Varicose Veins
ANDREA T. OBI and THOMAS W. WAKEFIELD
Presentation
A 47-year-old man with no significant past medical history presents to your office complaining of right leg pain and swelling with prolonged standing. Results of the physical examination are normal, except for large, bulging varicose veins (Fig. 1) and edema of the right lower extremity.

FIGURE 1 Symptomatic varicosities.
Differential Diagnosis
Leg edema can be caused by a pathophysiologic process limited to the leg or by a systemic process. Systemic processes responsible for lower extremity edema, which is generally bilateral, include organ failure (heart, liver, kidney), certain medications, and paralysis and muscle atrophy resulting in prolonged periods of extremity dependency. Lymphedema can cause unilateral or bilateral leg swelling.
Swelling may be the result of varicose veins alone or may be attributable to deep venous pathology that can coexist with varicose veins. Thrombosis and congenital anomalies can cause deep venous obstruction and deep venous insufficiency; both of these latter conditions can be associated with unilateral or bilateral edema, with or without varicose veins. The symptoms of deep venous pathology are similar to those associated with varicose veins caused by superficial venous insufficiency, but the treatment of these entities is different.
Discussion
The edema that results from organ failure, paralysis, muscle atrophy, prolonged extremity dependency, or medications can generally be ruled out by a thorough history and physical examination. Unlike the “pitting” edema associated with venous insufficiency, which begins in the ankles and calves, the “nonpitting” edema of lymphedema begins in the dorsum of the foot, usually involves the toes, and progresses proximally with time. The skin of a lymphedematous limb is characterized by a peau d’orange appearance and papillomas. The skin associated with superficial venous insufficiency and varicose veins can show no changes at all or can display lipodermatosclerosis and stasis pigmentation changes in the gaiter region.
The etiology of varicose veins is the result of three pathophysiologic states: valvular insufficiency, obstruction, or calf pump malfunction. Valvular insufficiency occurs most frequently in the superficial system and is associated with development of varicose veins. The most commonly affected veins include the great saphenous (70% to 80%) followed by small saphenous (15% to 20%) and nonsaphenous (10%). Increasing severity of symptoms occurs with involvement of more than one venous system. Chronic reflux results in transmission of high venous pressures to the lower leg while standing. Valvular insufficiency occurs as the valve becomes elongated and floppy or by dilation of the valvular ring. Deep venous thrombosis accounts for half of the cases of deep vein valvular dysfunction due to vein wall fibrosis and valve scarring. Other causes of reflux include high levels of estrogen during pregnancy and prolonged standing, which both cause vein dilation.
Venous hypertension can also be the result of an obstruction to blood exiting the lower extremity. Obstruction can be due to a vascular occlusive lesion from a deep venous thrombosis or from nonthrombotic occlusion, such as compression of the left common iliac vein by the right common iliac artery (May-Thurner syndrome).
The diagnosis of chronic venous disease begins with a thorough history and physical exam. Severity of illness is categorized by the Clinical, Etiology, Anatomy, Pathophysiology (CEAP) (Table 1) and Venous Clinical Severity Scoring System (VCSS) (Table 2). Venous duplex ultrasonography is capable of detecting both deep and superficial venous thrombosis or insufficiency. In our practice, duplex imaging is performed on all patients presenting with venous disease. The patient is positioned standing with weight on the contralateral limb. The standing position allows for filling of the deep venous system and accentuates the hydrostatic effects of venous insufficiency. The deep venous system is assessed for acute and chronic disease. If acute deep venous thrombosis (DVT) is discovered, the investigation is ended. If there is not a DVT, the pulse wave Doppler is performed during Valsalva and during distal compression if possible, and time of reflux is measured. Duration of valve closure greater than 500 ms (0.5 seconds) in the superficial or perforator veins is considered pathologic (Fig. 2). Retrograde flow in the deep veins of up to 1000 ms (or 1.0 seconds) is considered normal. Importantly, reflux should be determined in all the veins including the great saphenous, small saphenous, accessory saphenous, common femoral, popliteal, and perforating veins. Such a practice will prevent missed pathologic refluxing veins and will provide the surgeon with a “road map” of disease. In a review of 1091 patients, we discovered 30% to have reflux in locations other than the saphenofemoral junction. Oftentimes, venous duplex represents the only imaging study necessary to determine appropriate treatment.
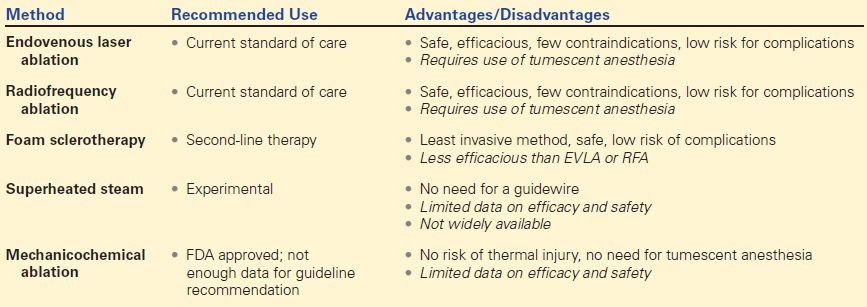
TABLE 1. CEAP
Adapted from Eklöf B, Rutherford RB, Bergan JJ, et al. American Venous Forum International Ad Hoc Committee for Revision of the CEAP Classification. Revision of the CEAP classification for chronic venous disorders: consensus statement. J Vasc Surg. 2004;40(6):1248–1252.
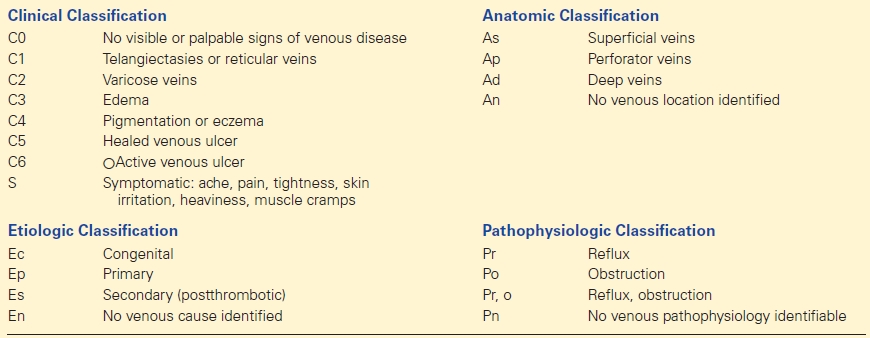
TABLE 2. Revised VCSS
Reprinted with permission from Vasquez MA, Rabe E, McLafferty RB, et al., American Venous Forum Ad Hoc Outcomes Working Group. Revision of the venous clinical severity score: venous outcomes consensus statement: special communication of the American Venous Forum Ad Hoc Outcomes Working Group. J Vasc Surg. 2010;52(5):1387–1396.
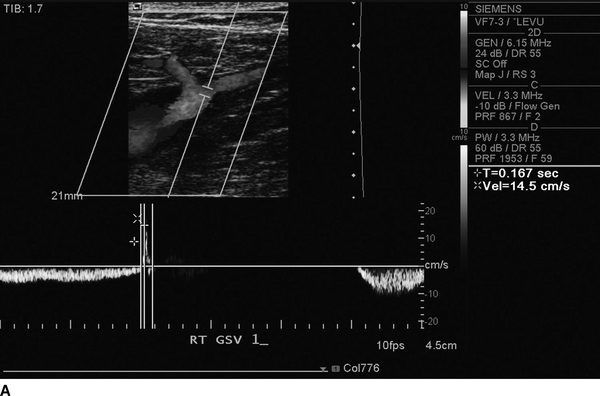
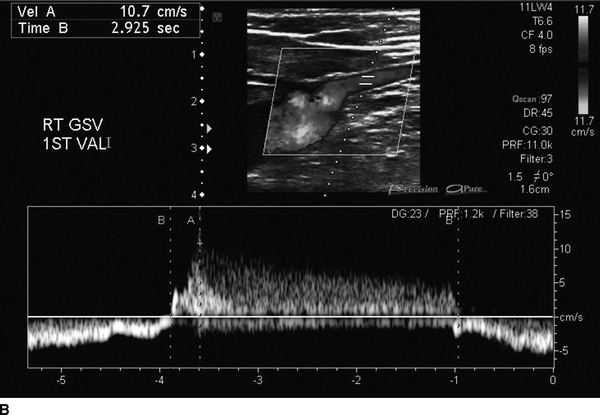
FIGURE 2 Duplex ultrasonography demonstrating competent (A) great saphenous vein and refluxing (B) great saphenous vein.
Recommendation
Venous Duplex Ultrasound
Venous Duplex Ultrasound Report
The right great saphenous vein displays saphenofemoral reflux (duration longer than 0.5 second). No significant reflux is noted in the left lower extremity. No reflux or obstruction is noted in the deep venous system.
Diagnosis and Recommendation
The venous duplex ultrasound shows the etiology of the patient’s varicose veins to be saphenofemoral reflux in the right lower extremity. The first line of treatment is compression therapy; intermittent leg elevation; exercise such as walking, cycling, and swimming; and protection of the skin barrier. Had the ultrasound shown significant deep venous insufficiency alone or in conjunction with superficial venous insufficiency, the nonoperative management noted above would be the recommended first treatment. In this patient, who has superficial venous insufficiency alone, surgical intervention is indicated if he remains symptomatic, develops a complication, or is unable to wear and tolerate compression therapy.
Surgical Approach
Treatment of Reflux
The widespread adoption of duplex ultrasound and development of endovenous therapies have significantly altered the treatment of varicose veins. The majority of patients presenting with varicosities will have concomitant venous reflux identified on duplex ultrasound. All patients with superficial reflux with a valve closure time of greater than 500 ms should be considered for an antireflux procedure if conservative therapy has not alleviated the symptoms. Currently, the use of endovenous thermal ablation, encompassing radiofrequency ablation (RFA) and endovenous laser therapy (EVLT), is the recommended therapy of choice over traditional open surgery (high ligation and stripping) with a grade 1B by the Society for Vascular Surgery (SVS) and American Venous Forum (AVF) varicose vein guidelines (Table 3). Foam sclerotherapy, while safe, is not as efficacious as is RFA, EVLT, or open surgery and thus is not recommended as first-line treatment for saphenous reflux.
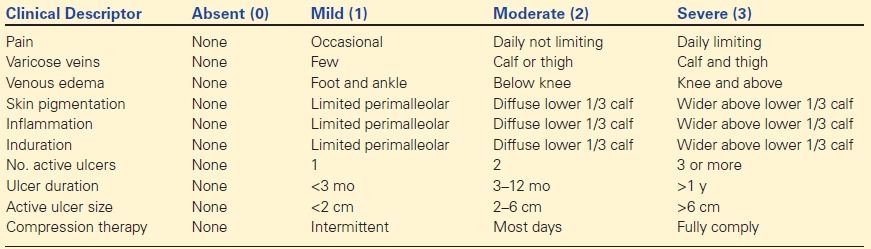
TABLE 3. Methods of Endovenous Ablation