After cardiac catheterization procedures, arterial closure can be achieved by manual compression (MC), using external mechanical compression devices, or by applying vascular closure devices (VCDs) with comparable vascular access site–related complication rates. The aim of the present study was to assess vascular access site–related complications during the implementation of structured sheath removal and MC by paramedics after catheterization procedures. After an observational phase of 3 months to assess the baseline complication rate, a structured 4-level training program was implemented to train assistant personnel, in this case paramedics, in the management of sheath removal by MC. Access site–related complication rates after sheath removal were assessed prospectively and MC by paramedics compared with MC by physicians and application of VCDs. To account for imbalances in procedure- and patient-related risk factors of access-site complications, propensity score–based matching analysis was performed ( ClinicalTrials.gov identifier NCT00825331 ). All consecutive percutaneous transfemoral arterial cardiac catheterization procedures were prospectively assessed over a period of 8 months (n = 3,503). MC was performed in 2,315 cases, of which 180 were performed by paramedics and 2,135 by physicians; VCDs were applied in 1,188 procedures. Rates of access site–related complications were significantly lower for paramedics compared with physicians (p = 0.03) and similar between paramedics and VCDs (p = 0.77). In conclusion a structured program for paramedics to be trained in sheath removal after percutaneous cardiac catheterization procedures can be readily implemented during clinical routine with low in-hospital complication rates.
Despite increasing application of radial access for percutaneous arterial catheter procedures, many interventions are still performed via the transfemoral approach, for various reasons. Achieving hemostasis by manual compression (MC) is a time-consuming, unpopular activity for physicians. Alternatives, especially vascular closure devices (VCD), are frequently applied, leading to significant shortening of time to achieve hemostasis and a reduction of access site–related vascular complications at the price of higher costs and sometimes detrimental severe complications, such as vessel occlusions. In Germany, sheath removal and MC are commonly performed by physicians; delegation to assistant personnel remains unusual. We developed a training program tailored for paramedics, enabling them to handle access site and sheath removal after percutaneous arterial procedures independently. Implementation and evaluation of this training program were carried out in the context of the present prospective observational study.
Methods
All consecutive transfemoral catheterization procedures at our clinic were prospectively monitored. After a period of 3 months, to assess baseline complication rates, the structured training program for paramedics was implemented. The study protocol was evaluated and approved by the local ethics committee, and the study design was registered at a public depository ( ClinicalTrials.gov identifier NCT00825331 ).
The training program included 4 risk levels for access site–associated complications, on the basis of anticoagulation status and sheath size. Level 1 included a single platelet aggregation inhibitor and sheath sizes of ≤5Fr, representing the patient group with the lowest expected access site–associated complication rate. In level 2, a sheath size of 6Fr and dual platelet aggregation inhibition was allowed. The next level augmented up to 7Fr sheaths, and in addition to dual platelet aggregation inhibition, the application of glycoprotein IIb/IIIa inhibitors or the presence of oral anticoagulation was allowed. Patients in whom the highest access site–associated complication rates were expected, including sheath sizes of ≥8Fr and dual platelet aggregation inhibition as well as oral anticoagulation, constituted level 4. If only 1 single criterion of a level was fulfilled, the patient was assigned to the higher level; for example, patients with dual platelet aggregation inhibition as well as oral anticoagulation were assigned to level 4 regardless of the sheath size used.
Sheath removal by the paramedics started with 10 sheath removals in level 1 patients under direct supervision of an experienced physician. Once these 10 removals were successfully completed, the paramedics were allowed to independently perform level 1 patient sheath removals and were eligible for 10 supervised sheath removals in level 2 patients. This approach was repeated at each level, permitting the paramedics to perform increasingly complex sheath removals in patients at higher risk in a stepwise fashion. During the entire study period, the access site was examined before sheath removal and after MC by a physician to ensure successful compression of the puncture site.
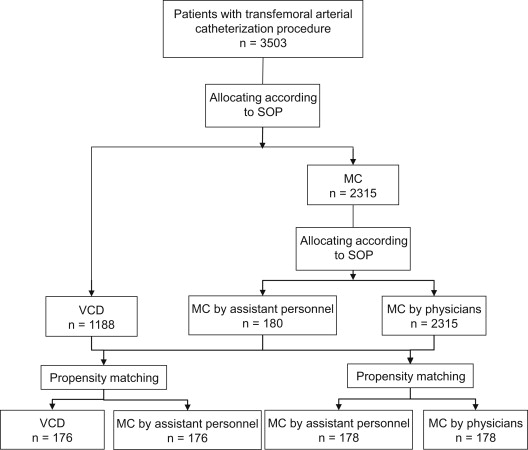
During the whole study period, sheath removal was carried out according to standard operating procedures of the clinic. A flow diagram of access site management is shown in Figure 1 . MC was performed for sheaths ≤5Fr. All sheaths ≥6Fr received VCDs, provided that no contraindications applied. To assess contraindications for VCD insertion, all patients underwent angiographic evaluation of the external iliac, common femoral, and proximal superficial femoral arteries. Contraindications were as follows: (1) site of arteriotomy ≤2 cm proximal to the bifurcation of the common femoral artery, below the femoral bifurcation, or above the inferior epigastric artery; (2) common femoral artery vessel diameter ≤6 mm; (3) extensive calcification or plaque formation in the area of sheath insertion; and (4) extensive scar tissue at the access site. Clinical evaluation of the puncture site was performed before and immediately after sheath removal as well as after removal of the compression bandage. Any changes or abnormalities at the puncture site were reported to a vascular specialist, resulting in vascular ultrasound and/or supplementary examinations such as CT angiography.
The following complications were recorded: bleeding, defined as external blood loss requiring MC; oozing requiring light manual pressure; ecchymosis >5 cm in the soft tissue of the upper thigh; hematoma formation; retroperitoneal extension of hematoma; vessel obstruction or closure; pseudoaneurysm; arteriovenous fistula confirmed by clinical examination, vascular ultrasonography, or computed tomography; infection of the puncture site; a reduction in hemoglobin concentration of ≥30 g/L or a ≥10% decrease in hematocrit; need for blood transfusion; and need for surgery.
Major vascular complications were defined as any of the following: need for surgery, infection requiring intravenous antibiotics or surgical lancing, retroperitoneal hemorrhage, bleeding requiring blood transfusion, pseudoaneurysm, hematoma associated with a decrease in hemoglobin concentration of ≥30 g/L or a ≥10% decrease in hematocrit (according to Thrombolysis In Myocardial Infarction [TIMI] minor bleeding), and postprocedural arteriovenous fistula.
Patient characteristics, anticoagulation medications (heparin, vitamin K antagonists, GPIs, aspirin, thienopyridine), and interventional procedural characteristics (sheath diameter, operator, additional sheaths, and puncture site) were recorded in all patients.
Data were entered and stored in a validated, custom-made database. Statistical analyses were conducted using the R programming language. Continuous variables were checked for normality, and normally distributed variables were compared using Student’s t test and are described as mean ± SD. The median and upper and lower quartiles are reported for continuous variables not normally distributed, and the nonparametric Wilcoxon’s rank-sum test was used. Categorical variables are presented as counts and percentages, and Fisher’s exact test was used. Two-sided p values <0.05 were considered statistically significant. Missing data were imputed using additive regressions, bootstrapping, and predictive mean matching from the Hmisc package in R. We performed propensity score–based matching using the nonrandom package in R. Response data were unbalanced and showed quasi-complete separation, as the number of access site–related complications was zero in the paramedic group. Odds ratios and confidence intervals in this situation were calculated using the logistf package in R, implementing penalized profile likelihood-based estimation of confidence intervals.
Results
Over a period of 8 months, 3,503 cardiac catheterizations with the transfemoral approach were performed. Baseline characteristics and the kind of intervention of the whole study group are listed in Table 1 . Because of the structure of the training program, the paramedics performed MC predominantly in lower risk patients. To adjust the imbalanced distribution of known patient- and procedure-associated risk factors for access site–related vascular complications, propensity score matching was performed ( Table 2 ).
| Variable | MC paramedics (n=180) | MC physicians (n=2135) | p ∗ | VCD (n=1188) | P † |
|---|---|---|---|---|---|
| Age (years) | 67.3 ± 11.9 | 68.6 ± 12.0 | n.s. | 65.9 ± 12.4 | n.s. |
| Women | 71 (39.4%) | 737 (34.5%) | n.s. | 350 (29.5%) | 0.017 |
| Body-Mass-Index (kg/m 2 ) | 28.1 ± 5.1 | 28.3 ± 18.8 | n.s. | 28.1 ± 5.2 | n.s. |
| Systolic blood pressure (mmHg) | 141.4 ± 28.0 | 140.2 ± 28.8 | n.s. | 135.9 ± 27.1 | 0.014 |
| Diastolic blood pressure (mmHg) | 70.4 ± 11.6 | 69.2 ± 13.9 | n.s. | 70.0 ± 14.4 | n.s. |
| Chronic renal insufficiency | 28 (15.5%) | 274 (12.8%) | n.s. | 95 (8.0%) | 0.002 |
| Diabetes mellitus | 47 (26.1%) | 557 (26.1%) | n.s. | 248 (20.9%) | n.s. |
| Warfarin | 25 (13.8%) | 270 (12.6%) | n.s. | 94 (7.9%) | 0.015 |
| Aspirin | 130 (72.2%) | 1641 (76.9%) | n.s. | 991 (83.4%) | <0.001 |
| Clopidogrel | 61 (33.8%) | 1123 (52.6%) | < 0.001 | 789 (66.4%) | <0.001 |
| Glycoprotein IIb/IIIa inhibitors | 4 (2.2%) | 169 (7.9%) | 0.005 | 154 (13.0%) | <0.001 |
| Arterial sheath size ≥7F | 2 (1.1%) | 3 (0.1)% | 0.05 | 3 (0.2%) | n.s. |
| Venous sheath | 46 (25.6)% | 448 (21.0%) | n.s. | 185 (15.6%) | 0.002 |
| Kind of intervention | |||||
| Diagnostic catheterizations | 156 (86.7%) | 1517 (71.1%) | <0.001 | 626 (52.7%) | <0.001 |
| Percutaneous Coronary Intervention | 1 (0.6%) | 232 (10.9%) | <0.001 | 259 (21.8%) | <0.001 |
| Myocardial infarction (Non-ST-Elevation and ST-Elevation) | 9 (5.0%) | 334 (15.6%) | <0.001 | 294 (24.7%) | <0.001 |
| Electrophysiological Study | 14 (7.8%) | 52 (2.4%) | <0.001 | 9 (0.8%) | <0.001 |
∗ MC paramedics vs. MC physicians.
| MC paramedics (n=178) | MC physicians (n=178) | p ∗ | VCD (n=176) | MC paramedics (n=176) | p † | |
|---|---|---|---|---|---|---|
| Age (years) | 67.3 ± 11.9 | 70.0 ± 10.3 | n.s. | 66.4 ± 11.9 | 67.5 ± 11.8 | n.s. |
| Women | 71 (39.9%) | 64 (36.0%) | n.s. | 51 (29.0%) | 66 (37.5%) | n.s. |
| Body-Mass-Index (kg/m 2 ) | 28.1 ± 5.1 | 32.5 ± 6.3 | n.s. | 28.5 ± 5.5 | 28.1 ± 5.1 | n.s. |
| Systolic blood pressure (mmHg) | 141.4 ± 28.0 | 140.9 ± 28.0 | n.s. | 130.4 ± 26.5 | 142.8 ± 27.7 | n.s. |
| Diastolic blood pressure (mmHg) | 70.4 ± 11.6 | 69.3 ± 14.0 | n.s. | 67.8 ± 14.5 | 70.6 ± 11.7 | n.s. |
| Chronic renal insufficiency | 28 (15.7%) | 30 (16.9%) | n.s. | 25 (14.2%) | 28 (15.9%) | n.s. |
| Diabetes mellitus | 47 (26.4%) | 43 (24.2%) | n.s. | 35 (19.9%) | 46 (26.1%) | n.s. |
| Warfarin | 25 (14.0%) | 33 (18.5%) | n.s. | 11 (6.3%) | 18 (10.2%) | n.s. |
| Aspirin | 130 (73.0%) | 121 (68.0%) | n.s. | 144 (81.8%) | 126 (71.6%) | 0.025 |
| Clopidogrel | 61 (34.3%) | 77 (43.3%) | n.s | 137 (77.8%) | 61 (34.7%) | < 0.001 |
| Glycoprotein IIb/IIIa inhibitors | 3 (1.7%) | 4 (2.2%) | n.s | 4 (2.3%) | 3 (1.7%) | n.s. |
| Arterial sheath size ≥7F | 2 (1.1%) | 2 (1.1%) | n.s. | 0 (0.0%) | 2 (1.1%) | n.s. |
| Venous sheath | 46 (25.8%) | 35 (19.7%) | n.s. | 17 (9.7%) | 39 (22.2%) | 0.002 |
| Kind of intervention | ||||||
| Diagnostic catheterizations | 156 (87.6%) | 153 (86.0%) | n.s. | 158 (89.8%) | 156 (88.6%) | n.s. |
| Percutaneous Coronary Intervention | 1 (0.6%) | 2 (1.1%) | n.s. | 3 (1.7%) | 1 (0.6%) | n.s. |
| Myocardial infarction (Non-ST-Elevation and ST-Elevation) | 9 (5.1%) | 13 (7.3%) | n.s. | 8 (4.5%) | 9 (5.1%) | n.s. |
| Electrophysiological Study | 12 (6.7%) | 10 (5.6%) | n.s. | 7 (4.0%) | 10 (5.7%) | n.s. |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


