The aim of this study was to investigate the relation between brain natriuretic peptide (BNP) levels and the detection rate of new documented atrial fibrillation (AF) after ischemic stroke. Consecutive patients with ischemic stroke prospectively enrolled within 24 hours of onset. Patients with AF on admission electrocardiography or with histories of AF were excluded. The plasma BNP level was measured on admission, and the factors associated with new documented AF were investigated by multivariate logistic regression analysis. Furthermore, the detection rates of AF according to BNP level were evaluated. A total of 584 patients were enrolled. AF was detected in 40 patients (new AF group; 6.8%). The median BNP level of the new AF group was significantly higher than for the non-AF group (186.6 pg/ml [interquartile range 68.7 to 386.3] vs 35.2 pg/ml [interquartile range 15.9 to 80.1], p <0.0001). The cut-off level, sensitivity, and specificity of BNP levels to distinguish the new AF group from the non-AF group were 65.0 pg/ml, 80%, and 70%, respectively. Multivariate logistic regression analysis demonstrated that National Institutes of Health Stroke Scale score >7 (odds ratio 3.4, 95% confidence interval 1.685 to 7.006, p = 0.0007) and a plasma BNP level >65.0 pg/ml (odds ratio 6.8, 95% confidence interval 2.975 to 15.359, p <0.0001) were independently associated with new AF. The detection rates of AF according to BNP level were as follows: 2% of patients with <50 pg/ml, 4% of those with 50 to <100 pg/ml, 12% of those with 100 to <200 pg/ml, 26% of those with 200 to <400 pg/ml, and 38% of those with ≥400 pg/ml. In conclusion, BNP levels can predict new AF in patients with acute ischemic stroke. Elevated BNP levels result in an increase in the frequency of detection of new AF.
Brain natriuretic peptide (BNP) is a 32–amino acid polypeptide containing a 17–amino acid ring structure that was isolated from porcine brain in 1988 and is a diuretic factor with vasodilator activity. BNP is primarily released from ventricular myocardium and has been shown to be useful in the assessment of patients with cardiac dysfunction. In addition, plasma BNP levels have also been shown to be elevated in patients with acute ischemic stroke, in particular those with atrial fibrillation (AF). Recently, several studies determined a BNP level threshold as a predictor of delayed AF after ischemic stroke or transient ischemic attack, but the sample sizes of these studies were small. No previous study has examined the association between the detection rate of new AF and BNP level. In the present study, we investigated the relation between elevated BNP levels and the detection rate of new AF during hospitalization in patients with acute ischemic stroke.
Methods
From March 2006 to August 2010, we prospectively enrolled consecutive patients with acute ischemic stroke within 24 hours of onset. Patients with AF on admission 12-lead electrocardiography (ECG) or with histories of AF were excluded. Patients with dialysis-dependent chronic renal failure were also excluded from the present study, because plasma BNP levels are increased in these patients. The plasma BNP level was measured on admission. This study complied with the Declaration of Helsinki with regard to investigations in humans, and the study protocol was approved by the ethics committee of Kawasaki Medical School Hospital.
Diagnosis of acute ischemic stroke was made by stroke neurologists and confirmed by computed tomography or magnetic resonance imaging. The following factors were assessed: age, gender, previous ischemic stroke, previous coronary artery disease, previous heart failure, vascular risk factors, treatment before ischemic stroke, stroke subtype, National Institutes of Health Stroke Scale (NIHSS) score on admission, and blood testing (serum creatinine and plasma BNP).
To identify the mechanism of cerebral infarction, we performed duplex carotid ultrasonography, ECG, transthoracic echocardiography, transcranial Doppler, magnetic resonance angiography, and/or computed tomographic angiography. Stroke subtype was classified according to the Trial of Org 10172 in Acute Stroke Treatment.
We also evaluated the following vascular risk factors: hypertension (defined as the use of antihypertensive agents, systolic blood pressure ≥140 mm Hg, or diastolic blood pressure ≥90 mm Hg before stroke onset or 2 weeks after stroke onset), diabetes mellitus (defined as the use of oral hypoglycemic agents or insulin, fasting blood glucose level ≥126 mg/dl, or glycosylated hemoglobin level ≥6.4%), hyperlipidemia (defined as the use of antihyperlipidemic agents or serum total cholesterol level ≥220 mg/dl), current smoking habit (defined as a history of smoking during the preceding 3 months), and AF (diagnosed by 12-lead ECG, continuous electrocardiographic monitoring, or 24-hour Holter ECG).
Baseline blood samples of all patients were taken on admission. We prospectively measured plasma BNP for all patients on admission. Samples were collected from a peripheral vein into tubes containing aprotinin and ethylenediamine tetraacetic acid, and the plasma was isolated and then stored at −80°C until analysis. The plasma BNP concentration was measured using a chemiluminescence enzyme immunoassay for human BNP (Shionogi & Company, Ltd., Osaka, Japan). Briefly, this assay uses 2 monoclonal antibodies against human BNP, 1 recognizing a carboxyl-terminal sequence and the other the ring structure of BNP, and measures BNP by sandwiching it between the 2 antibodies. BNP can be accurately quantified within 11 minutes. The normal value of BNP is ≤18.4 pg/ml in our hospital. The minimal detectable quantity of BNP is 3.9 pg/ml. The intra-assay coefficient of variation ranges from 1.6% to 3.6%, and the interassay coefficient of variation ranges from 1.3% to 4.5%. Investigators were not blinded to BNP results.
First, we investigated the detection rate of new AF, the method of identifying AF, and the interval to detection of AF during hospitalization. Second, we divided the patients into 2 groups according to the presence of AF: the new AF group, whose patients had newly documented AF during hospitalization, and the non-AF group. We compared the clinical characteristics, including BNP level, between the 2 groups using chi-square tests and Mann-Whitney U tests, and linear regression analysis was used to examine factors associated with plasma BNP level. The optimal cut-off points for each continuous variable to distinguish the new AF group from the non-AF group were determined from receiver-operating characteristic curves. Then, the factors with p values <0.10 on univariate analysis and the optimal level of plasma BNP were entered into a multivariate analysis to determine adjusted odds ratios. Finally, we evaluated the frequency of new AF detection for the following BNP levels: <50, 50 to <100, 100 to <200, 200 to <400, and ≥400 pg/ml. Data were statistically analyzed using StatView version 5 (SAS Institute Inc., Cary, North Carolina) and SPSS version 11 (SPSS Japan, Inc., Tokyo, Japan). Differences were considered statistically significant at p <0.05.
Results
During the study period, 844 patients were admitted to our hospital <24 hours after the onset of acute ischemic stroke. We excluded 260 patients with AF on admission ECG or with histories of AF or dialysis-dependent chronic renal failure. Finally, 584 patients were included in the present study (mean age 71.1 years, 209 women). The mean NIHSS score on admission was 7.1 ± 7.4.
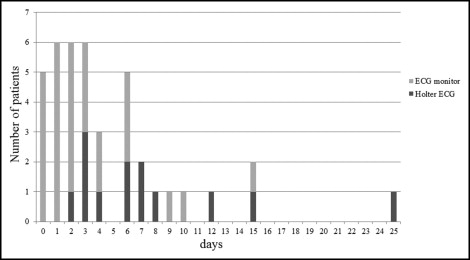
All patients underwent continuous electrocardiographic monitoring, and 24-hour Holter ECG was performed in 536 patients (91.8%) (large artery atherosclerosis 91%, small vessel occlusion 100%, cardioembolism 81%, and other or undetermined findings 91%). AF was documented in 40 patients (6.8%) during hospitalization (new AF group). Delayed AF was detected in 28 patients by ECG and in 12 by 24-hour Holter ECG. The median interval from admission to the appearance of AF was 3 days (range 0 to 25; Figure 1 ) . The non-AF group consisted of 544 patients (93.2%).
The baseline characteristics of the patients in the present study are listed in Table 1 . The median age in the new AF group (78 years, interquartile range [IQR] 71 to 84) compared to the non-AF group (72 years, IQR 62 to 80) (p = 0.0007) and the median NIHSS score on admission (14 [IQR 5 to 20] vs 4 [IQR 2 to 9], p <0.0001) were significantly higher in the new AF group than in the non-AF group. There were no differences in the other variables.
| Variable | Non-AF Group (n = 544) | New AF Group (n = 40) | p Value |
|---|---|---|---|
| Age (years) | 72 (62–80) | 78 (71–84) | 0.0007 |
| Women | 189 (35%) | 20 (50%) | 0.0520 |
| Previous ischemic stroke | 107 (20%) | 10 (25%) | 0.4162 |
| Previous coronary artery disease | 53 (10%) | 4 (10%) | 0.9578 |
| Previous heart failure | 1 (0.2%) | 1 (2.5%) | 0.1324 |
| Hypertension | 361 (66%) | 24 (60%) | 0.4127 |
| Diabetes mellitus | 139 (26%) | 11 (28%) | 0.7854 |
| Hyperlipidemia | 155 (28%) | 8 (20%) | 0.2478 |
| Smoker | 283 (52%) | 15 (38%) | 0.0762 |
| Preadmission medications | |||
| Warfarin | 17 (3%) | 1 (3%) | 1.0000 |
| Antiplatelet agents | 114 (21%) | 7 (18%) | 0.6065 |
| β blockers | 23 (4%) | 2 (5%) | 0.6861 |
| Angiotensin-converting enzyme inhibitors or angiotensin receptor blockers | 93 (17%) | 9 (23%) | 0.3849 |
| Calcium channel blockers | 106 (19%) | 9 (23%) | 0.6435 |
| Digitalis | 7 (1%) | 0 (0%) | 1.0000 |
| Diuretics | 26 (5%) | 0 (0%) | 0.2456 |
| Stroke subtype | <0.0001 | ||
| Large artery atherosclerosis | 125 (23%) | 0 (0%) | |
| Small vessel occlusion | 69 (13%) | 0 (0%) | |
| Cardioembolism | 38 (7%) | 37 (93%) | |
| Others/undetermined | 312 (57%) | 3 (7%) | |
| NIHSS score on admission | 4 (2–9) | 14 (5–20) | <0.0001 |
| Creatinine (mg/dl) | 0.72 (0.57–0.90) | 0.77 (0.59–0.91) | 0.4296 |
| BNP (pg/ml) | 35.2 (15.9–80.1) | 186.6 (68.7–386.3) | <0.0001 |
The mean interval from stroke onset to blood sample collection was 8.2 ± 6.9 hours. The median plasma BNP level of the new AF group was significantly higher than that of the non-AF group (186.6 pg/ml [IQR 68.7 to 386.3] vs 35.2 pg/ml [IQR 15.9 to 80.1], p <0.0001). Plasma BNP level was significantly associated with female gender (p <0.0001) and previous coronary artery disease (p = 0.0013). Furthermore, plasma BNP level was correlated with age (r = 0.194, p <0.0001) and NIHSS score (r = 0.260, p <0.0001).
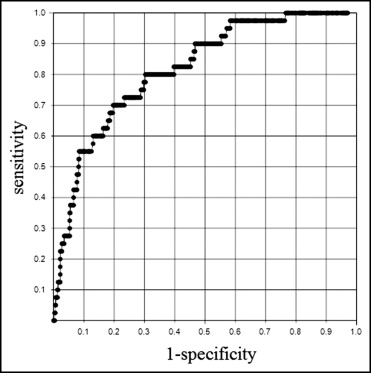
Age, female gender, NIHSS score on admission, and plasma BNP level were chosen as possible admission factors associated with delayed AF. The ability of BNP to identify the new AF group was assessed using receiver-operating characteristic curve analysis. A BNP level of 65.0 pg/ml had sensitivity of 80% and specificity of 70% ( Figure 2 ) . The area under the curve when BNP was used to differentiate the new AF group from the non-AF group was 0.82 (95% confidence interval 0.753 to 0.881). The cut-off levels of other variables that identified new AF with high sensitivity and high specificity were age >75 years (60% and 63%, respectively) and NIHSS score >7 (68% and 60%, respectively). On multivariate logistic regression analysis using these variables, NIHSS score >7 (odds ratio 3.4, 95% confidence interval 1.685 to 7.006, p = 0.0007) and plasma BNP >65.0 pg/ml (OR 6.8, 95% confidence interval 2.975 to 15.359, p <0.0001) were found to be independently associated with new AF ( Table 2 ). The detection rates of new AF according to BNP levels were as follows: 2% of patients with BNP <50 pg/ml, 4% of those with 50 to <100 pg/ml, 12% of those with 100 to <200 pg/ml, 26% of those with 200 to <400 pg/ml, and 38% of those with ≥400 pg/ml ( Figure 3 ) .