Fig. 5.1
Diagrammatic illustration showing access to the right pleural cavity with the retraction of the superior vena cava anteriorly SVC Superior vena cava; IJV Internal jugular vein; IA Innominate artery; RA Right atrium
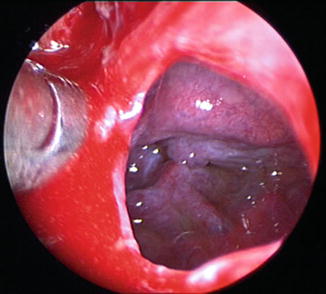
Fig. 5.2
Pleurotomy made through cervical mediastino-thoracoscopy
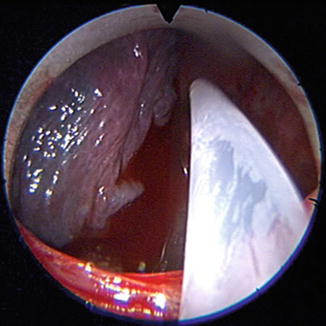
Fig. 5.3
Operative arrangement of the thoracoscope being inserted into the mediastinoscope
Once all interventions have been completed, a 28 French chest drain is inserted into the pleural space via the mediastinoscope and caudally tunnelled to the cervical incision through the pre-sternal tissues where it is brought out. The mediastinoscopy wound is closed and the drain placed on 5 kilopascals of suction.
5.6 Results
The first report using CMT was published by Deslauriers et al. (1976) [2]. In their paper, 275 of 1,100 patients underwent CMT over a period of 6 years. This cohort was divided into three groups: those who had a final diagnosis of bronchogenic carcinoma (153 patients), benign pulmonary disease (102 patients) or pleural disease (20 patients). The success rates in obtaining histopathological diagnoses were poor in this study: 102 of 153 (78 %) of malignant lesions were identified, and 92 out of 102 (91 %) of benign lesions were characterised. Since this report, there have been three further studies reporting on this approach.
Chamberlain et al. (2008) reported the use of video-assisted cervical mediastino-thoracoscopy in 15 patients (13 male) with a median age of 57 years [3]. All patients in this group had disease highly suspicious for malignant pleural mesothelioma and were candidates suitable for radical surgical resection by way of extended pleurectomy and decortication. The majority (13 patients) had right-sided disease. Simultaneously, 26 patients underwent conventional staged preoperative workup. The overall success rate of the operative technique was concluded to be 67 % (10 of 15 patients). The authors were unable to perform the procedure in three patients with right-sided disease owing to excessive mediastinal fat precluding adequate views of the pleura for safe progression in one patient; in the other two cases, bulky mediastinal pleural tumour prevented entry to the hemithorax. In both patients with left-sided disease, the procedure proved unsuccessful due to thickened pleura surrounding the aortic arch. In the 10 successful cases, mean operative time was documented to be 71 min (range: 65–90 min), and hospital stay was on average 4 days (range: 3–7 days).
The authors reported two post-operative complications: one patient, who had left-sided disease, suffered a transient left recurrent laryngeal nerve palsy, and in another patient a prolonged air leak was documented on the background of emphysematous lung disease.
In addition to the above results, the authors were able to demonstrate that the time taken to have definitive radical surgery was reduced by approximately 2 months in patients who had a CMT (28 ± 17 days versus 87 ± 56 days; p < 0.001) when compared with patients referred following a VATS biopsy elsewhere who required a separate conventional mediastinoscopy for further staging.
Fowkes et al. (2009) published their experience with cervical mediastino-thoracoscopy in 15 patients over a 3-year period [4]. The operation was performed for the diagnosis of pleural effusion in seven patients, staging of mesothelioma in seven patients and the staging of lung cancer in one patient. Thoracoscopy was carried out on the left side in six patients and on the right side in eight patients and bilaterally in one patient. The operative success was reported to be 93 % (14 of 15 patients). The one failed procedure had dense pleural adhesions which made access via pleurotomy impossible, and the subsequent VATS approach failed for the same reason and an open biopsy via thoracotomy was expedited. The mean operative time for unilateral procedures was 64 min (range: 24–142 min) and 62 min for bilateral procedures. There were three reported post-operative complications: in one patient, acute lung injury and renal failure following talc pleurodesis incurred a 22-day admission, and two patients who underwent left CMT developed a left recurrent laryngeal nerve palsy. The mean length of post-operative hospital stay was 2.4 days (excluding the patient who had a 22-day admission).
The most recent article by Liberman et al. (2012) originating from Quebec, Canada, describes the use of the CMT in a single patient with bilateral pleural effusions [5]. The operative technique used in this patient was modified in that a flexible gastroscope was passed through the mediastinoscope to allow satisfactory visualisation of the whole pleural cavity and biopsies of peripheral lung tissue that are more difficult to reach with the rigid thoracoscope. This procedure was completed in 48 min, and the patient was discharged from the thoracic surgical department on post-operative day four with no documented post-operative complications.
5.7 Complications
The procedure-specific complications are outlined in Table 5.1 and are based on the evidence of the three studies performed to date analysing a total cohort of 31 patients [3–5]. The most frequently documented complication is that of a left recurrent laryngeal nerve palsy when gaining access to the left pleural cavity. The incidence of vocal cord paralysis following video-assisted mediastinoscopy has been reported to be less than 1 % [6]; however, it has been documented to lie in the region of 6 % [7] in a study where all patients were subjected to preoperative and post-operative indirect laryngoscopy and is most likely the result of a traction injury to the nerve. It is imperative that patients are consented with a view to the above complications and that informed consent is obtained for a video-assisted thoracoscopic surgery approach or open diagnostic anterior mediastinotomy via the third intercostal space in the event of a failed cervical approach.
Table 5.1
The recognised complications following cervical mediastino-thoracoscopy as evidenced from 31 patients
Complication | Number (%) |
|---|---|
Left recurrent laryngeal nerve palsy | 3 (10 %) |
Prolonged air leak | 1 (3 %) |
Acute lung injury | 1 (3 %) |
Renal failure | 1 (3 %) |
5.8 Conclusions
The use of CMT as a surgical approach to the mediastinum and pleural cavities has been available for over three decades, but only recently used owing to advancements and the widespread application of video-assisted thoracoscopic surgical techniques. Its main uses have been reported in pulmonary and pleural malignancies.
5.8.1 Pulmonary Malignancy
The management of patients with lung cancer potentially amenable to surgical input may be improved by the introduction of CMT. Such an approach could be applied to patients with peripheral lung tumours (primary or metastatic) that are highly suspicious for neoplasia given the history and imaging used. This would allow a tissue diagnosis and also assess the degree of nodal involvement by mediastinal lymph node dissection in stations 2L, 2R, 4L, 4R and 7 to determine the most appropriate management plan.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


