Fig. 6.1
Patient position. The right thorax is prepared for potential conversion to video-thoracoscopy
6.2.2 First Step
The first step is similar to a conventional cervical video-assisted mediastinoscopy. Patients are positioned in a hybrid dorsal and lateral position with the neck in hyperextension (Fig. 6.1). As mentioned above, the patient’s position should allow the possibility of thoracoscopy in case of CITES failure.
A horizontal cervical incision (1–2 cm) is made just above the sternal manubrium. All tissues to the pretracheal fascia are dissected. Digital dissection is then performed in the pretracheal plane following the upper and lateral sides of the trachea (Fig. 6.2). The video-mediastinoscope is introduced as usual and used for the exploration of the mediastinum, for lymph node biopsies and for the opening of both mediastinal pleuras.


Fig. 6.2
Digital dissection of latero-tracheal space
6.2.3 Second Step
To create the mediastinal pleural windows, we proceed differently for each side. On the right side, digital dissection of the right mediastinal pleura under the level of the superior vena cava is initiated, creating a communication between the mediastinum and the right pleural cavity. Suction and dissection tools could be used to facilitate this step (Fig. 6.3). On the left side, the pleurotomy is performed using the same technique between the left common carotid and subclavian artery.
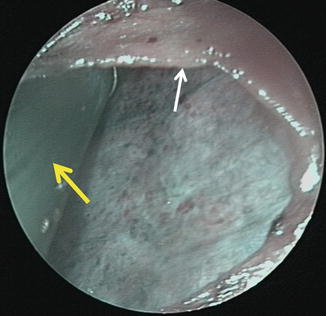
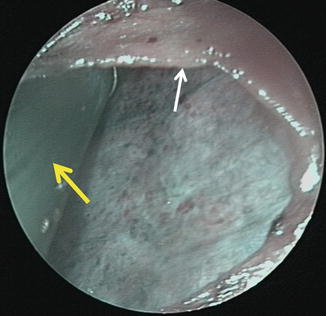
Fig. 6.3
Right pleural window. White arrow shows the borders of mediastinal pleura and yellow arrow the dissection tool used for window creation. Notice the right lung in the background of the figure
After mediastinal exploration and pleural window creation, the video-gastroscope is introduced first through the cervical incision to the latero-tracheal space and then into the pleural cavities through both pleurotomies (Fig. 6.4). In fatty patients, the use of a guide (small silicone chest tube) can be helpful to facilitate the introduction of the gastroscope into the pleural cavity.
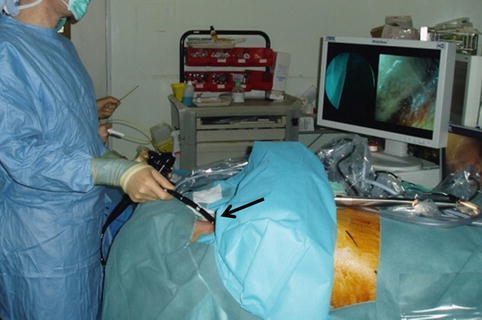
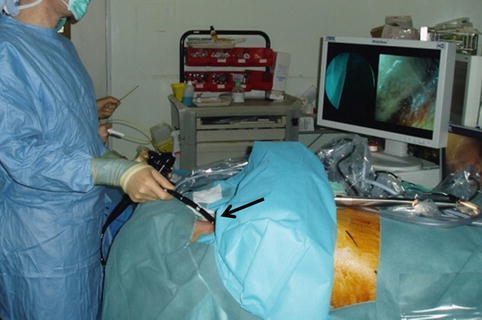
Fig. 6.4
Flexible gastroscope introduced through cervical incision (black arrow)
After this step of thoracic cavity exploration, large biopsies are taken on the targeted zones in both pleural cavities. To perform pleural biopsies, we use the endoscopic biopsy forceps introduced through the operative channels of the gastroscope (Fig. 6.5). Two forceps could be used simultaneously to obtain large pleural biopsies performing limited pleurectomies, if needed.


Fig. 6.5
Parietal pleural biopsies performed with endoscopic biopsy forceps. Arrow shows the tip of the biopsy forceps grasping the parietal pleura
The gastroscope has the capacity of wide rotation and navigation (180° rotation, anteroposterior and lateral movements). It represents an excellent tool to explore parietal and visceral pleura, the mediastinum and the diaphragm (phrenic nerve). Identification of the phrenic and sympathetic nerves bilaterally is also easily preformed.
If bilateral pleural exploration and biopsies are required, we perform the right-side exploration first. Before we move from one side to another, a chest tube is introduced through the cervical incision into the pleural window. Intrathoracic position of the chest tube is visually verified as well as the good ventilation of the operated lung (Fig. 6.6). The tube is exteriorised through the cervical incision (Fig. 6.7).

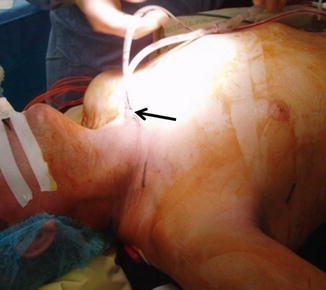

Fig. 6.6
Chest tube insertion into the pleural space
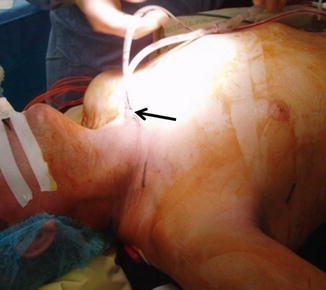
Fig. 6.7
Chest tube drainage exteriorised through cervical incision. Arrow shows the exteriorization of the chest tubes
6.3 Indications
1.
Cancer staging is the principal current indication of CITES. It takes a major place in cases of simultaneous mediastinal and pleural biopsies in lung cancer staging. It offers the possibility of mediastinal lymph node biopsies and bilateral exploration and biopsies of the parietal pleura. Other biopsies, such as lymph node biopsies in stations 5 and 6, can be performed using the rotation and navigation capacities of the gastroscope.
2.
Bilateral pleural biopsies and talc instillation in cases of bilateral pleural metastases with pleural effusion.
6.4 Contraindications
1.
Medical history of any disease that creates pleural adhesions or pleurodesis: previous thoracic surgery, pneumonia, empyema, etc.
2.
Limited pulmonary function in patients that cannot tolerate single-lung ventilation during the operation.
3.
Short and large neck: the access to the mediastinal pleura and the creation of pleural windows can be difficult with high risk of vascular and neurological complications.
4.
Proximal tumours or tumours invading the mediastinum: the risk of haemorrhage during the opening of the mediastinal pleuras is high.
6.5 Results
We used CITES approach for simultaneous exploration of the mediastinum and pleural cavity in lung cancer staging [21]. The original technique was successfully applied, and mediastinal lymph node and parietal pleural biopsies were successfully performed.
The mediastinal exploration allowed an excellent visualisation of the mediastinal structures. Mediastinal lymph nodes, 2R, 4R, 7 and 4L, were consistently identified and biopsies were easy to perform. The introduction of the video-gastroscope into the pleural cavities through the previously created mediastinal windows was not difficult.
At the end of the procedure, the small silicone chest tube was placed through both the cervical incision and the pleural window. The intrathoracic position of the tube was visually verified (Fig. 6.6). The tube was exteriorised through the cervical incision (Fig. 6.7).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


