Fetal movement (FM) counting
Assessment of uterine growth
Antepartum fetal heart rate (AFHR) testing
Biophysical profile (BPP) testing
Doppler velocimetry
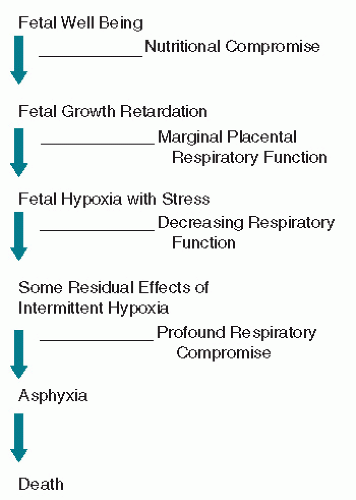 Figure 11.1. Theoretical scheme of fetal deterioration with progressive uteroplacental insufficiency. |
TABLE 11.1 Conditions placing the fetus at risk for UPI | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
TABLE 11.2 Indications for antepartum testing by primary surveillance test | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
is usually taught how to count movement, because the reason for her perceived decreased count is often her nonrecognition of movement that is there. When simultaneous real-time ultrasound scanning has been done with patients asked to note the perceived movements, more movements are observed by ultrasound than are perceived by the patient (11). Most patients will feel three movements in just a few minutes, so very little time is actually required for the patient. A FM count that drops below three in 12 hours or that ceases for 12 hours is termed the “movement alarm signal” by Sadovsky, which correlates with impending fetal death (12,13 and 14). Moore and Piacquadio (15) performed a pilot study in which all patients were instructed to monitor the elapsed time it took every day from 28 weeks to register ten FMs. An NST was performed if 2 hours elapsed without 10 movements. They report a fourfold reduction in fetal mortality associated with complaints of decreased FM using this simple protocol. However, while awareness of FMs correlates with improved fetal and neonatal outcomes, the ability to identify a specific quantitative alarm for decreased FMs has not been successful (16). As an added point, the patient presenting with a complaint of absent or markedly decreased FM who has a nonreactive NST should be considered to be at increased risk for acute fetal-maternal hemorrhage (see Chapter 12).
TABLE 11.3 Distribution of test results by primary surveillance test | ||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ||||||||||||||||||||||||
TABLE 11.4 Indications and gestational age for AFHR testing | |||||||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| |||||||||||||||||||||||||||||||||||||||||||||||
What follows is a description of the various testing options available with particular emphasis on the evolution and reported application of the CST, NST, BPP, and the MBPP. There continues to be argument and controversy regarding the relative value and efficacy of these various types of fetal assessment despite their well-established place in the clinical practice of obstetrics (25).
 Figure 11.2. Spontaneous negative contraction stress test (no oxytocin needed). The patient is actually found to be in labor. |
associated with uterine tachysystole and fails to achieve adequate uterine activity in approximately 20% of tests (38,39,40 and 41). The test is best performed with the patient initially rolling or tugging on one nipple through her clothing until a contraction occurs. If no contraction results following 2 to 3 minutes, the patient is asked to perform bilateral stimulation following a 5-minute rest period. This cycle of stimulation is then repeated until adequate uterine activity is documented. Figure 11.4 is an example of a reactive negative CST done with nipple stimulation. Following the appearance of adequate uterine activity, oxytocin infusion or breast stimulation is stopped and the patient continued to be monitored until activity significantly diminishes or disappears (42).
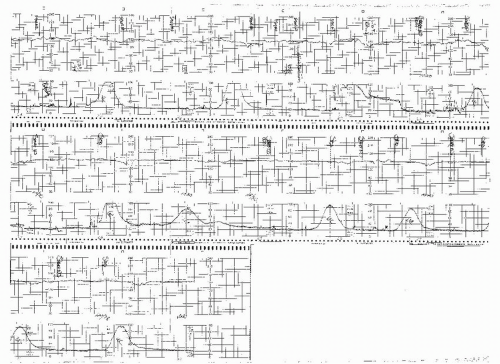
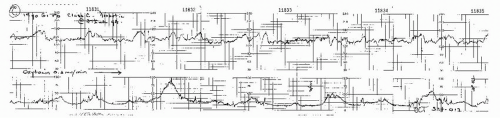 Figure 11.3. Negative contraction stress test result. Three contractions are obtained in 10 minutes, lasting more than 60 seconds each, with adequate quality fetal heart rate recording. |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree