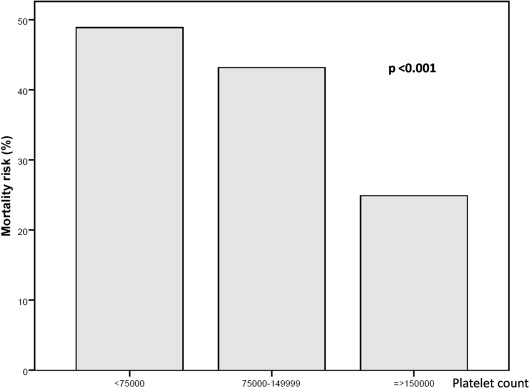
In-hospital mortality of patients with infective endocarditis (IE) remains exceedingly high. Quick recognition of parameters accurately identifying high-risk patients is of paramount importance. The objective of this study was to analyze the incidence and severity of thrombocytopenia at presentation and its prognostic impact in patients with native valve left-sided IE. We studied a cohort of 533 consecutive episodes of native valve left-sided IE prospectively recruited. We distinguished 2 groups: group I (n = 175), episodes who had thrombocytopenia at admission, and group II (n = 358) gathered all the episodes who did not. Thrombocytopenia at admission was defined as a platelet count of <150,000/μl. No differences were found in the need for surgery, but in-hospital mortality was significantly higher in patients with thrombocytopenia (p <0.001). Mortality rate was associated with the degree of thrombocytopenia (p <0.001). In the multivariable analysis, thrombocytopenia at admission was an independent predictor of higher mortality (p = 0.002). A synergistic interaction between thrombocytopenia and Staphylococcus aureus on mortality risk was also observed (p = 0.04). In conclusion, thrombocytopenia at admission is an early risk marker of increased mortality in patients with native valve left-sided IE. Mortality rates increased with increasing severity of thrombocytopenia. Thrombocytopenia at admission should be used as an early marker for risk stratification in patients with native valve IE to identify those at risk of complicated in-hospital evolution and increased mortality.
The objectives of this study were to analyze (1) the incidence and degree of severity of thrombocytopenia at presentation of patients with native valve left-sided infective endocarditis (IE), (2) associated risk factors for its development, and (3) the correlation of thrombocytopenia and clinical outcome in a large cohort of patients with native valve left-sided IE.
Methods
This study was conducted at 3 tertiary care university hospitals with surgical facilities. All centers are using standardized protocols, uniform data collection, and identical diagnostic and therapeutic criteria. From 1996 to 2013, data from 855 consecutive patients with left-sided IE were prospectively recorded on an on-going multipurpose database. For this study, 533 patients with native valve IE were selected. Patients with prosthetic IE were excluded to avoid potential effects of anticoagulation on platelet count. This registry was approved by the local ethical committees, and the study protocol has been carried out in accordance with The Code of Ethics of the World Medical Association (Declaration of Helsinki). Informed consent was obtained for participation in the study. For purposes of analysis and comparison, we distinguished 2 groups: group I (n = 175), episodes who had thrombocytopenia in blood analysis at admission, and group II (n = 358), episodes who did not.
To ensure consecutive enrollment, all patients who underwent an echocardiogram to rule out IE were clinically followed until a diagnosis was established. Duke criteria were applied until 2002 and modified Duke criteria thereafter. To avoid potential source of errors, only definite cases of IE were finally included in the study.
Data collection included a detailed clinical history, standard physical examination, electrocardiography, chest x-ray, blood analysis, urinalysis, a set of 3 blood cultures at admission, and 3 additional blood cultures 48 to 72 hours later, and at least 1 transthoracic and transesophageal echocardiogram. Empiric antibiotic treatment was started after blood cultures were taken, and specific antibiotic therapy was initiated once the results of blood cultures were available. If blood cultures were negative after 72 hours, specific serological tests were done for Chlamydia , Brucella , Q fever, Legionella , Mycoplasma , and Bartonella .
Blood results were systematically collected at presentation to the emergency department. For those patients already hospitalized at the time of infection (nosocomial IE), laboratory parameters (included platelet count) were registered on the date of the first positive blood culture.
Nosocomial and community-acquired IE were defined according to the literature. Acute-onset IE was applied when the time between the appearance of symptoms and hospital admission was <15 days. Under the term of immunosuppression were included patients with HIV and those who were on steroids or other immunosuppressive therapy.
Renal insufficiency was defined as the presence of a serum creatinine concentration >2 mg/dl. Heart failure was diagnosed on the basis of guidelines criteria. Persistent signs of infection, septic shock, and perivalvular complications have been defined in detail elsewhere.
Thrombocytopenia was defined as a platelet count of <150,000/μl. The diagnosis of systemic embolism was based on clinical signs and/or data derived from imaging procedures. Vegetations were measured in various planes, and the greatest diameter was recorded for subsequent analysis. In the case of multiple vegetations, the largest was measured. Surgery was performed when any of the following occurred: heart failure refractory to medical treatment, recurrent embolism with persistent vegetations in the echocardiogram, persistent signs of infection, and fungal endocarditis. When a patient meeting surgical criteria did not undergo surgery, the reason was either because of patient rejection, unacceptably high surgical risk, or when the patient was too frail.
In the univariate analysis, we compared demographic variables, predisposing factors, co-morbidities, microbiologic profile, and outcome of patients with and without thrombocytopenia.
Normally distributed continuous variables are described as a mean value and SD or median (interquartile range [IQR]) when appropriate. In quantitative variables, the groups were compared by a 2-tailed Student’s t test or Mann-Whitney U test when necessary. Categorical variables are expressed as a frequency and a percentage and were compared with the chi-square test or Fisher’s exact test when appropriate. A multivariable regression analysis was done by means of a backward stepwise logistic model. Receiver operating characteristic curve analysis was performed to see prediction of mortality by platelet count and to determine cut-off level for platelet count for determining increased mortality. Interaction between thrombocytopenia and S. aureus infection was explored by 2 multivariable logistic regression analysis calculated by bootstrapping. This interaction was explored in our study sample and also in the whole cohort of left-sided IE.
The adjusted odds ratios with 95% confidence intervals (CIs) for each variable have been calculated. There was no variable with losses surpassing 15%. All tests were 2 sided, and differences were considered statistically significant at p values <0.05. Statistical analysis was performed with PASW Statistics, V 17.0 (SPSS, Inc. Chicago, Illinois).
Results
Mean age of our patient population (n = 533) was 61 ± 15 years, 357 (67%) were men, and 73.1% of the episodes were community-acquired infections. The mean platelet count in the episodes with thrombocytopenia was 98.5 × 10 3 (SD 34 × 10 3 ), whereas in those without thrombocytopenia was 265.7 × 10 3 (SD 127.4 × 10 3 ). Demographic characteristics, co-morbidities, laboratory parameters, and clinical presentation comparisons between patients who had thrombocytopenia (group I) and those who did not (group II) are listed in Table 1 .
| Group I (n=175) | Group II (n=358) | p | |
|---|---|---|---|
| Age (years) | 60.4 (16.5) | 61.7 (15.1) | 0.358 |
| Male | 104 (59.4%) | 253 (70.7%) | 0.010 |
| Community-acquired IE | 120 (68.6%) | 270 (75.6%) | 0.106 |
| Previous valve disease | 73 (43.5%) | 163 (48.7%) | 0.270 |
| Chronic anemia | 38 (21.7%) | 77 (21.7%) | 0.995 |
| Chronic renal failure | 18 (10.3%) | 35 (9.9%) | 0.886 |
| Diabetes mellitus | 35 (20.0%) | 69 (19.4%) | 0.878 |
| Alcoholism | 23 (13.3%) | 37 (10.4%) | 0.329 |
| Chronic obstructive pulmonary disease | 14 (8.0%) | 25 (7.1%) | 0.698 |
| Malignant neoplasia | 21 (12.0%) | 35 (9.8%) | 0.444 |
| Immunosuppression | 28 (16.1%) | 20 (5.7%) | <0.001 |
| Symptoms before admission (days) | 14 (6-41) | 25 (8-60) | 0.371 |
| Acute onset (<15days) | 99 (56.6%) | 119 (31.8%) | <0.001 |
| Fever at admittance | 120 (70.2%) | 261 (74.4%) | 0.312 |
| Heart failure | 59 (33.7%) | 128 (36.3%) | 0.565 |
| Acute renal failure | 45 (26.0%) | 63 (17.8%) | 0.029 |
| Septic shock | 21 (12.2 %) | 16 (4.5%) | 0.001 |
| Chest pain | 15 (8.7%) | 43 (12.2%) | 0.231 |
| Abdominal pain | 26 (15.1%) | 36 (10.2%) | 0.104 |
| Splenomegaly | 26 (15.1%) | 32 (9.1%) | 0.040 |
| Confusional syndrome | 32 (18.4%) | 42 (11.9%) | 0.044 |
| Coma | 12 (6.9%) | 4 (1.1%) | <0.001 |
| Stroke | |||
| Hemorrhagic | 11 (6.3%) | 10 (2.8%) | 0.082 |
| Ischemic | 23 (13.1%) | 40 (11.3%) | 0.119 |
| Systemic embolism | 47 (26.9%) | 71 (20.1%) | 0.080 |
| Hemorrhagic skin lesions | 23 (30.7%) | 17 (13.0%) | 0.002 |
| Hematuria | 4 (2.3%) | 18 (5.1%) | 0.131 |
| Arthritis/Spondylodiscitis | 26 (14.9%) | 57 (16.1%) | 0.721 |
| Second and third degree AV block | 3 (1.7%) | 7 (2.0%) | 0.841 |
| Left bundle-branch block | 5 (2.9%) | 13 (3.7%) | 0.631 |
| Acute myocardial infarction | 1 (0.6%) | 8 (2.3%) | 0.283 |
| Cardiomegaly | 76 (43.7%) | 182 (51.0%) | 0.114 |
| Left heart failure | 59 (33.9%) | 134 (37.4%) | 0.428 |
| Pleural effusion | 43 (25.0%) | 85 (23.7%) | 0.752 |
| C-reactive protein (mg/dl) ∗ | 15.9 (5.10-76.9) | 12.5 (4.6-52.6) | 0.023 |
| Hemoglobin (g/L) | 11.1 (2.3) | 11.0 (2.0) | 0.524 |
| Leukocyte count | 11.2×10 3 (6.7×10 3 ) | 11.9×10 3 (6.8×10 3 ) | 0.546 |
| Neutrophils (%) | 80.5% (12.3) | 77.8% (11.5) | 0.014 |
Concerning co-morbidities, thrombocytopenia was significantly associated with immunosuppression. Antibiotic treatment previous to admittance to the hospital was similarly present in both groups (group 1: 28.9% and group II: 36.7%; p = 0.097).
An acute onset of symptoms was more common in patients with thrombocytopenia. At hospital admission, acute renal failure, septic shock, splenomegaly, confusional syndrome, coma, and hemorrhagic skin lesions were more frequently present in episodes from group I. C-reactive protein (CRP) level was higher in patients with thrombocytopenia.
Staphylococcus aureus and Gram-negative bacilli were more frequently isolated in episodes with thrombocytopenia, whereas infections because of streptococcus viridans were more commonly present in group II ( Table 2 ). Among S. aureus episodes (n = 96), thrombocytopenia was present in 55 (57.3%), whereas in non– S. aureus infections occurred in 120 (27.6%) episodes. High-magnitude bacteremia (≥3 positive blood cultures) was similar in both groups (group I: 55.2% vs group II: 55.0%; p = 0.955).
| MICRO-ORGANISM | Group I (n=175) | Group II (n=358) | p |
|---|---|---|---|
| Streptococcus bovis | 7 (4.0%) | 21 (5.9%) | 0.357 |
| Streptococcus viridans | 16 (9.1%) | 73 (20.5%) | 0.001 |
| Other streptococci | 17 (9.7%) | 34 (9.6%) | 0.952 |
| Enterococci | 16 (9.1%) | 39 (11.0%) | 0.519 |
| Staphylococcus aureus | 55 (31.4%) | 41 (11.5%) | <0.001 |
| Coagulase negative staphylococci | 16 (9.1%) | 44 (12.4%) | 0.271 |
| Gram negative bacilli | 10 (5.7 %) | 7 (2.0%) | 0.021 |
| Fungi | 4 (2.3%) | 3 (0.8%) | 0.226 |
| HACEK Group | 1 (0.6%) | 3 (0.8 %) | >0.999 |
| Anaerobes | 2 (1.1%) | 2 (0.6%) | 0.602 |
| Polymicrobial | 8 (4.6%) | 26 (7.3%) | 0.227 |
| Others | 5 (2.9%) | 18 (5.1%) | 0.242 |
| Culture-negative | 18 (10.3%) | 45 (12.6%) | 0.430 |
Echocardiographic data are listed in Table 3 . Vegetation detection rate and vegetation size were similar in both groups. No differences were found in periannular complications or the degree of valvular regurgitation.
| Group I (n=175) | Group II (n=358) | P | |
|---|---|---|---|
| Location of the infection | |||
| Aortic valve | 90 (51.4%) | 201 (56.1%) | 0.304 |
| Mitral valve | 109 (62.3%) | 217 (44.2%) | 0.863 |
| Mitroaortic valve | 24 (13.7%) | 60 (16.8%) | 0.365 |
| Vegetations | |||
| Detection by TTE/TEE | 161 (93.1%) | 316 (91.1%) | 0.966 |
| Vegetation size (mm) | 15.7 (10.3-23.9) | 13.0 (9.0-19.6) | 0.201 |
| Moderate to severe valvular insufficiency | 142 (82.1%) | 289 (83.3%) | 0.731 |
| Periannular complications | 41 (23.7%) | 84 (24.2%) | 0.898 |
| Abscess | 27 (15.6%) | 46 (13.3%) | 0.467 |
| Pseudoaneurysm | 21 (12.1%) | 53 (15.3%) | 0.335 |
| Fistula | 4 (2.3%) | 10 (2.9%) | 0.705 |
During hospitalization, patients with thrombocytopenia were significantly more likely to be complicated with a stroke and to develop persistent signs of infection and septic shock ( Table 4 ).
| Group I (n=175) | Group II (n=358) | P | |
|---|---|---|---|
| Heart failure | 48 (27.4%) | 93 (26.1%) | 0.735 |
| CNS embolism | 15 (8.6%) | 14 (3.9%) | 0.026 |
| Systemic embolism | 31 (17.7%) | 40 (11.2%) | 0.038 |
| Acute renal insufficiency | 32 (18.3%) | 62 (17.4%) | 0.794 |
| AV block | 9 (5.1%) | 17 (4.8%) | 0.848 |
| Persistent signs of infection+Septic shock | 63 (36.0%) | 94 (26.6%) | 0.025 |
| Cardiac surgery | 96 (54.9%) | 215 (60.1%) | 0.253 |
| Death | 76 (44.7%) | 85 (24.9%) | <0.001 |
No differences were found in the need for surgery, but in-hospital mortality was significantly higher in patients with thrombocytopenia. Overall, 76 of 175 (44.7%) patients with thrombocytopenia died ( Table 4 ). Among thrombocytopenic patients, mortality was lower in those who underwent surgery (35.5% vs 55.8%; p = 0.001). To avoid a potential source of bias because of the selection of patients for surgery, mortality was analyzed separately excluding and including those patients who underwent surgery. Thrombocytopenia was still associated with an increased mortality risk regardless of whether they underwent surgery (35.5% vs 20.7%; p = 0.007) or not (55.8% vs 31.2%; p <0.001). Median time (days) from diagnosis to surgery was similar in both groups (group I: 14 days [IQR 5 to 25.8] and group II: 14 days [IQR 6 to 25.7]; p = 0.981). Even excluding S. aureus infections, thrombocytopenic episodes had higher mortality than those without thrombocytopenia (49 [42.6%] vs 64 [21.2%]; p <0.001). Mortality rate was associated with the degree of thrombocytopenia. Thus, the lower the platelet count, the higher the mortality risk ( Figure 1 ). The difference in mortality according to platelet count was maintained even after excluding S. aureus infections (chi-square TREND : p <0.001). On receiver operating characteristic curve analysis, platelet count was found to be predictive of increased mortality (area under the curve of 0.60) as shown in Figure 2 . A cut-off point of <149,500/μl had a sensitivity of 47% and specificity of 73% in predicting increasing mortality.