The evaluation of the fetus during labor by electronic fetal heart rate (FHR) monitoring is a complex process. Patterns that are known to have an excellent correlation with normal oxygenation and a vigorous baby at birth have been identified and are highly reliable. These must be distinguished from patterns that suggest suboptimal oxygenation so that action may be taken to reverse the problem, find alternatives to correct the abnormal pattern, or intervene operatively before damage or death can occur. Many factors must be weighed to determine the significance of the pattern. The FHR is evaluated for baseline rate, variability, and presence of accelerations or decelerations, as well as the progression of each component over time. Contraction frequency and strength must be considered. The patient’s parity, her rate of progress in labor, the estimated time of delivery, and maternal and obstetric complications are all factored into this rather complex equation.
Quantifying various parameters of fetal well-being by means of mathematical and statistical computations of the FHR is difficult. This is because the interpretation of FHR tracings is both a study of pattern recognition and a process of evaluating multiple clinical and heart rate variables in determining the status of fetal oxygenation. Previous chapters have dealt with the basic understanding of the physiology and technology of electronic FHR monitoring. This chapter is devoted to pattern recognition.
Efforts to arrive at universal nomenclature and criteria for various FHR patterns have not been uniformly successful. In 1997, a workshop convened by the National Institute of Child Health and Human Development (NICHD) published a document in an attempt to create more consistent and uniform terminology and guidelines for interpreting FHR patterns (
1). At that meeting, the participants found there were only two situations where there was universal agreement with respect to the significance of FHR patterns. The first was the pattern with normal baseline rate and variability and no periodic decelerations. It was agreed that such patterns were consistent with normal oxygenation and there were no requirements for intervention with respect to fetal wellbeing. The second patterns that were agreed to by the group as being consistent with hypoxia sufficient to cause death or damage were those patterns with repetitive late or variable decelerations or bradycardia all of which were accompanied by absent FHR variability. Any patterns between these two extremes could not gain general agreement from the group with respect to significance or management (
1).
In 2008, the Eunice Kennedy Shriver National Institute of Child Health and Human Development partnered with the American College of Obstetricians and Gynecologists and the Society for Maternal-Fetal Medicine to sponsor a workshop focused on electronic FHR monitoring (
2). This workshop gathered a diverse group of investigators with expertise and interest in the field to accomplish three goals: (a) to review and update the definitions for FHR pattern categorization from the prior workshop, (b) to assess existing classification systems for interpreting specific FHR patterns and make recommendations about a system for use in the United States, and (c) to make recommendations for research priorities for electronic fetal monitoring (EFM). A complete clinical understanding of EFM necessitates discussion of uterine contractions, baseline FHR rate and variability, presence of accelerations, periodic or episodic decelerations, and the changes in these characteristics over time. A number of assumptions and factors common to FHR interpretation in the United States are central to the proposed system of nomenclature and interpretation. Two such assumptions are of particular importance. First, the definitions are primarily developed for visual interpretation of FHR patterns but should be adaptable to computerized systems of interpretation. Second, the definitions should be applied to intrapartum patterns but also are applicable to antepartum observations.
Uterine contractions are quantified as the number of contractions present in a 10-minute window, averaged over
a 30-minute period. Contraction frequency alone is a partial assessment of uterine activity. Other factors such as duration, intensity, and relaxation time between contractions are equally important in clinical practice.
Listed as follows is terminology used to describe uterine activity:
Normal: five contractions or less in 10 minutes, averaged over a 30-minute window
Tachysystole: more than five contractions in 10 minutes, averaged over a 30-minute window
Characteristics of uterine contractions
The terms hyperstimulation and hypercontractility are not defined and should be abandoned.
Tachysystole should always be qualified as to the presence or absence of associated FHR decelerations.
The term tachysystole applies to both spontaneous and stimulated labor. The clinical response to tachysystole may differ depending on whether contractions are spontaneous or stimulated.
The following are EFM category definitions and descriptions based on the 2008 NICHD Working Group findings. Decelerations are defined as recurrent if they occur with at least one-half of the contractions.
CLASSIFICATION OF FETAL HEART RATE TRACINGS
A variety of systems for EFM interpretation have been used in the United States and worldwide. Based on careful review of the available options, a three-tiered system for the categorization of FHR patterns is recommended (see box). It is important to recognize that FHR tracing patterns provide information only on the current acid-base status of the fetus. Categorization of the FHR tracing evaluates the fetus at that point in time; tracing patterns can and will change. An FHR tracing may move back and forth between the categories depending on the clinical situation and management strategies used.
Category I FHR Tracings are Normal
Category I FHR tracings are strongly predictive of normal fetal acid-base status at the time of observation. Category I FHR tracings may be monitored in a routine manner, and no specific action is required.
Category II FHR Tracings are Indeterminate
Category II FHR tracings are not predictive of abnormal fetal acid-base status, yet presently there is not adequate evidence to classify these as Category I or Category III. Category II FHR tracings require evaluation and continued surveillance and reevaluation, taking into account the entire associated clinical circumstances. In some circumstances, either ancillary tests to ensure fetal well-being or intrauterine resuscitative measures may be used with Category II tracings.
NICHD 2008 Terminology Three Tier FHR Interpretation System |
Category I: Normal FHR Pattern |
Baseline rate 110-160 BPM |
Baseline FHR variability: moderate (5-25 BPM) |
Late and variable decelerations absent |
Early decelerations present or absent |
Accelerations present or absent |
Category II: Equivocal FHR Patterns |
Baseline Rate and Variability |
Baseline rate: Bradycardia (<110 BPM) not accompanied by absent variability |
Tachycardia (>160 BPM) |
Variability minimal (=or<5 BPM but present) |
Variability absent without recurrent decelerations |
Marked baseline variability (>25 BPM) |
Periodic Changes |
Absence of induced accelerations after fetal stimulation |
Recurrent variable decelerations accompanied by minimal or moderate baseline variability |
Prolonged deceleration >2 min but <10 min |
Recurrent late decelerations with moderate baseline variability |
Variable decelerations with other characteristics such as slow return to baseline or overshoot |
Category III: Abnormal FHR Patterns |
Absent FHR variability and of the following: |
|
Recurrent late decelerations |
|
Recurrent variable decelerations |
|
Bradycardia |
|
Sinusoidal pattern |
Category III FHR Tracings are Abnormal
Category III tracings are associated with abnormal fetal acidbase status at the time of observation. Category III FHR tracings require prompt evaluation. Depending on the clinical situation, efforts to expeditiously resolve the abnormal FHR pattern may include but are not limited to provision of
maternal oxygen, change in maternal position, discontinuation of labor stimulation, treatment of maternal hypotension, and treatment of tachysystole with FHR changes. If a Category III tracing does not resolve with these measures, delivery should be undertaken. We attempt to follow these new guidelines for nomenclature in this edition of this book.
PATIENT IDENTIFICATION
Many modern monitoring systems have electronic storage of patient information and EFM tracings. These systems require patient data entry before starting the monitor on a new patient. However, many hospitals continue to store paper records for backup medical records, for teaching purposes, or because some information (e.g., continuous fetal pulse oximetry data) may not be stored on the digital record. Therefore, it is important to appropriately label the paper record as well. Monitors should be identified numerically and tracings labeled accordingly. Should a technical problem occur, it can be traced to the correct monitor. Also, different monitors may have different logic and other technical characteristics, and when a facility has various brands, the clinician can better interpret the tracing by taking the make and model into consideration.
BASELINE FETAL HEART RATE
The normal baseline FHR ranges from 110 to 160 beats per minute (BPM). The NICHD defined baseline FHR as the mean FHR during a 10 minute window. The mean is expressed in increments of 5 BPM. Changes of shorter duration are called “periodic changes.” While it is appropriate to attempt to create a defined duration of a periodic change, for which a more sustained rate becomes a baseline change, this is often inconsistent with what is the obvious physiologic explanation for a prolonged periodic change. For example, a profound hypotensive episode that results in a prolonged deceleration will ultimately return to the original baseline when the insult is reversed. Thus the deceleration may have lasted longer than 10 minutes and, according to the previous NICHD definition, would now be called a bradycardia, but it was truly not a baseline change. Similarly, a fetus that is unusually active may have an acceleration that lasts considerably longer than 10 minutes but returns to the original baseline when the fetus returns to a more quiet state.
Fetal Tachycardia
Fetal tachycardia is defined as a baseline heart rate in excess of 160 BPM. Factors associated with or causing tachycardia are listed in
Table 6.1. Because tachycardias represent increased sympathetic and/or decreased parasympathetic autonomic tone, they are generally associated with a loss of variability (
Fig. 6.1). Most fetal tachycardias do not reflect a hypoxic fetus, particularly when present in a term gestation. In a preterm
fetus or when seen in a term pregnancy without an obvious explanation (e.g., maternal fever), close evaluation is critical.
Fetal Bradycardia
Bradycardia is a baseline FHR of <110 BPM Bradycardia, within the range of 80 to 110 BPM with moderate variability generally indicates good oxygenation without acidemia (
Fig. 6.2). Slowing of the baseline heart rate is most likely in response to an increased vagal tone (
3). Fetal bradycardia that is first noted at the initiation of monitoring may be difficult to distinguish from a prolonged deceleration. Generally, prolonged decelerations are associated with loss of variability and their rate fluctuates up and down rather than remaining consistent, unless rates below 70 BPM are seen.
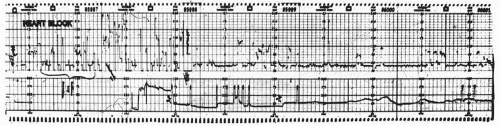
Actual baseline FHRs of <70 BPM are generally seen without variability and may represent congenital heart block (
Fig. 6.3). Persistent bradycardia from complete atrioventricular dissociation should alert the clinician to the possible diagnosis of maternal connective tissue disease, most often systemic lupus erythematosus, which results in fetal heart block and bradycardia consequent to transplacental passage of maternal antibodies that have an affinity for fetal cardiac conduction fibers (
4) (see
Chapter 4). Structural cardiac defects and cytomegalovirus infections are also potential etiologies of congenital heart block. To reliably establish that fetal cardiac activity is present and that the persistent bradycardia is due to fetal heart block, confirmation with realtime ultrasound is necessary. Ultrasound allows for a further advantage in that cardiac structure can be carefully evaluated as well (see
Chapter 7). However, ultrasound is really only an option in the antepartum period because it may not be possible to take the time required to make this evaluation in labor where either a bradycadia or prolonged deceleration may require urgent operative intervention. When the diagnosis of complete fetal heart block is made antenatally, the problem then becomes how to monitor the fetus in labor because the normal alterations in FHR in response to hypoxrmia and other central nervous system (CNS) input cannot be transmitted to the ventricles. Thus, in this situation, the FHR cannot be used as a way to monitor for fetal hypoxemia and to rule out acidemia. Three options are reasonable in this situation. Intermittent scalp pH is theoretically an option, but the need for repeating the test every 30 minutes makes this option unrealistic except in very rapid labors. In the past, an elective cesarean section was often undertaken, simply because there had been no other way to monitor the fetus. Although no longer available in the United States, fetal pulse oximetry has
provided a logical option, and limited data suggest that this is a safe and effective way of monitoring patients whose fetal arrhythmia prevents adequate FHR monitoring (
5).
Bradycardia with moderate variability may occur in the second stage and is not indicative of abnormal fetal acidbase status. Other, more rare causes of fetal bradycardia are maternal hypothermia, prolonged hypoglycemia, betablocker therapy, and fetal panhypopituitarism with brainstem injury (
6). Persistent bradycardia requires careful evaluation to ensure that it is not the maternal heart rate being recorded in the presence of a fetal demise or secondary to signal ambiguity. Real-time ultrasound can establish the correct diagnosis and thus avoid unnecessary and potentially dangerous therapy in the presence of an already dead fetus. Maternal heart rate can also be recorded from the Doppler transducer and in the rare situation where the fetus is dead the MHR may be recorded from the scalp electrode (see
Chapter 4).
Variability
In the 2008 NICHD update on nomenclature, FHR variability was classified as follows:
Absent
Minimal (1 to 5 BPM)
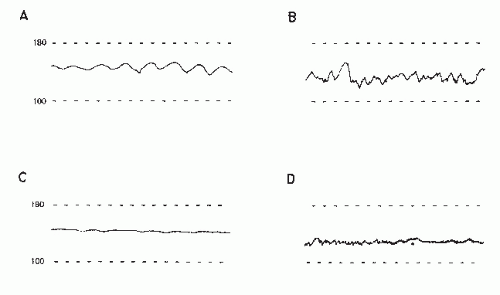
Moderate (5 to 25 BPM)
Increased (>25 BPM)
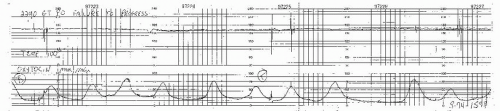
In determining the immediate fetal status, the most important single FHR characteristic is variability. Moderate variability (6 to 25 BPM peak to trough) is a reflection of intact neurologic modulation of the FHR and of intact or normal cardiac responsiveness. The two components are short-term and long-term variability (LTV) (
Fig. 6.4). Shortterm variability (STV) is the beat-to-beat irregularity caused by the normal variance in intervals between consecutive cardiac cycles. It is a consequence of the constant “push-pull” effect of sympathetic and parasympathetic nervous system input. LTV is the waviness of the FHR tracing, generally at a frequency of 3 to 5 cycles per minute. With older EFM systems, using external Doppler, FHR variability could not be accurately determined because Doppler monitoring can artifactually increase FHR variability due to the imprecision of the signal. With newer Doppler signal processing systems, however, variability can be accurately assessed. Although there is utility in distinguishing between LTV and STV in research settings because mathematical quantification of these two types are different, there is no current evidence that the distinction between the two has any clinical relevance. Perhaps the single exception to this is the sinusoidal tracing that is absent short term but uniformly increased LTV. Increased variability has been shown in animals to be a sign of mild hypoxia (
7). However, when FHR variability is moderate or increased, fetal pH is usually normal.
As gestation advances and the fetal autonomic nervous system matures, the baseline FHR decreases and both STV and LTV increases. This is thought to reflect an increase in vagal control of cardiovascular reflexes. Decreased variability may be seen with prematurity, fetal sleep cycles or anything that causes fetal CNS depression. Fetal hypoxemia with acidemia is the most worrisome cause; however, any condition that depresses the CNS can also decrease variability (
Table 6.2). In labor it is critical to carefully review the strip for the presence or absence of late, variable, or prolonged decelerations when decreased variability is seen. It is highly unlikely that minimal or absent variability reflects CNS depression due to metabolic acidemia unless there are decelerations indicating ongoing hypoxemia. The exception to this rule may occur in the fetus who presents in labor with a absent variability without decelerations, as one cannot rule out an hypoxic insult prior to the initiation of electronic monitoring. Especially in the absence of significant decelerations, other causes of CNS depression should be considered. Certain drugs may be responsible (
Table 6.3), particularly drugs that depress the CNS (
Fig. 6.5) and drugs with autonomic blocking effects. Parasympathetic blocking drugs
decrease variability while increasing baseline heart rate. Sympatholytic drugs (e.g., beta-adrenergic blockers) also decrease variability but decrease baseline heart rate.
Baseline heart rate variability is also associated with fetal wakefulness. When the fetus is sleeping, there may be decreased variability (
Fig. 6.6). Usually the variability will spontaneously return to its previous level after a reasonable time, although the duration of fetal sleep states in labor is not as consistent as in the antepartum period. Stimulation of the fetus by manipulation of the uterus or noise may arouse the fetus and cause the variability to return or result in a FHR acceleration, both of which reliably predict the absence of abnormal fetal academia. The new onset of loss of variability in the absence of periodic FHR decelerations with contractions is not a sign of fetal hypoxia.
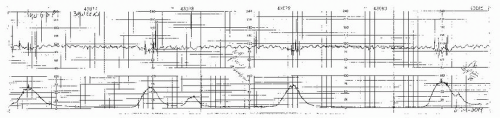
From an intrapartum monitoring perspective, the most ominous cause of decreased variability is fetal hypoxemia where FHR decelerations precede the loss of variability. In the presence of heart rate patterns, such as persistent late decelerations, loss of variability is associated with a high incidence of fetal acidosis and low Apgar scores (
8) (
Fig. 6.7), particularly in the case of preterm infants (
9). A most difficult heart rate pattern to interpret is absent variability seen in the fetus with a normal baseline heart rate and no decelerations. This may represent a previous insult to the fetus that has since been corrected but has resulted in persistent neurologic damage. Also, this pattern may be seen in fetuses with significant congenital anomalies, especially of the central nervous and cardiac systems. Extreme prematurity is associated with decreased variability and nonreactive FHR patterns. Finally, these patterns can be idiopathic and occur in a subsequently vigorous and healthy neonate (
10).
Table 6.3 lists the causes of decreased variability.