Unilateral Leg Swelling Secondary to Venous Insufficiency
MARGARET CLARKE TRACCI and JULIE ARMATAS
Presentation
A 33-year-old woman with no past medical history presents with pain, swelling, and heaviness of her left leg. She first noticed these symptoms 4 years ago after giving birth to her second child. Her symptoms have progressed over time and are most pronounced at the end of the day or after prolonged standing. She has worn compression stockings for several months with persistence of her symptoms.
Physical examination reveals moderate edema of the left lower leg from midcalf to the ankle and a visible large varicosity traversing the medial thigh and proximal lower leg (Fig. 1). There are scattered telangiectasias and reticular veins around the ankles bilaterally; however, the right leg is without symptoms. The femoral and pedal pulses are palpable, and there are no skin changes noted.

FIGURE 1 Visible large varicosity traversing the medial thigh and proximal lower leg.
Differential Diagnosis
While up to one third of the population is affected by venous disease, there are a variety of pathophyiologic processes that may underlie leg edema. Bilateral lower extremity edema may be systemic in nature, associated with underlying renal, cardiac, or hepatic disease, malnutrition, or inciting medications. Careful review of the patient’s history is necessary to distinguish these.
Lymphedema may cause unilateral or bilateral edema, which is generally nonpitting in nature and involves the toes and dorsum of the foot. The skin often assumes a thickened, peau d’orange appearance. A positive Stemmer’s test, indicated by the inability to pinch and lift a skinfold at the base of the second toe, is typical of lymphedema. Lymphedema may occur in association with venous insufficiency and is, in this setting, called phlebolymphedema.
Venous disease may be unilateral or bilateral and may involve physiologic elements of both obstruction and insufficiency. Symptoms include aching, throbbing, a sensation of heaviness or fatigue of the affected limb, or burning, itching, or “pins and needles” sensation in the skin. These will tend to be more prominent toward the end of the day and after periods of prolonged standing. Elements of patient history, such as female gender, parity, the presence of obesity, and family history of varicose veins, may support the diagnosis. The identification of occlusive disease is essential.
The most common etiology of venous occlusive disease is deep vein thrombosis, which may be provoked or associated with various thrombophilias. External compressive syndromes may result from pelvic or other tumors or from iliac vein compression by the right iliac artery or distal aorta, known commonly as May-Thurner syndrome. Patients may or may not present with the visible varicosities, reticular veins, or telangiectasias commonly associated with venous insufficiency.
Physical examination may demonstrate palpable varicosities or the cords or tenderness of chronic phlebitis. Skin changes associated with venous disease range from hemosiderin deposition to severe lipodermatosclerosis and even skin ulceration, typically in a gaiter distribution. The presence of unsightly veins leads some patients to seek treatment for cosmesis in the absence of significant symptoms. It is important to note that visible telangiectasias, reticular veins, and varicosities may occur in the absence of other symptoms or axial reflux.
Workup
A thorough history and physical exam can typically distinguish systemic, lymphatic, or venous causes of lower extremity edema. When venous insufficiency is suspected, duplex ultrasound (DU) is the inexpensive, noninvasive, and safe workhorse of diagnosis and is useful not only to establish the diagnosis but also to guide treatment and assess outcomes.
Duplex Ultrasound
A thorough venous duplex examination should comprise visualization of both deep and superficial systems as well as assessments of vessel compressibility, flow (including the presence and duration of reflux), and augmentation. The reflux examination is ideally obtained in a standing position, using patient Valsalva to elicit reflux at the common femoral vein, saphenofemoral junction, and more central portion of the greater saphenous vein (GSV) and manual or cuff compression and release to do the same in veins of the distal leg. Pathologic reflux is defined as retrograde flow that lasts greater than 1000 ms in the common femoral, femoral, and popliteal veins (deep system) and greater than 500 ms for the greater and small saphenous veins, the deep femoral vein, tibial veins, and perforating veins.
Plethysmography
Plethysmography provides a physiologic measurement of venous volume or pressure and is used to detect and characterize venous disease. Volume changes, amount of reflux, degree of venous outflow obstruction, and the efficiency of the calf muscle pump can be estimated. The availability of plethysmography has also limited its use in recent years, although it is still felt to be useful in the setting of advanced disease for the clarification of pathophysiology.
Advanced Imaging (CT and MR Venography)
These modalities are used selectively primarily in the evaluation of congenital malformations (primarily gadolinium-enhanced magnetic resonance [MR]) or central pathologies such as thrombotic or nonthrombotic iliocaval obstruction or compressive syndromes such as May-Thurner, pelvic congestion, or nutcracker syndromes (MR or computed tomography [CT]).
Contrast Venography and Intravascular Ultrasound
For patients with complex obstructive or mixed disease, ascending and descending venography may play a critical role in diagnosis and management. It provides physiologic as well as anatomic information regarding both reflux and obstruction as well as the opportunity to treat obstructive disease, particularly in central locations. Intravascular ultrasound can serve as an important adjunct to a catheter-based study or intervention, as it provides excellent data regarding the cross-sectional area of the vein and may be more sensitive in the detection and characterization of compressive or obstructive lesions than contrast venography alone.
Medical Evaluation
In the event of recurrent or unprovoked venous thrombosis, thorough review of patient and family history as well as laboratory investigation for thrombophilia is appropriate.
Results
DU on this patient revealed reflux in the left GSV, greater than 5 seconds. The left GSV measured 5.3 mm, and there was no reflux in the small saphenous vein. These findings led to a diagnosis of left GSV reflux (Fig. 2).
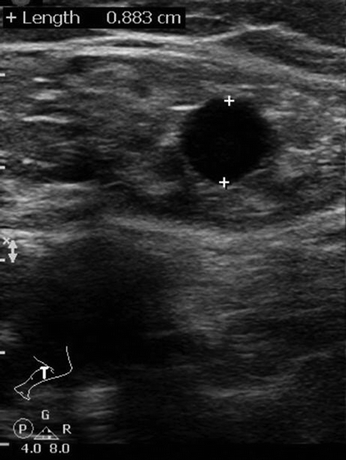
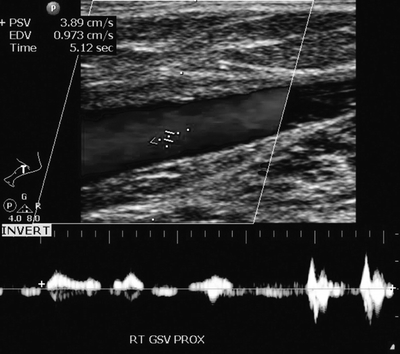
FIGURE 2 Axial view (A) of GSV in sheath and longitudinal view (B) demonstrating reflux.



