proBNP at 3 months after diagnosis and age at diagnosis significantly predicted adverse outcomes. The hazard ratio of log NT-proBNP at 3 months after diagnosis was 2.078 (95% confidence interval; 1.123 to 3.845, p = 0.020), but that of age at diagnosis was 1.010.
| Variable | Univariate | Multivariate | ||||
|---|---|---|---|---|---|---|
| Hazard Ratio | 95% CI | p | Hazard Ratio | 95% CI | p | |
| Age at diagnosis | 1.011 | 1.003 to 1.018 | 0.004 | 1.010 | 1.001 to 1.020 | 0.027 |
| Log NT-proBNP | ||||||
| At diagnosis | 1.131 | 0.786 to 1.630 | 0.507 | — | — | — |
| At 3 mo | 1.968 | 1.388 to 2.791 | <0.001 | 2.078 | 1.123 to 3.845 | 0.020 |
| At 6 mo | 1.615 | 1.222 to 2.135 | 0.001 | 1.011 | 0.626 to 1.632 | 0.964 |
| Percent change of NT-proBNP | ||||||
| By 3 mo | 1.006 | 0.999 to 1.013 | 0.101 | 0.990 | 0.973 to 1.007 | 0.257 |
| By 6 mo | 1.007 | 1.002 to 1.013 | 0.006 | 1.006 | 0.996 to 1.015 | 0.239 |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


