Acute Traumatic Aortic Transection
Benjamin J. Pearce
Jay D. Pal
John H. Calhoon
Acute traumatic aortic transection (TAT) remains a devastating complication of blunt trauma with a mortality of 80% at the scene and is the second leading cause of death from blunt injuries. Further, up to half of the patients surviving to hospital admission perish within the first 4 hours. Due to the mechanism of injury, TAT is rarely an isolated finding and confounding extrathoracic injuries complicate both the diagnosis and management strategy. A multidisciplinary approach including trauma services, critical care management, radiology, and the cardiovascular surgeon is critical to assessing the spectrum of injuries and decisively executing a therapeutic plan.
Increasing sophistication of trauma systems and the introduction of multidetector computed tomographic angiography (CTA) have led to the increase in both the initial survival of TAT patients to hospital admission and diagnosis of aortic pathology. The ability to obtain quick, high-resolution imaging with multiplane reconstruction through CTA has replaced traditional angiography in the diagnosis of TAT. In addition, the liberal application of computed tomography scanning has allowed for better assessment of concurrent injuries and allowed for appropriate planning of either an open or endovascular surgical approach. Further, documented decrease in rupture rates with the administration of anti-impulse therapy has allowed for more patients to reach the operating room and a small subset of patients to be treated without surgery.
Despite these advances, TAT continues to be a highly lethal entity. Operative mortality approaches 25% in recent American Association for the Surgery of Trauma (AAST) prospective trials on management of TAT. Data are promising for the ability of thoracic endovascular aortic repair (TEVAR) to improve outcomes in this population; however, the applicability of this technology to all patients is controversial and still limited by anatomic and device-specific constraints. Continued experience in open surgical repair (OSR) for TAT is critical in approaching these complex patients. The most efficacious approach to management will be appropriate selection of both the timing and technique of intervention.
NATURAL HISTORY AND PATHOLOGIC CONSIDERATIONS
Eighty percent of acute TAT occur as a result of motor vehicle collisions. Other causes include kicks, falls from heights, and crush injuries. Most series report that 20% of motor vehicular accident fatalities are a result of TAT. The incidence is higher in the young adult population and has an increased male-to-female ratio. More than one half of the transections occur at the aortic isthmus, 25% can occur in the arch and great vessels, and the remaining throughout the descending and abdominal aorta. Recent pooled data of OSR only trials for meta-analysis reported the need for open arch reconstruction in TAT at 4.1%. This was associated with significantly elevated mortality. Similarly, concomitant repair of injury at the isthmus and abdominal aortic branches has increased mortality and morbidity, likely due to the greater force and associated injuries needed to create this spectrum of disease.
Multiple mechanisms of injury have been reported by autopsy study and ex vivo mechanical testing of the tensile strength of the aorta. The most commonly accepted theory is the sudden movement of the heart and arch against the fixed position of the descending thoracic aorta. In this deceleration model, the greatest tension point is the aortic isthmus, resulting in the spectrum of injuries in TAT. Other proposed mechanisms include a sudden rise in blood pressure, high-pressure reflected wave from sudden occlusion of the aorta at the diaphragmatic hiatus, and stretching or “pinching” of the aorta by the osseous structures in the thorax. Regardless of mechanism, the natural history of TAT is such that immediate death was historically reported in 80% to 90% of cases. In a contemporary autopsy study of 242 cases of fatal TAT, Burkhart et al. (J Trauma 2001) published immediate mortality in 57%, 37% within 4 hours of admission, and only 6% who died >4 hours after hospital arrival.
A basic understanding of the underlying pathology can also greatly aid in diagnosis and decision making regarding surgical timing. TAT is a continuum of disease spanning from subintimal hemorrhage to complete transection, and extent of injury likely plays the ultimate role in survival. Parmley et al. (Circulation 1958) classified the injuries as intimal hemorrhage only, intimal hemorrhage with laceration, medial laceration, complete laceration of all layers, pseudoaneurysm formation, and free aortic hemorrhage. The fine detail provided by CTA allows for classification of these injuries along this spectrum at diagnosis.
 DIAGNOSIS
DIAGNOSISWith a history of any deceleration injury, there should be a suspicion for possible acute aortic transection. Symptoms on arrival at the emergency room in a conscious patient range from nonspecific complaints to those of chest pain, intrascapular pain, hoarseness, dyspnea, dysphasia, and frank paralysis. Physical examination findings include rib fractures, sternal fractures, and even imprints of the steering wheel on the chest. The cervical and thoracic spines are also vulnerable, and these should be carefully examined. Hypertension in the arms, so-called coarctation syndrome, has been reported. It is important to carefully examine the pulses in the upper and lower extremities and check for any differences. A baseline neurologic examination is extremely important in these patients because paraplegia may be present preoperatively and may be due to other causes such as spinal fractures and dislocations.
In the era of liberal CT scanning, chest roentogram has a less important role, but diligent examination is still warranted,
especially in patients with otherwise underwhelming presentation. An initial chest radiograph should be obtained as soon as the patient’s cervical spine is cleared. An upright posteroanterior (PA) film is desirable; however, the most upright anterior-posterior (AP) film possible is the best alternative. Supine chest radiographs usually reveal a widened mediastinum. Any abnormality seen in the mediastinum on an upright PA chest film should raise the suspicion for aortic transection and prompt further investigation. Various specific radiographic findings associated with aortic transection include mediastinal widening, obscurity of the aortic knob, obliteration of the AP window, tracheal deviation, depression of the left mainstem bronchus, widening of the paravertebral stripe, deviation of the esophagus (seen most commonly as deviation of the nasogastric tube), and a left hemothorax. Fractures of the first rib and/or scapula should raise the suspicion of an aortic injury due to the extreme force required to fracture these bones. A history of a deceleration injury in conjunction with an abnormal mediastinum seen on the chest radiograph should prompt further investigation.
especially in patients with otherwise underwhelming presentation. An initial chest radiograph should be obtained as soon as the patient’s cervical spine is cleared. An upright posteroanterior (PA) film is desirable; however, the most upright anterior-posterior (AP) film possible is the best alternative. Supine chest radiographs usually reveal a widened mediastinum. Any abnormality seen in the mediastinum on an upright PA chest film should raise the suspicion for aortic transection and prompt further investigation. Various specific radiographic findings associated with aortic transection include mediastinal widening, obscurity of the aortic knob, obliteration of the AP window, tracheal deviation, depression of the left mainstem bronchus, widening of the paravertebral stripe, deviation of the esophagus (seen most commonly as deviation of the nasogastric tube), and a left hemothorax. Fractures of the first rib and/or scapula should raise the suspicion of an aortic injury due to the extreme force required to fracture these bones. A history of a deceleration injury in conjunction with an abnormal mediastinum seen on the chest radiograph should prompt further investigation.
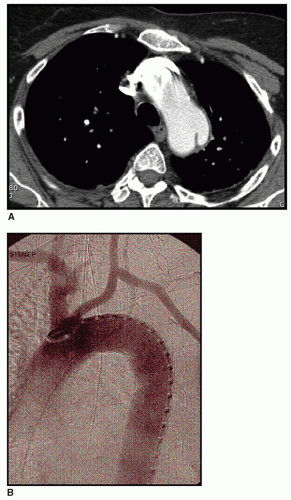
CTA has replaced arch angiography as the modality of choice in investigating blunt aortic injury (Fig. 62.1). Magnetic resonance imaging (MRI) has also been advocated, especially considering the physiologic information which can be gained from functional MRI; however, it is often too cumbersome to obtain in the acute trauma situation. Transesophageal echocardiography (TEE) has been shown to be a useful diagnostic tool, but this test may not be readily available in all institutions, and its accuracy is operator anatomy dependent. With TEE, there is also a risk of free aortic rupture due to patient gagging or Valsalva from inadequate sedation causing increase in intrathoracic pressure. In our experience, TEE has been most useful when the patient was sent to the operating room emergently for other life-threatening injuries and there remains a question regarding the diagnosis of acute TAT. Intraoperatively, TEE is useful in helping to rule in or out aortic injury. Operative exploration is now justified without the use of arteriography in the acute setting with a suggestive clinical picture along with other diagnostic radiologic findings such as that seen on plain radiographs, CT scans, and intraoperative TEE findings. Associated injuries are common, and acute TAT is rarely seen as an isolated entity. Injuries to other organ systems (intracranial, intra-abdominal), including major fractures (spine, pelvis), must be considered and treated if a successful outcome is to be obtained. When associated injuries are present, the cardiovascular surgeon should be involved with the treatment and prioritization of these injuries.
Three recent papers have attempted to grade CT findings of TAT along the lines of pathologic injury. The Simplest of these is the Vancouver simplified grading systems described by Lamarche et al. (J Thorac Cardiovasc Surg 2011). In order from least to most severe: Grade I is defined as an intimal flap/thrombus/hematoma <1 cm in length; Grade II as intimal flap/thrombus/hematoma >1 cm; Grade III pseudoaneurysm formation; and Grade IV free contrast extravasation. Furthermore, the authors correlated these findings to outcomes in a small subset of patients, advocating observation for all Grade I and some Grade II injuries with no mortality. Grade III injuries were treated with intervention and hospital survival in 90% and Grade IV with only 33% survival despite intervention. These favorable data can be used to guide operative decision making.
CTA can be both diagnostic and used for planning of operative intervention. Sizing of landing zones for TEVAR, presence of anomalous great vessel anatomy, patency of vertebral circulation, evidence of prior coronary grafting from internal mammary, angulation of aortic arch, and presence of other injuries can all be assessed with appropriate CTA. When CTA is being performed for suspected TAT, it is advantageous to scan the entire vascular tree from neck to femoral vessels. This allows for assessment of access vessels
in the event of possible TEVAR without adding to the contrast administration. One must consider that in younger patients with compliant vessels, intake CT scans may underestimate the actual size of the aorta and iliac system. Several millimeters of variance have been described in the under-resuscitated state. Furthermore, the more dynamic pulsation of the aorta in a young patient can be misrepresented on a static scan. This can lead to inappropriate oversizing of an endograft as will be described later. In patients with a documented anaphylactic reaction to iodine, or concern for renal failure, a noncontrasted thin cut CT scan can still be a useful adjunct in evaluating TAT and for operative planning and can be augmented by other modalities such as TEE and intravascular ultrasound (IVUS).
in the event of possible TEVAR without adding to the contrast administration. One must consider that in younger patients with compliant vessels, intake CT scans may underestimate the actual size of the aorta and iliac system. Several millimeters of variance have been described in the under-resuscitated state. Furthermore, the more dynamic pulsation of the aorta in a young patient can be misrepresented on a static scan. This can lead to inappropriate oversizing of an endograft as will be described later. In patients with a documented anaphylactic reaction to iodine, or concern for renal failure, a noncontrasted thin cut CT scan can still be a useful adjunct in evaluating TAT and for operative planning and can be augmented by other modalities such as TEE and intravascular ultrasound (IVUS).
MEDICAL THERAPY
The use of anti-impulse therapy was first applied in the management of descending thoracic dissection and has expanded to use in the management of acute traumatic aortic injuries. This therapy decreases the wall stress tension in the aorta by means of beta-blockade and, if necessary, vasodilating agents. Prospective studies have demonstrated a decrease in the incidence of spontaneous rupture with the institution of appropriate anti-impulse therapy. This is an important aspect in the management of multiply injured patients where other life-threatening injuries need to be addressed first, prior to aortic repair.
The goals of therapy are to reduce systolic blood pressure to <100 mmHg. This is best achieved with a combination of pain control, inotropic/chronotropic blockade, and afterload reduction. Often overlooked is the importance of adequate analgesia. The contribution of acute pain to the cascade of catecholamine release is significant and appropriate treatment with intravenous opiates is warranted. One of the most feared complications of TAT is paraplegia from spinal cord infarction either spontaneously or from treatment. As such, the use of intrathecal analgesia is contraindicated.
Initiation of therapy with beta-blockade is the standard of care. The goal heart rate is <80 bpm. By initiating beta-blockade early, reflex tachycardia and catecholamine release are blunted with the initiation of afterload reducing agents. Choice of a betablocker, for example labetalol, with α and β adrenergic effects may achieve appropriate cardiac and peripheral effects with a single agent. However, this may precipitate pulmonary complications in at-risk patients and thus initiation of therapy with a short acting agent, for example esmolol, may be more prudent in selected cases. Initiation of sodium nitroprusside infusion after beta-blockade has been an effective agent. However, recent data have shown similar efficacy of nicardipine infusion in treatment of acute type B dissection without the risk of cyanide toxicity and may be applied to TAT.
TIMING OF REPAIR
While expectant management of a potentially fatal injury pattern can be anxiety provoking, the scope of injuries in the TAT patient often makes this management advantageous. Perceived advantages of delayed repair include allowing for appropriate resuscitation, time for full evaluation and treatment of other life-threatening injuries, stabilization of intracranial or solid-organ injuries, which may potentially hemorrhage with heparinization, improvement in pulmonary mechanics in patients requiring significant ventilator support, correction of hypothermia and coagulopathy, and allow for proper sizing and acquisition of endografts if TEVAR is planned.
An inherent bias exists in the literature regarding this issue. Intuitively, the patients with the most severe grade of TAT will necessarily require a more immediate operation and have expected worse outcomes. The AAST evaluated this issue in a prospective manner. Two major groups were examined—those with and without major extrathoracic injuries. In the group with major extrathoracic injuries, the mortality in the early repair group was 21.6% versus 3.2% in the delayed repair group. Even when adjusting for severity of injuries and modality of repair in a regression analysis, this trend toward improved overall survival in delayed repair was evident. A similar trend was described in patients with no other associated injuries. The authors in the AAST advocate delayed repair when feasible in all comers, although it is more difficult to justify observation of a potentially fatal injury in an otherwise stable patient based on these data alone. Conversely, a recent consensus statement from the Society of Vascular Surgery states that most patients should be repaired within 24 hours when feasible. Careful consideration of the entire clinical picture combined with appropriate grading of the injury on CTA will lead to the most judicious timing of intervention.
CHOICE OF MODALITY
TEVAR for TAT has rapidly gained acceptance as an alternative to OSR. In fact, in a recent meta-analysis of OSR versus TEVAR for TAT, TEVAR was performed in the majority of cases (60%). There are currently several device-specific trials attempting to gain Federal Drug Administration (FDA) indication for TAT; however, it must be mentioned that this remains an off-label therapy for commercially available grafts in the United States at this time.
The perceived advantages of TEVAR in other aortic pathologies also make it an attractive option in TAT as well. The devices can be delivered from remote sites without the need for a major cavity operation in patients who may have associate injuries in these areas. In addition, heparin administration is significantly less than that needed for cardiopulmonary bypass, and TEVAR can be performed under regional anesthesia in many cases. No aortic cross-clamping is needed attenuating the hemodynamic effects on both the heart and distal vasculature. Reported rates of spinal cord infarction are significantly less with TEVAR than OSR, and paraplegia can often be managed expectantly without the need of prophylactic spinal drainage.
However, as with any new technology, TEVAR has developed a new set of complications. Rupture of access vessels due to the large-bore devices was common in early experiences and still remains an important consideration in operative planning. Careful attention to evidence of anomalous arch anatomy or prior coronary bypass is crucial to prevent coverage of vital branch vessels. Proper oversizing of the endograft is difficult in the young trauma patient, and angulation of the distal arch can make delivery and seal of the proximal aspect of the stent difficult, both of which may lead to proximal type I endoleak or collapse of the endograft. Type I and Type II endoleaks are present in up to 20% of cases necessitating repeat intervention.
Similar to evaluating delayed versus immediate intervention, bias exists in evaluating the literature regarding OSR versus TEVAR. In five of six meta-analyses comparing the two modalities, operative mortality was in favor of TEVAR, but in those studies reporting timing or severity of injury, OSR was more often the modality chosen. However, in more contemporary series, the perioperative mortality and paraplegia rate have favored TEVAR. In the same cohort of patients from the prior study, the AAST investigators evaluated OSR versus TEVAR in a prospective manner. In patients
with and without other associated injuries, the mortality was significantly lower with TEVAR as was paraplegia (2.9% OSR. 0.8% TEVAR). There was no associated difference in ICU stay, systemic complications, or days of ventilator dependence.
with and without other associated injuries, the mortality was significantly lower with TEVAR as was paraplegia (2.9% OSR. 0.8% TEVAR). There was no associated difference in ICU stay, systemic complications, or days of ventilator dependence.
The pooled data on TEVAR are limited by a mean follow up of only 18 months. Similar to evaluation OSR versus TEVAR for aneurysm disease, it appears that the survival benefit of TEVAR is lost after 1 year, likely due to the not insignificant morbidity and mortality of subsequent interventions required in patients treated with TEVAR. Perhaps, the most important factor limiting application of TEVAR to all cases of TAT is the lack of long-term data regarding performance of the grafts in young patients. Concern exists regarding potential for migration as the aorta dilates with age. Further, it is unknown whether these devices will suffer material fatigue when implanted for extended periods of time. Several reports describe successful salvage of failed endografts with open repair.
No clear data exist to definitively favor one modality over the other. A strong trend toward decreased perioperative mortality and paraplegia in patients treated with TEVAR for TAT. This technique can expand therapy to patients who are not candidates for open repair. Evaluation of anatomy, associated injuries, urgency of repair, and patient age will lead to proper operative decision making.
OPEN SURGICAL MANAGEMENT
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree