Definition and classification
The Seventh Report of the Joint National Committee on the Prevention, Detection, Evaluation, and Treatment of High Blood Pressure (JNC 7)1 defines normal blood pressure (BP) as systolic blood pressure (SBP) below 120 mmHg and diastolic blood pressure (DBP) below 80 mmHg. Hypertension is defined as SBP 140 mmHg or greater and/or DBP 90 mmHg or greater. Individuals with SBP 140–159 mmHg and/or DBP 90–99mmHg are classified as stage 1 hypertension while those at or above SBP 160 mmHg and/or DBP 100 mmHg constitute stage 2 hypertension.
A new category designated prehypertension has been added, and it is defined as SBP between 120 and 139 mmHg and DBP between 80 and 90 mmHg (Table 13.1). Prehyper-tension is a designation chosen to identify individuals at high risk for developing hypertension, so that both patients and clinicians are alerted to this risk and encouraged to intervene and prevent or delay the hypertension from developing. Individuals who are prehypertensive are not candidates for drug therapy based on their level of BP and should be firmly and unambiguously advised to practice lifestyle modification in order to reduce their risk of developing hypertension in the future. This classification does not stratify hypertensive individuals by the presence or absence of risk factors or target organ damage in order to make different treatment recommendations. Should either or both be present, JNC 7 suggests that all people with hypertension (stages 1 and 2) be treated. The treatment goal for individuals with hypertension and no other compelling conditions is < 140/90 mmHg. The goal for individuals with prehypertension and no compelling indications is to lower BP to normal levels with lifestyle changes, and prevent the progressive rise in BP using the recommended lifestyle modifications.
Table 13.1 JNC 7 blood pressure classification for adults aged 18 years and older*
| Category | Systolic/diastolic (mmHg) |
| Normal | <120/80 |
| Prehypertension | 120–139/80–89 |
| Hypertension | ≥140/90 |
| Stage 1 | 140–159/90–99 |
| Stage 2 | ≥160/100 |
Impressive evidence has accumulated to warrant greater attention to the importance of SBP as a major risk factor for cardiovascular disease (CVD). Clinical trials have demonstrated that control of isolated systolic hypertension (ISH), defined as SBP ≥160mmHg and DBP <90mmHg, reduces total mortality, cardiovascular mortality, stroke, and heart failure.2,3 A Clinical Advisory Statement4 recommends that SBP should be the principal measure for the detection, evaluation, and treatment of hypertension in both middleaged and older individuals.
Diagnosis and evaluation of hypertensive patients should include assessment of other cardiovascular risk factors or concomitant disorders that may affect prognosis and guide treatment (Box 13.1) and looking for identifiable causes of high BP. Identifiable causes of high BP include chronic kidney disease, coarctation of the aorta, Cushing’s syndrome and other glucocorticoid excess states including chronic steroid therapy, drug-induced or drug-related hypertension, obstructive uropathy, pheochromocytoma, primary aldosteronism and other mineralocorticoid excess states, renovascular hypertension, sleep apnea, and thyroid or parathyroid disease.1
Hypertension affects 20–30% of the world’ s population.5,6 When the new JNC 7 classification was applied to a nationally representative sample of US adults, it was found that in populations aged 20 or greater, an estimated 41.9 million men and 27.8 million women have prehypertension, 12.8 million men and 12.2 million women have stage 1 hypertension, and 4.1 million men and 6.9 million women have stage 2 hypertension.7 A higher percentage of men than women have hypertension before age 45. From age 45 to age 54, the percentages of men and women with hypertension are similar. After that, a much higher percentage of women have high BP than do men.8 The age-related changes in BP explain the increase in overall prevalence of hypertension with age and the increase in the prevalence of ISH with advanced age. From 1988–1994 to 1999–2002, the prevalence of hypertension in adults increased from 35.8% to 41.4% among blacks, and it was particularly high among black women, at 44.0%. Prevalence among whites also increased from 24.3% to 28.1%.9 Prevalence of prehy-pertension in African Americans is lower at older ages because of a higher prevalence of hypertension.10
*The classification is based on the average of two or more properly measured, seated BP readings in individuals not taking antihypertensive drugs and not acutely ill. When systolic and diastolic BP fall into different categories, the higher category should be selected to classify the individual’ s BP status. For example, 160/92 mmHg should be classified as stage 2 hypertension. Isolated systolic hypertension is defined as SBP ≥ 140 mmHg and DBP < 90 mmHg and staged appropriately. For example, 170/82 mmHg is defined as stage 2 isolated systolic hypertension. Adapted from JNC 71
BOX 13.1 Components for cardiovascular risk stratification in patients with hypertension
Major risk factors
Tobacco usage, particularly cigarettes
Dyslipidemia*
Diabetes mellitus*
Age older than 65 years for women, 55 years for men
Estimate glomerular filtration rate (GFR) <60mL/min
Family history of cardiovascular disease: women under age
65 or men under age 55
Microalbuminuria
Obesity* (body mass index ≥30kg/m2)
Physical inactivity
Target organ damage/clinical cardiovascular disease
Left ventricular hypertrophy
Angina/prior myocardial infarction
Prior coronary revascularization
Heart failure
Stroke or transient ischemic attack
Chronic kidney disease
Peripheral arterial disease
Retinopathy
* Components of the metabolic syndrome
Adapted from JNC 71
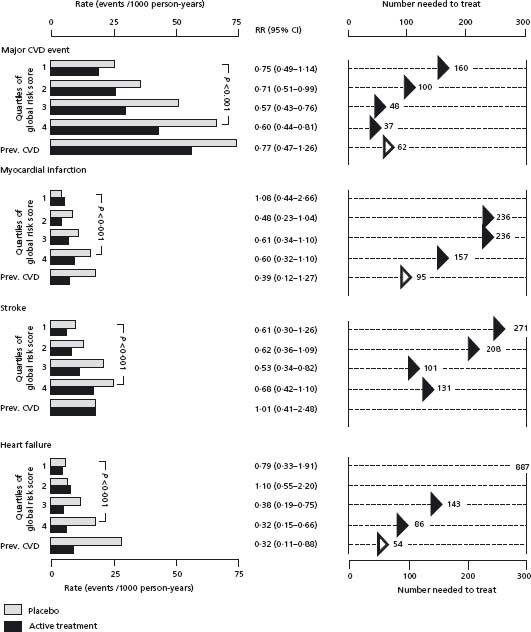
Hypertension is one of the major risk factors for cerebrovascular disease (stroke), coronary heart disease (acute myocardial infarction (MI) and angina pectoris), congestive heart failure, and chronic renal disease. The risk is directly associated with the BP level and with the presence of target organ manifestations and other cardiovascular risk factors. Ferrucci et al11 calculated the cardiovascular risk score for each participant in the Systolic Hypertension in the Elderly Program (SHEP) using the multiple risk factor assessment equation.12 This simple risk score is based on age, sex, total and high-density lipoprotein (HDL)-cholesterol, SBP, smoking, and diabetes. In the placebo group, the five-year rates of MI, stroke, and heart failure were progressively higher with higher quartiles of risk score in those who were free of cardiovascular disease at baseline. The relative event protection conferred by chlorthalidone-based treatment was similar across quartiles of risk. Thus, the absolute risk reduction increased by quartile of risk. This was reflected in a 2-to 10-fold lower “number needed to treat” (NNT) to prevent hypertensive complications in the highest-risk quartile (Fig. 13.1). The authors concluded that hypertensive patients with additional cardiovascular risk factors should be the prime candidates for antihypertensive treatment. Even in the absence of additional cardiovascular risk in individuals 40–70 years of age, each increment of 20 mmHg in SBP or 10 mmHg in DBP doubles the risk of CVD across the entire BP range from 115/75 to 185/115mmHG.13 The classification of “prehypertension” introduced by the JNC 71 recognizes this relationship and signals the need for increased education of healthcare professionals and the public health to reduce the BP levels in the general population.
Figure 13.1 Rates of new cardiovascular events, relative risks (RR), and 95% confidence intervals and estimates of NNTs by quartile of global risk score for SHEP participants free of CVD. The fifth group of bars in each panel shows data for subjects with prevalent (prev.) CVD at baseline. (Adapted from Ferrucci et al.11)
The article by Franklin and colleagues14 provides additional data on the natural history of BP ranges of 130–139 systolic or 80–89 diastolic (prehypertension as defined by the JNC 7). After adjustment for age and sex, the incidence of ISH per 100 person-years was 22.8 among individuals with BP 120/80 to 129/84 and 35.4 among individuals with BP 130/85 to 139/89, as opposed to only 6.6 among individuals with BP less than 120/80. Furthermore, 59% of subjects who developed ISH did not have diastolic hypertension at the baseline visit or at any other visit before ISH onset. These data provide further support to the argument that prehypertension, intended as the combination of normal plus high-normal BP categories, is a useful working definition in the setting of cardiovascular disease prevention because it identifies individuals at increased risk of developing progressive vasculopathy with stiffening of the aorta and elastic arteries over time.
Worldwide prevalence estimates for hypertension may be as much as 1 billion individuals, and approximately 7.1 million deaths per year may be attributable to hypertension.15 It has been identified as the leading risk factor for cardiovascular mortality, and is ranked third as a cause of disability-adjusted life-years.16 From 1994 to 2004, the age-adjusted death rate from hypertension increased 25.2%, and the actual number of deaths rose 54.6%. The 2004 overall death rate from hypertension was 17.9%. Death rates were distributed as follows: 15.6% for white males, 49.9% for black males, 14.3% for white females, and 40.6% for black females.17 Data from “Ambulatory care visits to physician offices, hospital outpatient departments, and emergency departments in the US” showed that the number of visits for essential hypertension was 45.3 million in 2002.18 This is projected as an estimated direct and indirect cost of high BP in 2007 to be $66.4 billion.17 Since as many as half of all hypertensives (defined as ≥140/90) remain untreated, the annual drug costs could easily double, unless we can change lifestyles more successfully or be more efficient in allocating resources.
Despite the established benefits of antihypertensive treatment, concerns are often raised about the prospect of use of antihypertensive drugs over decades by 25% or more of the adult population. All drugs have adverse effects and the cost of medical care for hypertension is considerable. Also, the 12-year follow-up of approximately 350 000 middle-aged men screened for the Multiple Risk Factor Intervention Trial shows that 32% of the coronary heart disease (CHD) deaths related to elevated BP occurred below the level at which drug treatment would be considered.19
The multifactorial etiology of hypertension is reflected by the large number of non-pharmaceutical approaches that have been tested.20–22 Two types of populations have been examined. In individuals with above-optimal (prehypertension stage according to the JNC 7) but non-hypertensive BP levels, lifestyle interventions have been tested to determine their effect on BP. The outcome has been either BP reduction in short-term trials or prevention of BP elevation with age and reduction in the incidence of hypertension in long-term trials. Trials have also been conducted in hypertensive patients with the objective of determining the BP-lowering effects of various non-pharmacologic interventions. One rationale has been that the findings are likely to be generalizable to non-hypertensive individuals. Another rationale has been to determine the efficacy of lifestyle modifications as definitive first-line or adjuvant therapy for hypertension. All treatment guidelines recommend lifestyle modifications as the first therapeutic approach in newly diagnosed, less severe hypertensive patients, with pharmacologic treatment to follow only in those who fail to respond adequately.
Cross-sectional or longitudinal observational studies have found the following factors to be associated with BP and prevalence or incidence of hypertension: adiposity, physical inactivity, alcohol consumption, high intake of sodium, low intake of potassium, magnesium, calcium, and certain types of dietary fiber, intake of certain macro-nutrients, and chronic stress.
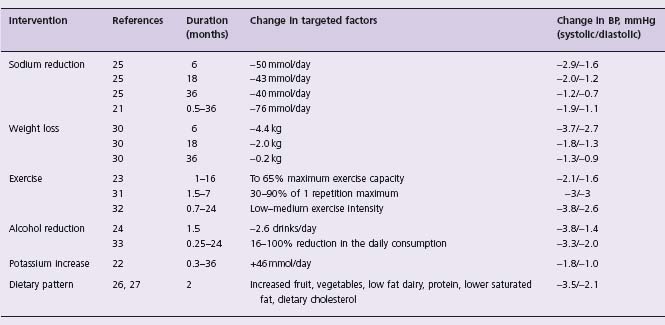
Trial results on the efficacy of interventions for prevention of hypertension are summarized in Table 13.2. Based on literature reviews, including meta-analysis, evidence of efficacy is conclusive for weight loss, exercise, diets high in fruits and vegetables, reduction in alcohol and sodium intake, and potassium supplementation (Level A). A weight reduction of 10 lb (4.5 kg) can be expected to lower the BP by approximately 4/3 mmHg. Since exercise, as part of efforts to achieve caloric balance, influences weight, distinguishing an exercise effect on BP from the effect of weight loss can be difficult, but there is good evidence of BP reduction from fitness training.23 Low-intensity/high-frequency activity appears as effective as or more effective than high-intensity exercise. A sodium reduction of 80–100 mmol/day induces an average BP reduction of 5/3 mmHg in hypertensives and 2/1 mmHg in non-hypertensives.21 Similar BP effects were observed in trials that accomplished alcohol reductions of about 85% (a mean consumption of 3 drinks/ day reduced to 3 drinks/week).24
The BP effects of lifestyle modifications are modest, but they appear to be additive under some circumstances.25 A short-term study reported substantial BP reductions in adults given a diet rich in fruits, vegetables, and low-fat dairy foods, and reduced saturated and total fat.26 A further reduction of SBP (2–8 mmHg) was observed when the sodium intake was reduced to below 100 mmol per day (2.4 g sodium or 6 g sodium chloride).27–29 However, counseling, if required on an indefinite basis through a traditional clinical setting, may not be more cost effective than drugs. Therefore, interventions (such as reducing salt intake by modifying processed foods) that can potentially be accomplished on a population basis are attractive. The efficacy of supplementation with magnesium, fiber, fish oil or calcium has been judged to be limited or unproven at this time.20 The trial findings are discordant and the effect sizes are small. Potassium supplementation (50–100 mmol KCl or equivalent increase from food) moderately reduces BP, especially in those who have a high sodium intake.22
In conclusion, long-term trials in individuals with high-normal BP have documented that sodium reduction,21,25 weight loss,30 exercise,31,32 alcohol reduction,24,33 and potassium supplementation22 can reduce the incidence of hypertension by as much as half (Level A). The most impressive results are from a five-year trial of a multifactorial intervention.34 The cumulative incidence of hypertension was 19.2% in the control group and 8.8% in the intervention group. The main factors contributing to this BP reduction were weight loss and sodium reduction.25 Overweight adults with prehypertension appear to be prime candidates for this intervention. Lifestyle modification is an integral part of management of hypertension. The BP-lowering effects are on average modest. Some patients do not respond or are unable to modify their lifestyles, while others respond well. As a consequence, many patients do not have to be placed on antihypertensive drugs and, if they are, lower drug doses or fewer drugs may be required. The challenge is to sustain the lifestyle modifications.
Placebo-controlled trials
Despite efforts at lifestyle modifications, most hypertensive patients require pharmacologic treatment. In the US, almost 25 million adults are currently taking antihypertensive medications.17 This high level of drug use to treat an asymptomatic condition has been justified by the high population burden of major morbidity and mortality causally related to untreated hypertension, and by strong evidence of treatment efficacy and safety from large, long-term clinical trials. In SHEP,35 which enrolled older adults ≥60 years with isolated systolic hypertension (SBP ≥160 mmHg), the five-year event rates for the combined endpoints of CHD and stroke per 100 patients were 13.6 in the placebo group and 9.4 in the active group. The risk difference of 4.2% means that about 24 older adults need to be treated for five years in order to prevent one coronary or cerebro-vascular event. It must be recognized that calculating the NNT in this manner from randomized clinical trials produces an underestimate for several reasons, chiefly the selection or self-selection of lower-risk patients into trials and the dilution of effects due to drop-in to active treatment by patients in the control group. For middle-aged populations, who are at lower risk, the NNT would be much higher. Because many people must receive therapy so that a few will benefit, even uncommon adverse effects may minimize or eliminate the BP-lowering benefits of antihypertensive therapy. Only with large, long-term trials such as SHEP can we be assured that the health benefits actually outweigh the health risks of particular therapies.
In a meta-analysis by Psaty et al,36 the evidence from large, long-term, controlled clinical trials of antihypertensive therapy was reviewed. The 18 randomized trials included 48 220 patients followed for an average of about five years. Clinical trials were classified according to the primary treatment strategy. While most studies used more than one drug, the agents were generally used in a stepwise fashion, and it was usually easy to identify the first-line therapy.
Compared with controls, beta-blocker therapy was effective in preventing stroke and congestive heart failure (Table 13.3). Similarly, high-dose diuretic therapy, which typically started with the equivalent of 50 mg/day of hydrochlorothiazide and often went to 100 mg/day, was associated with a reduced risk of stroke and heart failure. Despite lowering BP by an average of about 5–6 mmHg, neither beta-blocker therapy nor high-dose diuretic therapy demonstrated significant reduction of coronary disease events (Level A) (see Table 13.3).
Table 13.3 Meta-analysis of randomized, placebo-controlled clinical trials in hypertension according to first-line treatment strategy
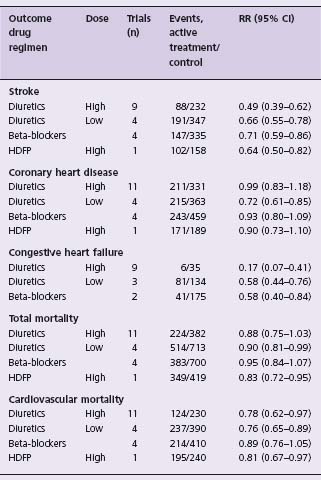
Trials (n) indicate number of trials with at least 1 endpoint of interest. Abbreviations: RR, relative risk; CI, confidence interval; HDFP, Hypertension Detection and Follow-up Program Study (5484 subjects in stepped care and 5455 in referred care). For these comparisons, the numbers of participants randomized to active therapy and placebo were 7768 and 12 075 for high-dose diuretic therapy; 4305 and 5116 for low-dose diuretic therapy; and 6736 and 12 147 for beta-blocker therapy. Because the Medical Research Council trial included two active arms, the placebo group is included twice in these totals, once for a diuretic comparison and again for beta-blocker comparison. The total numbers of participants randomized to active therapy and control therapy were 24 294 and 23 926, respectively.36
Compared with controls, low-dose diuretic therapy prevented not only stroke and heart failure but also CHD and cardiovascular and total mortality (see Table 13.3). In contrast to high-dose diuretic therapy, the adverse metabolic effects of low-dose diuretic therapy are minimal. The safety and proven effectiveness make low-dose diuretic therapy the logical first-line pharmacologic treatment for hypertension. The JNC 71 appropriately identifies low-dose diuretics as preferred first-line agents in the treatment of hypertension (Class I, Level A).
It is not clear why low-dose diuretic therapy prevents CHD, but neither high-dose diuretic therapy nor beta-blocker therapy is associated with a reduced risk of coronary disease. The low-dose trials (see reference 36 for references) were conducted mainly in older adults while the high-dose trials were conducted largely in middle-aged adults. Evidence from observational studies suggests that, compared with low-dose diuretic therapy, high-dose diuretic therapy is associated with an increased risk of sudden death.37 For high-dose diuretics, the most likely explanation for this increased risk of sudden death is the dose of the diuretics rather than the age of patients. Abrupt withdrawal of beta-blocker therapy is associated with an increased risk of MI in patients with high BP.38
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree