Aspirin use for primary prevention in patients at high risk with diabetes mellitus (DM) is often recommended under the assumption that most patients with DM have coronary artery disease (CAD). However, not all patients may have CAD. The present study evaluated, in 425 patients at high risk with DM (without chest pain syndrome or a history of cardiac disease), the prevalence of CAD on coronary computed tomography angiography (CTA). Moreover, the association between the presence and number of traditional cardiovascular (CV) risk factors and CAD (on coronary CTA) was evaluated. The median coronary artery calcium score was 29 (interquartile range 0 to 298). On coronary CTA, 116 patients (27%) had no CAD (defined as <30% stenosis). Of the 309 patients (73%) with any CAD (≥30% stenosis), 35% had obstructive CAD (≥50% stenosis). The number of traditional CV risk factors was not associated with the presence of any CAD (≥30% stenosis; p = 0.18) or obstructive CAD (≥50% stenosis; p = 0.13). Hypertension was the only traditional CV risk factor associated with a higher frequency of any CAD (≥30% stenosis; odds ratio = 2.21, 95% CI 1.43 to 3.41, p <0.001) and obstructive CAD (≥50% stenosis; odds ratio 2.03, 95% CI 1.33 to 3.11, p = 0.001). In conclusion, in patients at high risk with DM without chest pain syndrome, any CAD was ruled out by coronary CTA in 27%, whereas 65% of the patients did not have obstructive CAD. The number of CV risk factors was not associated with the presence of CAD. Hypertension was the only traditional CV risk factor that was associated with a higher frequency of CAD. These observations support potential use of coronary CTA to tailor aspirin therapy in patients at high risk with DM.
The European Society of Cardiology (ESC) guidelines recommend to consider aspirin use for primary prevention in patients at high risk with diabetes mellitus (DM). However, the definition of patients at high risk with DM is not entirely clear. The 2012 ESC guidelines on cardiovascular (CV) disease prevention suggested that patients with DM, and at least one other CV risk factor or target organ damage, should be considered to be at very high risk and all other patients with DM to be at high risk. Traditional risk scores such as the Framingham CV Risk Equation or Systematic Coronary Risk Evaluation were not specifically developed for patients with DM. There have been attempts to design risk engines for patients with DM such as the United Kingdom Prospective Diabetes Study and the Swedish National Diabetes Register, but the applicability of these scores for clinical practice needs further validation. Moreover, current risk engines do not incorporate (noninvasive) imaging tests, which have been shown to be of great value for risk stratification in patients with DM and without DM. Treatment with aspirin has been proved to reduce CV events in secondary prevention (in patients with coronary artery disease [CAD]). However, the efficacy and safety in primary prevention are still unclear and need more research. Patients with DM often have (severe) CAD, but are frequently free of chest pain symptoms. However, not all patients with DM have CAD. Therefore, it is important to identify which patients at high risk with DM are free of CAD and may not need aspirin. Assessment of CAD on coronary computed tomography angiography (CTA) could be of value over established traditional CV risk factors to identify patients without CAD who do not need aspirin. Therefore, aims of this study were: (1) to investigate the prevalence of CAD on coronary CTA and (2) to evaluate the association between the presence and number of traditional CV risk factors and the presence of CAD on coronary CTA in patients at high risk with DM without chest pain syndrome.
Methods
The population consisted of 448 patients with DM without chest pain syndrome who were clinically referred for coronary CTA for evaluation of CAD. The inclusion criteria were (1) a diagnosis of type 1 or 2 DM, (2) the absence of chest pain syndrome defined as atypical or typical angina, and (3) one or more traditional CV risk factors besides DM. The risk factors included hypercholesterolemia (defined as a self-reported history of hypercholesterolemia and/or therapeutic treatment with lipid-lowering drugs), hypertension (defined as the self-reported history of hypertension and/or the use of antihypertensive medication, or systolic blood pressure ≥140 mm Hg and/or diastolic blood pressure ≥90 mm Hg), family history of CV disease, current smoker, and obesity (body mass index ≥30 kg/m 2 ). Patients with a history of CAD (history of myocardial infarction [MI], percutaneous coronary intervention, or coronary artery bypass graft surgery), heart failure, valvular heart disease, arrhythmia, or congenital heart disease were excluded.
Demographic data were prospectively entered into the departmental Cardiology Information System (EPD-Vision; Leiden University Medical Center, Leiden, the Netherlands) and retrospectively analyzed. For retrospective analysis of clinically acquired data, the institutional review board waived the need for patient written informed consent.
Coronary CTA was performed using a 64- or 320-detector row computed tomography scanner (64-slice Aquillon 64, Toshiba Medical Systems, Otawara, Japan and 320-slice Aquillon ONE). Data acquisition protocol has been previously described. In summary, a nonenhanced and contrast-enhanced CT scans were performed. Postprocessing of scans was performed with dedicated software (Vitrea FX 1.0; Vital Images, Minnetonka, Minnesota). Uninterpretable scans were excluded from the analysis.
The coronary artery calcium (CAC) score was performed according to the algorithm of Agatston, which was categorized in four risk categories 0, 1 to 100, 101 to 400 and, >400. All coronary CTAs were analyzed, according to the modified 17-segment American Heart Association classification. Only segments which were interpretable (no severe motion artifacts) with a diameter of ≥1.5 mm were analyzed. Structures >1 mm 2 within and/or adjacent to the vessel lumen that could be discriminated from surrounding pericardial tissue, epicardial fat and the vessel lumen itself were defined as plaque. The severity of coronary stenosis in each segment was classified by visual estimation in 5 categories: no stenosis, stenosis 1% to 29%, stenosis 30% to 49%, stenosis 50% to 70%, and stenosis ≥70%. Coronary plaques were stratified into 3 groups: calcified (plaque containing ≥50% calcified tissue), mixed (plaque containing <50% calcified tissue), and noncalcified (plaque containing no calcified tissue). Importantly, 2 separate analyses were performed based on (1) the presence of “any CAD” which was defined as at least one stenosis ≥30% in any vessel, and (2) the presence of “obstructive CAD” which was defined as at least one stenosis ≥50% in any vessel.
Normally distributed variables were expressed as mean ± SD and nonnormally distributed variables as median and interquartile range. Categorical variables were expressed as frequencies. First, the distribution of any CAD (≥30% stenosis) in patients with a CAC score of 0 and >0 was assessed. Second, the association between the number of CV risk factors and the presence of any CAD (≥30% stenosis) was evaluated. Patients were stratified into 1, 2, 3, and ≥4 traditional CV risk factors. The prevalence of any CAD (≥30% stenosis) in each category was investigated with the Fisher’s exact test. The effect of the number of traditional CV risk factors on the presence of any CAD (≥30% stenosis) was assessed with logistic regression analysis. Third, the association between the several traditional CV risk factors and the presence of any CAD (≥30% stenosis) was investigated. Patients were stratified according to the presence of several traditional CV risk factors: hypertension, hypercholesterolemia, family history of CAD, current smoker, and obesity. The prevalence of any CAD (≥30% stenosis) in each CV risk factor was assessed. The association between the several traditional CV risk factors and the presence of any CAD (≥30% stenosis) was assessed with the Fisher’s exact test. Similarly, the analyses were repeated for the presence of obstructive CAD (≥50% stenosis). A 2-sided p value <0.05 was considered statistically significant. All analyses were performed with SPSS software, version 22.0 (IBM Corp., Armonk, New York).
Results
The clinical characteristics of the patients are provided in Table 1 ; 23 patients (5%) were excluded because of poor coronary CTA quality. The final population consisted of 425 patients at high risk with DM without chest pain syndrome (mean age 56 ± 11 years, 57% men). Referral for coronary CTA included nonspecific chest pain/symptoms (16%), high-risk profile (81%), abnormal electrocardiogram (2%), and preoperative screening (1%).
| Variable | All Patients (n=425) |
|---|---|
| Men | 243 (57%) |
| Age (years) | 56 ± 11 |
| Height (meter) | 1.72 ± 0.10 |
| Weight (kg) | 86 ± 18 |
| Diabetes mellitus (type 2) | 346 (81%) |
| BMI ≥ 30 (kg/m 2 ) | 156 (37%) |
| Family history of CV disease | 173 (41%) |
| Hypercholesterolemia ∗ | 244 (57%) |
| Hypertension † | 254 (60%) |
| Current smoker | 98 (23%) |
| Number of additional CV risk factors ‡ | |
| 1 | 131 (31%) |
| 2 | 138 (32%) |
| 3 | 109 (26%) |
| ≥ 4 | 47 (11%) |
| Medication use | |
| Ace-inhibitor/AT II | 219 (52%) |
| Statin | 273 (64%) |
| Betablocker | 71 (17%) |
| Calciumantagonist | 50 (12%) |
| OAC/Clopidogrel/Persantin/Aspirin | 118 (28%) |
∗ Defined as a self-reported history of hypercholesterolemia, and/or therapeutic treatment with lipid-lowering drugs.
† Defined as a self-reported history of hypertension, systolic blood pressure ≥140 mm Hg and/or diastolic blood pressure ≥90 mm Hg, and/or the use of antihypertensive medication.
‡ Additional CV risk factors consisted of family history of CV disease, hypercholesterolemia, hypertension, obesity, and current smoker.
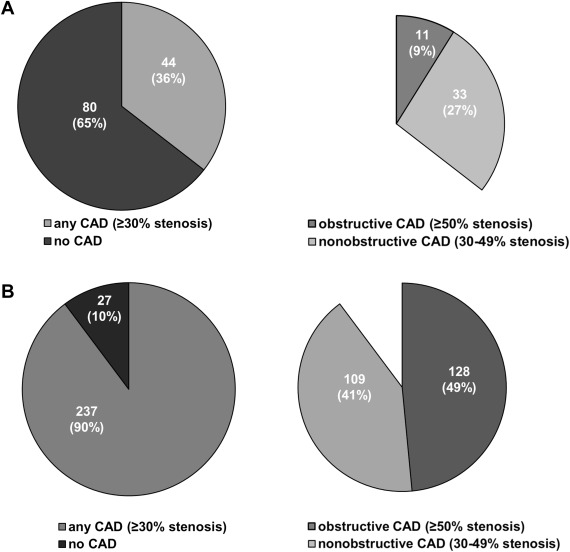
A CAC score was performed in 388 patients (91%). The median CAC score was 29 (interquartile range 0 to 298). As depicted in Figure 1 , a CAC score of 0 was observed in 124 patients (32%). Of these patients, 44 patients (35.5%) had any CAD (≥30% stenosis), of which 11 patients (9%) had obstructive CAD (≥50% stenosis). In the 264 patients (68%) with a CAC score >0, any CAD (≥30% stenosis) was observed in 237 patients (90%), of which 128 patients (48.5%) were obstructive CAD (≥50% stenosis; Figure 1 ).
Coronary CTA results are presented in Table 2 ; the prevalence of any CAD (≥30% stenosis) was 73%. A coronary artery stenosis of 30% to 49% was observed in 160 patients (38%) and a coronary artery stenosis ≥50% in 149 patients (35%). Importantly, 116 patients (27%) presented with a normal coronary CTA (no or <30% stenosis). The mean number of calcified segments was 1 ± 2, the mean number of segments with mixed plaque was 2 ± 2 and on average 1 ± 2 segments had noncalcified plaque.
| Variable | Patients |
|---|---|
| CAC scoring | (n=388) |
| CAC score, Agatston | 29 (IQR 0-298) |
| CAC classification | |
| 0 | 124 (32%) |
| 1-100 | 118 (31%) |
| 101-400 | 63 (16%) |
| > 400 | 83 (21%) |
| Coronary CTA findings | (n=425) |
| Coronary stenosis | |
| no stenosis | 54 (13%) |
| stenosis <30% | 62 (14.5%) |
| stenosis 30-49% | 160 (37.5%) |
| stenosis 50%-69 | 119 (28%) |
| Stenosis ≥ 70% | 30 (7%) |
| Coronary plaques composition | |
| No. of calcified plaques | 1 ± 2; 0 (IQR 0-1) |
| No. of mixed plaques | 2 ± 2; 0 (IQR 0-2) |
| No. of non-calcified plaques | 1 ± 2; 0 (IQR 0-1) |
In Figure 2 , the distribution of any CAD (defined as ≥30% stenosis) according to the number of traditional CV risk factors is shown. In patients with one CV risk factor, the prevalence of any CAD (≥30% stenosis) was 66%. In patients with 2, 3, or ≥4 CV risk factors, the prevalence of any CAD (≥30% stenosis) was 73%, 76%, and 81%, respectively. Overall, there was no significant association between the number of traditional CV risk factors and the presence of any CAD (≥30% stenosis; p = 0.18; Figure 3 ). However, there was a significant trend for increasing numbers of traditional CV risk factors and the presence of any CAD (≥30% stenosis; p value for trend 0.03).
Within the various traditional CV risk factors, the prevalence of any CAD (≥30% stenosis) was 73% in patients with hypercholesterolemia compared with 79%, 71%, 80%, and 71% for patients with hypertension, a family history of CAD, current smoker, or obesity, respectively ( Figure 4 ). Only hypertension was correlated with a higher frequency of any CAD (≥30% stenosis; odds ratio [OR] 2.21, 95% CI 1.43 to 3.41, p <0.001; Figure 3 ).
In Figure 2 , also the distribution of obstructive CAD (≥50% stenosis) according to the number of traditional CV risk factors is shown. In patients with one CV risk factor, the prevalence of obstructive CAD (≥50% stenosis) was 27% compared with 36%, 42%, and 36% for patients with 2, 3, or ≥4 CV risk factors. Overall, there was no significant association between the number of CV risk factors and the presence of obstructive CAD (≥50% stenosis; p = 0.13, p value for trend 0.06). However, compared with one CV risk factor, patients with 3 CV risk factors presented significantly more often with obstructive CAD (≥50% stenosis; OR 1.90, 95% CI 1.11 to 3.25, p = 0.02; Figure 5 ). Within the different traditional CV risk factors, the prevalence of obstructive CAD (≥50% stenosis) in patients with diabetes was 38% in patients with hypercholesterolemia compared with 41%, 30%, 42%, and 33% for patients with hypertension, a family history of CAD, current smoker, and obesity, respectively ( Figure 4 ). Comparable to patients with any CAD (≥30%), only hypertension was correlated with a higher frequency of obstructive CAD (≥50 stenosis; OR 2.03, 95% CI 1.33 to 3.11, p = 0.001; Figure 5 ).




