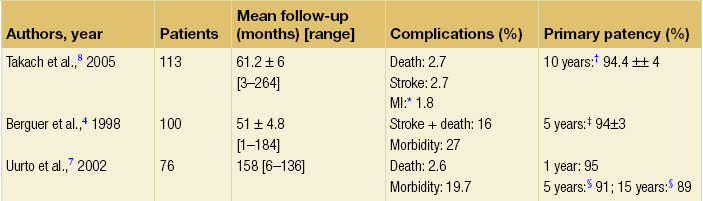
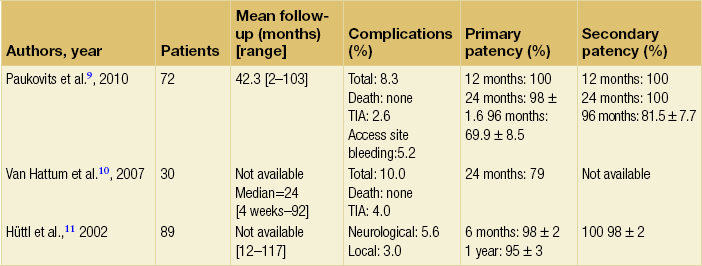
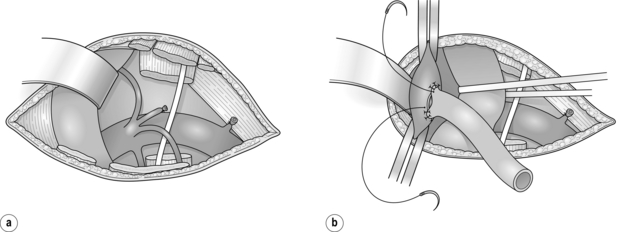
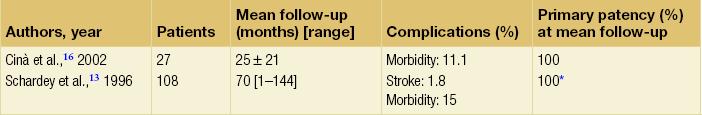
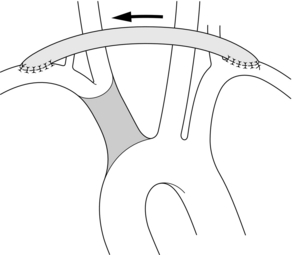
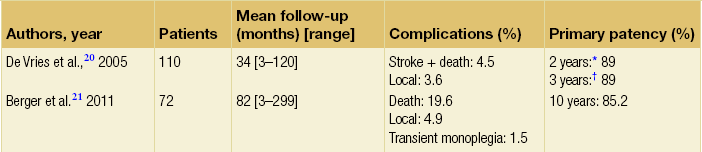
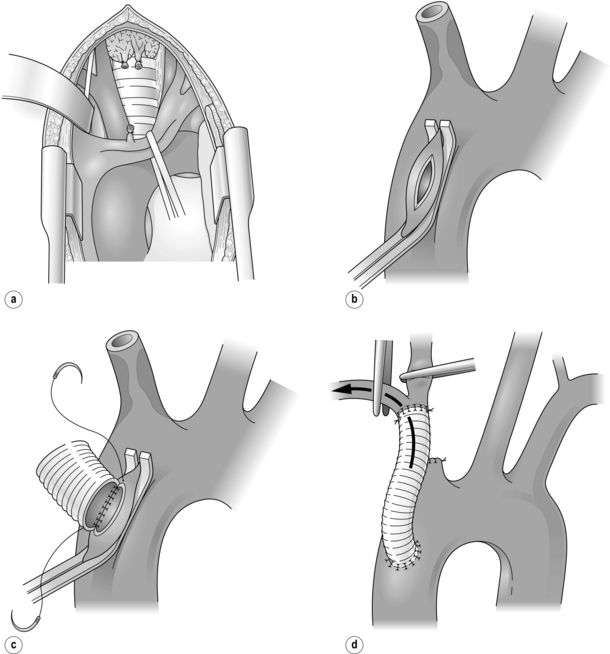
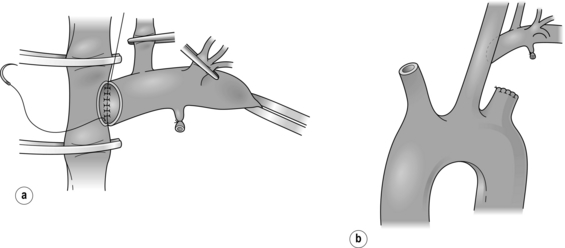
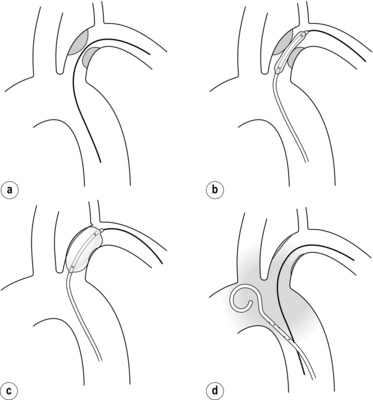
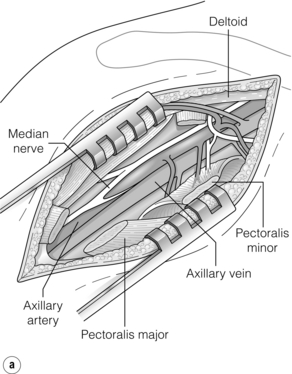
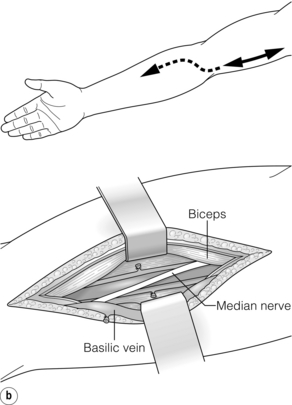
11 Arterial diseases of the upper limb are relatively rare in comparison with those involving the lower extremity. The good collateral supply around the shoulder and elbow explains why chronic occlusive disease is commonly asymptomatic, but acute occlusion due to embolism can result in limb-threatening ischaemia. In addition, thoracic outlet syndrome, axillo-subclavian vein thrombosis and occupational vascular problems need to be considered. In this chapter we do not review vasospastic disorders, connective tissue disease, vasculitis and Raynaud’s disease, as these are covered in Chapter 12, nor vascular trauma, which is covered in Chapter 9. The main causes of upper limb vascular disease are summarised in Box 11.1. Occlusive lesions of the brachiocephalic and subclavian arteries occur in relatively young patients with mean ages ranging from 50 to 60 years. These lesions are much less frequent than those involving the carotid bifurcation.1 Atherosclerosis is the predominant cause in Europe, with Buerger’s disease and Takayasu’s arteritis seen rarely. The symptoms of occlusive disease of the upper extremities include muscle fatigue and ischaemic rest pain. Digital necrosis or atheroembolisation is less common than in the lower extremities, accounting for no more than 5% of patients with limb ischaemia.2 Stenotic lesions of the brachiocephalic artery are uncommon and may be asymptomatic in 13–22% of patients.3,4 Symptomatic patients may present with ischaemia of the right upper extremity, carotid territory symptoms or vertebrobasilar symptoms.5 The diagnosis is suspected by physical examination (i.e. right supraclavicular/cervical bruit, absent right subclavian or axillary pulse) and confirmed by duplex scanning, conventional angiography, or computed tomography (CT) or magnetic resonance angiography (MRA). Most patients (61–84%) with brachiocephalic artery occlusion have multiple lesions of the aortic arch vessels.6 Stenotic lesions of the brachiocephalic artery may be approached by median sternotomy with direct bypass grafting from the aortic arch, or indirectly by extra-anatomical bypass such as subclavian–subclavian, contralateral carotid–carotid or subclavian–carotid bypass. A median sternotomy is used with extension into the neck. The left brachiocephalic vein is identified (Fig. 11.1a). A partial occluding clamp is applied to the ascending aorta proximal to the brachiocephalic artery in order to avoid the risk of fracturing atheromatous plaque (Fig. 11.1b). An 8–10 mm prosthetic graft is anastomosed at this site with deep suture placement in the aortic wall (Fig. 11.1c). Once the anastomosis is completed, a clamp is applied across the graft and systemic heparin is given. The brachiocephalic artery is clamped, sectioned and the proximal stump oversewn. The patent distal artery is spatulated and the graft attached in an end-to-end fashion (Fig. 11.1d). Air is evacuated from the graft by back-bleeding the subclavian artery, then flow is released into the arm and then into the carotid artery. The mortality of direct bypass ranges from 5.8% to 8% in Kieffer’s and Berguer’s series, with a primary patency rate at 5 years of 94% in both series. Figure 11.1 (a) The left brachiocephalic vein is retracted to expose the brachiocephalic artery. (b) A clamp is applied laterally to the ascending aorta. (c) A polyester graft is implanted on the ascending thoracic aorta proximal to the brachiocephalic artery. (d) Completed bypass. Flow is released into the arm and then into the common carotid artery. Percutaneous transluminal angioplasty (PTA) and stenting of the brachiocephalic artery is being performed with increased frequency. The approach may be percutaneous from either the femoral or brachial artery or through an anterolateral cervical approach with clamping of the right common carotid artery to avoid atheroembolisation during the angioplasty. Because of a relatively small number of cases, most papers concerning angioplasty of the brachiocephalic artery include results for the subclavian artery. Only three series report PTA of the brachiocephalic artery alone9–11 (Table 11.2). The benefit of adjuvant stenting is not well established.9,10 Open surgery gives better mid-term results but angioplasty is much less invasive. Symptomatic lesions of the subclavian artery are associated in 72% of cases with concomitant lesions of carotid and vertebral vessels.1 The indications for intervention are those of vertebrobasilar insufficiency and marked upper extremity ischaemia. Atheroembolisation is quite common in this location.12 If surgery is contemplated and the ipsilateral common carotid artery is healthy, carotid–subclavian bypass or carotid–subclavian transposition is the method of choice. Access is achieved by a horizontal supraclavicular incision with division of both heads of the sternomastoid muscle. Scalenus anterior and the phrenic nerves are exposed, and then scalenus anterior is divided near its insertion into the first rib (Fig. 11.2a). On the left side, the thoracic duct is ligated. The carotid sheath is opened, safeguarding the vagus nerve. After heparinisation, the common carotid artery is clamped as low as possible. A vein or polytetrafluoroethylene (PTFE) graft is then anastomosed to the lateral aspect of the common carotid artery in an end-to-side fashion (Fig. 11.2b). Use of a prosthetic graft seems to give better results than the vein graft in this location.13 The graft under arterial tension is then passed behind the jugular vein. Graft length should be cautiously estimated and the graft anastomosed end-to-side to the superior aspect of the distal subclavian artery. If the proximal subclavian lesion is ulcerated, it should be excluded by proximal ligation. If the distal subclavian artery is too diseased for distal implantation, the graft should be passed behind the clavicle and implanted on the axillary artery exposed via a short infraclavicular incision. Reimplantation of the subclavian artery into the common carotid artery is an alternative that avoids graft material but requires a more extensive cervical dissection. Dissection should avoid the recurrent laryngeal nerve, which is closely related to the posterior aspect of the subclavian artery. A curved clamp is applied across the subclavian artery, which is transected and the proximal stump oversewn. The site of anastomosis to the common carotid artery should be chosen to avoid kinking and angulation of the vertebral artery. The clamps on the common carotid artery should be rotated anteriorly to present the posterolateral surface for anastomosis with the subclavian artery (Fig. 11.3). An ellipse is excised from the wall of the common carotid artery and the subclavian artery anastomosed in end-to-side fashion. Figure 11.3 Carotid–subclavian transposition: (a) clamps on the common carotid artery are rotated anteriorly to present the posterolateral surface for anastomosis with the subclavian artery; (b) end-to-side anastomosis completed. Subclavian revascularisation may also be achieved by crossover subclavian–subclavian or axilloaxillary bypass. These grafts are relatively simple to construct, although their greater length and reversed angle of take-off may reduce durability. Furthermore, problems may arise if subsequent median sternotomy is needed for coronary bypass. The donor and recipient arteries are exposed by a short supraclavicular incision on either side (Fig. 11.4). A tunnel is created from one side of the neck to the other passing behind the sternomastoid muscles and anterior to the carotid vessels. Crossover axilloaxillary bypass is easier to perform but the graft has to pass subcutaneously over the sternum, with risks of compression or erosion. The postoperative death rate for crossover axilloaxillary bypass is 1.6% with a 5-year primary patency of 86.5% in the series of Mingoli et al.19 PTA of subclavian artery stenoses is a relatively safe and often simple procedure to perform. Access is usually obtained from the femoral artery or from the brachial artery and the lesion dilated to 5–8 mm (Fig. 11.5). Because there is usually retrograde flow in the vertebral artery, stroke is rare. When there is not retrograde flow, an occlusion balloon may be placed in the vertebral artery from the arm while the stenosis is dilated. Simple stenoses are adequately dilated by balloon. Occlusions are more difficult to cross and less frequent in most endovascular series;20,21 they often require catheterisation from the brachial artery with the use of balloon or self-expandable stents. Figure 11.5 Retrograde approach from the brachial artery by percutaneous puncture, or cut-down if stenting is necessary: (a) the guidewire is placed through the subclavian stenosis; (b) balloon is advanced over the guidewire and balloon angioplasty performed; (c) arteriography completed by withdrawing the balloon with the same catheter; (d) more accurate arteriographic control can be achieved by using a second transfemoral pigtail catheter positioned in the aortic arch. From Schneider PA. Endovascular skills, 2003. Reproduced by permission of Informa Healthcare. Patients with chronic atherosclerotic occlusion of the axillary or brachial arteries usually present with fatigue on using the arm. Many of these patients have radiation-induced occlusive disease. Severe ischaemia with rest pain or digital necrosis is uncommon unless there have been repeated episodes of embolism due to proximal ulceration or aneurysmal degeneration. Direct reconstructive surgery is feasible since the occlusive lesions tend to be segmental with preserved distal patency. Axillobrachial occlusions can be managed by a bypass procedure if symptoms justify it. These sites can usually be approached by limited incisions and the bypass tunnelled subcutaneously between the two incisions (Fig. 11.6). Autogenous saphenous vein is the preferred graft material. When unavailable, the basilic or cephalic vein may be considered. Upper limb bypass using saphenous vein has a 5-year patency rate of 60–90%.22 PTFE has a lower patency rate at this level. Figure 11.6 (a) Axillary artery approach. The pectoralis minor muscle is divided and the neurovascular bundle is exposed. If access to the axillobrachial junction is needed, the pectoralis major tendon should also be resected. (b) Brachial artery approach. Incision along the medial border of the biceps. If necessary, the bicipital aponeurosis is divided to expose the brachial artery division. The causes of chronic occlusion in the forearm or hand vessels include atherosclerosis, Buerger’s disease, immunological and connective tissue disorders (see Chapter 12), and occupational trauma. Arch angiography, to exclude proximal embolic disease, and selective arteriography are essential in evaluating these patients with distal disease. Most of these patients with distal disease and severe digital ischaemia can be managed conservatively. Avoidance of cold and abstinence of tobacco are essential. Vasodilator or sympatholytic agents may also be employed. Patients with digital necrosis may require local debridement or amputation if gangrene is extensive. Some patients with radial, ulnar or palmar arch occlusion and critical ischaemia may be managed, if run-off is present, by vein graft bypass using microsurgical techniques. Cervicodorsal sympathectomy by thoracoscopy may also be considered in patients with severe distal forearm ischaemia. However, results of sympathectomy have often been disappointing, particularly in patients with diffuse arteritis. True aneurysms of the upper limb arteries are uncommon. The subclavian artery is the most frequent site, usually caused by thoracic outlet compression. These patients may present with distal ischaemia, embolisation or acute thrombosis. False aneurysms from trauma or infection often produce motor or sensory impairment as a result of brachial plexus compression. Subclavian artery aneurysms are best managed by a combined supraclavicular and infraclavicular approach (see later). Aneurysms of the brachiocephalic artery are rare. In the series of Kieffer et al.23 the perioperative death rate was 11%, most deaths occurring in patients operated in an emergency setting. An aberrant right subclavian artery arising from the descending thoracic aorta is a common anomaly. Rarely, the artery compresses the oesophagus against the trachea, producing a condition described as dysphagia lusoria. Aneurysmal degeneration, known as Kommerell’s diverticulum, may also occur. The largest experience has been reported by Kieffer et al.24 Because of the possibility of rupture, resection of the aneurysmal artery with aortic prosthetic reconstruction via a thoracic approach is recommended. As this technique carries a high postoperative mortality, hybrid procedures with aortic stent grafts are feasible. Axillary artery aneurysms are usually caused by blunt or penetrating trauma. Degenerative or congenital aneurysms are rare in this location. False aneurysms of the axillary artery occur with humeral fractures and anterior dislocation of the shoulder. These aneurysms can lead to neurological complications because of compression of the brachial plexus. Duplex scan and arteriography allow an accurate diagnosis. The axillary artery is exposed by a deltopectoral incision with division of the pectoralis minor. The aneurysm is resected followed by interposition of a reversed saphenous vein graft. Stent grafts have been used for emergency control of upper limb aneurysms but their long-term integrity is often compromised by compression between the first rib and clavicle or by excessive arterial flexion.25
Vascular disorders of the upper limb
Introduction
Occlusive disease
Brachiocephalic artery
Aorto-brachiocephalic bypass
Endovascular treatment
Subclavian artery
Carotid–subclavian bypass
Carotid transposition
Crossover grafts
Endovascular treatment
Upper arm arteries
Lower arm and hand arteries
Aneurysmal disease
Upper arm artery aneurysms
Vascular disorders of the upper limb