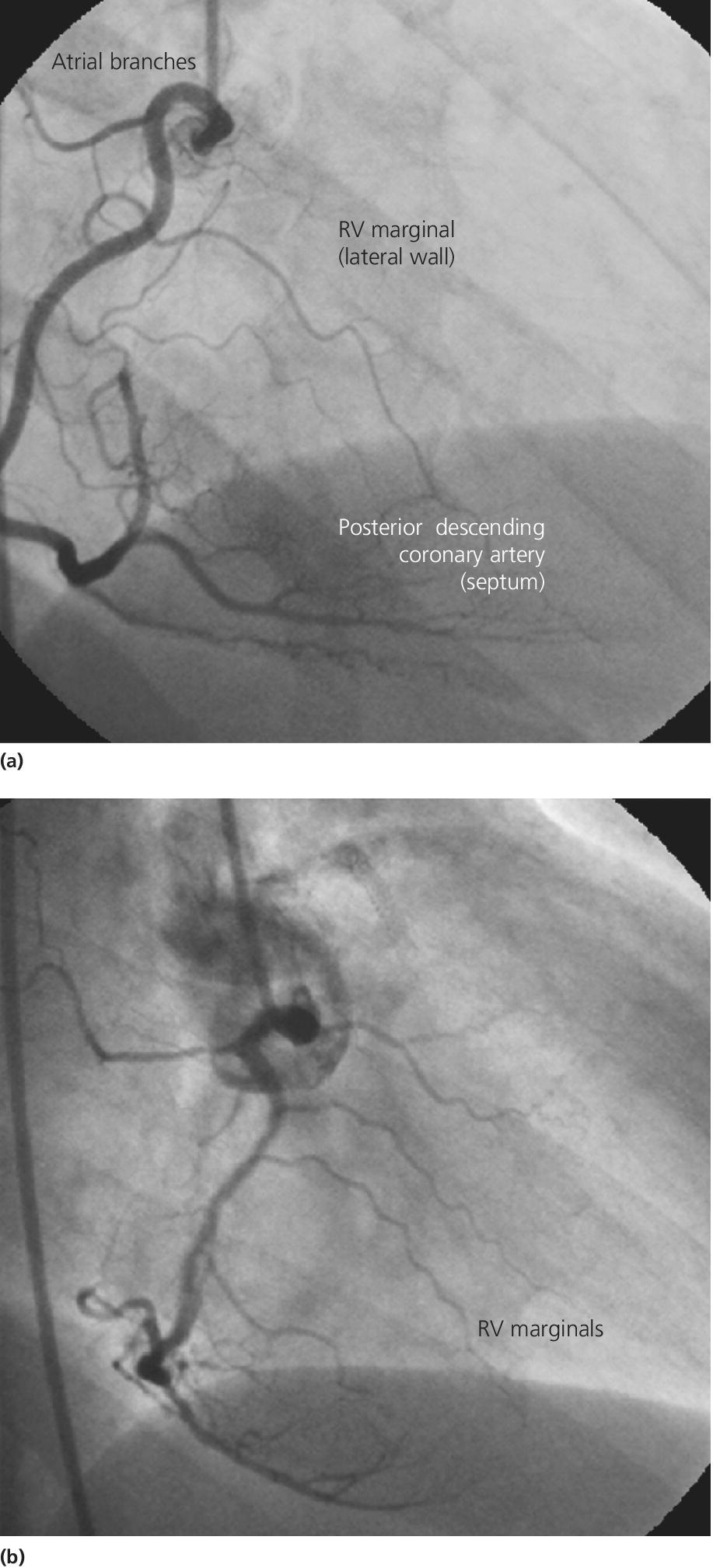
CHAPTER 25 Robert V. Kelly, Mauricio G. Cohen and George A. Stouffer Right ventricular (RV) dysfunction occurs to some degree in approximately 30–50% of inferior wall and 10% of anterior wall infarcts. Severe RV dysfunction leading to the classic hemodynamic changes occurs in approximately 10% of inferior myocardial infarctions and is associated with higher rates of mortality, cardiogenic shock, sustained ventricular arrhythmias, and advanced atrioventricular (AV) block. Patients in cardiogenic shock with RV involvement have significantly higher in‐hospital mortality compared to patients without RV involvement. While RV dysfunction during acute arterial occlusion has classically been labeled RV infarction, profound RV ischemia may be more accurate, since patients with RV infarctions who survive their initial hospitalization tend to do well in the long term and RV function generally recovers. The RV is pyramidal shaped with a triangular base and a thin crescentic free wall. It is designed as a volume pump ejecting into the low‐resistance pulmonary circulation. The RV is less susceptible to ischemia than the left ventricle (LV) for two reasons: oxygen demand is less and the blood supply is more redundant. Oxygen demand is lower due to the smaller muscle mass of the RV (approximately 15% of muscle mass of LV), lower preload, and lower afterload. Less oxygen extraction at rest means that the RV has greater extraction reserve during stress. The RV receives its blood supply from several sources. The septum is perfused by the left anterior descending (LAD) artery and posterior descending artery, the lateral wall by marginal branches of the right coronary artery (RCA), and the anterior wall by the conus branch of the RCA and the moderator branch artery of the LAD. The RV is also thought to receive oxygen directly from the ventricular cavity by diffusion. Coronary perfusion to the RV occurs approximately equally during systole and diastole, both under normal conditions and with collateral perfusion during RCA occlusion. RV perfusion during systole is greater than LV perfusion because of lower systolic intramyocardial pressure and less diastolic intracavitary pressure. The vast majority of RV infarcts occur with occlusion of the RCA, although the LAD and circumflex can also cause RV infarcts. There is a large interindividual variation in the number and origin of RV branches from the RCA (Figure 25.1), but a direct correlation exists between more proximal occlusion of the RCA occlusion and a larger extent of RV infarction. Figure 25.1 Right ventricular blood supply. Panel (a) is an AP cranial projection of RCA demonstrating RA branches, a large RV marginal branch, and the posterior descending coronary artery. Panel (b) is an RAO projection of RCA from a different patient and demonstrates several RV marginal branches originating from the mid‐portion of the RCA. From this angiogram, it is easy to see that the more proximal the occlusion in the RCA, the greater the extent of RV ischemia. The diagnosis of RV myocardial infarction is made using the clinical presentation in combination with echocardiogram (ECG), echocardiographic, and/or hemodynamic criteria. The classic clinical triad described with RV infarction is hypotension, clear lung fields, and elevated jugular venous pressure in the setting of an inferior wall myocardial infarction. The ECG with right‐sided leads is very useful in the diagnosis of RV myocardial infarction. The sensitivity of ST elevation in V4R, V3R, and V1 is 93%, 69%, and 28%, respectively, while the specificity is 95%, 97%, and 92%. Echocardiographic findings that support the diagnosis of RV infarction include RV dilation, RV wall motion abnormalities, paradoxical motion of the interventricular septum, tricuspid regurgitation, decreased descent of the RV base, and plethora of the inferior vena cave (IVC). In proximal RCA occlusion there is compromised perfusion to the RV free wall, with RV dyskinesis and depressed RV function, which is reflected in the RV waveform as a sluggish upstroke, depressed broadened systolic peak, delayed relaxation phase, and diminished RV stroke work (Figure 25.2). RV systolic dysfunction reduces transpulmonary delivery of LV preload, leading to decreased cardiac output despite intact LV contractility. RV dysfunction is compensated for by augmented RA contraction and by left ventricular septal contraction, which bulges in piston‐like fashion into the RV during systole and generates force against a stiff RV free wall. Figure 25.2 RV pressure tracing in a patient with RV ischemia.
Right ventricular myocardial infarction
The effects of ischemia on the right ventricle
Clinical presentation, ECG changes, and echocardiographic findings in RV infarction
Hemodynamics of RV infarction

Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


